1. General Information
Welcome to the School of Medical Sciences
Welcome to your Postgraduate Taught Programme in the School of Medical Sciences within the Faculty of Biology, Medicine and Health at the University of Manchester. The University has a worldwide reputation based on high quality teaching and research, and I am sure that your programme will provide a solid foundation for your future career success.
Within the School and the wider Faculty, our goal is to create an environment that allows you to excel and reach your full potential. Offering access to first-class facilities and strong links with regional health-service providers, our postgraduate programmes are designed to meet the diverse needs of all our students. The curriculum of our taught programmes provides the knowledge and skills you will need in your subject area and all our Masters programmes include an opportunity to carry out an independent research project on topics spanning all areas of biomedical research from molecular to experimental biology and clinical medicine. While subject areas cover a broad range, all our taught programmes have two common aims:
- To develop your skills in your chosen field of study
- To enhance your knowledge within the field you have chosen. Whether you are a graduate, professional or have a clinical background, the programmes have been tailored to meet your specific needs.
As a student of the School of Medical Sciences, you will be expected to take responsibility for your degree, within a supportive environment that fosters your development and helps prepare you for your future career. This handbook will be a useful resource as you progress through your programme. It provides programme-specific information that I am sure that you will find helpful throughout your study. If however, you have questions or would like some further advice, please do not hesitate to contact the people listed in this handbook for further information and assistance.
I wish you every success as you embark upon your programme, and in your future career.
Dr Carol Yates
Director of Postgraduate Taught Education
School of Medical Sciences
Faculty of Biology, Medicine and Health
Welcome to the MSc Paediatric Anaesthesia
Welcome to the new taught MSc Paediatric Anaesthesia. Paediatric anaesthesia is an important subspecialty of anaesthesia. Children and infants present unique challenges to anaesthetists, who are involved not only in the delivery of safe anaesthesia but also in peri-operative care, pain management and in the resuscitation and stabilisation of the seriously ill or injured child.
The MSc in Paediatric Anaesthesia is a unique programme, which has been developed in partnership between the University of Manchester and the Department of Paediatric Anaesthesia at the Royal Manchester Children’s Hospital. The programme draws on the high level of knowledge and expertise available at RMCH, and will provide students with the breadth and depth of knowledge and understanding expected from paediatric anaesthetists today.
The MSc is a part-time postgraduate programme, running over three years, making full use of a blended learning approach. It will be flexible enough for full-time professionals to undertake, and will consist of online distance-learning, supplemented by face-to-face study days at the University of Manchester. We offer three exit points – PGCert (1 year), PGDip (2 years), and MSc (3 years).
This academic course, combined with your clinical experience, will enhance your knowledge and enable you to deliver high quality care in the field of paediatric anaesthesia. We wish you every success in this course and in your career.
Dr Jacques Diacono, Programme Director

Dr Victoria Barlow, Programme Director

List of important contacts with e-mail, telephone and location
| Programme Directors: | Dr Jacques Diacono Royal Manchester Childrens Hospital Oxford Road Manchester M13 9WL Tel: 0161 701 1263 jacques.diacono@manchester.ac.uk Dr Victoria Barlow Royal Manchester Childrens Hospital Oxford Road Manchester M13 9WL victoria.barlow-2@manchester.ac.uk |
| Programme Administrator:
MSc Paediatric Anaesthesia Student Representative |
Sarah Watson Programme Administrator School of Medical Sciences, Coupland 3 Building University of Manchester Manchester M13 9PL Tel: (0161) 275 5063 e-mail: paed.anaesthesia@manchester.ac.uk To be appointed by students post registration. The student rep will be nominated from the selection of the students who would like to volunteer for the position. The student rep is required to feedback to the programme directors and administrator on any issues or queries that the students have. They will be required to attend official programme committees throughout the year. |
| eLearning Support: | You can contact eLearning to receive support at elearning@manchester.ac.uk. However, you must enter “FBMH eLearning – MSc Paediatric Anaesthesia” in your email subject header. This will help ensure your request reaches us quickly. Further information on BMH eLearning can be found here. |
| General IT Support: | Contact the Service Desk via the online Knowledge Base http://servicedesk.manchester.ac.uk/portal/ss and report any IT failure or submit a service request. Call the Service Desk on: 0161 306 5544 (or ext 65544). Opening hours are: Monday to Friday 9am to 5pm. |
Online Skills Training Resource
The Faculty has developed a skills training resource to support you through your postgraduate taught programme. This online material should supplement the assessed learning material and activities undertaken in your taught programme.
Accessing the online skills resource
You can access Blackboard through the My Manchester portal (http://my.manchester.ac.uk). The skills training resource is available in an academic community space available to all registered PGT students in the Faculty through Blackboard.
If you cannot see these units in your Blackboard please contact your Programme Administrator.
Content
Full details of all these resources can be found in the introduction to each unit. These resources have been designed to give you formative feedback on your progress through them. If you experience any problems and would like to talk to someone please contact your Programme Director. If you have questions about referencing and how it applies to your own work, please contact your Programme Director or dissertation supervisor/module lead.
| Academic Writing | This is an excellent resource that supports you to write your assignments and dissertation. It is split into units that focus on key areas that previous students have found difficult and aims to enhance your academic writing style. |
| Research Methods* | This course is spilt into 3 units that cover introductions to study design, statistics and dissertation skills. It has a number of online quizzes where you can test your knowledge. |
| Statistics* | The course provides a valuable foundation for understanding and interpreting biostatistics. It aims to provide you with the fundamentals of quantitative analysis. |
| Presentation Skills | This short interactive unit is designed to help you to enhance your presentation skills. Regardless of whether you are presenting in public, preparing for conferences, an oral examination or more informal settings this unit will give you the tops tips to improve your delivery. |
| Qualitative Research Methods* | This unit has been designed to give you an introduction to Qualitative Research. |
| SPSS* | This is an introduction to statistics, using SPSS, a popular and comprehensive data analysis software package containing a multitude of features designed to facilitate the execution of a wide range of statistical analyses. |
| Intellectual Property Awareness Resource | This Intellectual Property (IP) awareness resource has been created in order to improve your understanding of IP. Topics include: Types of intellectual property • Copyright and IP clearance • University policy on IP • IP commercialisation • IP in research or consultancy • IP issues to be aware when dealing with academic materials |
* NOTE: the material in this online resource is for reference and formative learning purposes only. In some of your taught programme you may be required to undertake assessed course units for Research Methods, Qualitative Research or Statistics. If your programme involves taught units then you should refer to the Blackboard material relating to that course unit. Please contact your Programme Administrator if you are unsure which material relates to your assessed work. You will still be able to refer to the online skills resource in later years.
Introductory Courses
All students are automatically enrolled onto a number of introductory course units that provide information on health and safety, academic malpractice and academic literacy. Completion instructions for each of these units are clearly defined within the course. Completion of these units is mandatory for all students. All assessments must be completed as soon as possible after the programme begins, with the academic malpractice assessment completed before the first piece of coursework is submitted. Completion of these units is monitored by the School.
Health and Safety
Before you visit the University campus, please take time to read the University’s Health and Safety Policy. This can be accessed via: http://documents.manchester.ac.uk/display.aspx?DocID=654
Communication with Students
Please note that only Blackboard, the University e-learning platform and your allocated student university email address will be used as official communication by University staff. It is your responsibility to ensure that you can access and read email from this source.
Students are required to keep the University informed of any change to their personal circumstances such as change of name or address. Changes can be recorded by the student via their own personal online record. It is also essential to inform the Programme Administrator if you do not intend to return to the next session of the course, if, for example, you are moving away.
Graduation
All students who successfully complete the Postgraduate Certificate, Diploma and MSc programme are invited, along with their guests, to attend a graduation ceremony. Further details can be accessed via: http://www.manchester.ac.uk/aboutus/dates/graduation
The University of Manchester degree ceremonies are broadcast live online, and are also stored on the University website.
2. Overview of the Programme
This is a part-time programme. The structure of the programme is as follows:
PG Cert Paediatric Anaesthesia (1 yr P/T)
Complete the 4 course units indicated below. These units together contribute 60 credits to the programme.
Course Units
Unit 1: Fundamentals of Epidemiology POPH60991 (15 credits)
Unit 2: Evidence Based Practice POPH60041 (15 credits)
Unit 3: Applied Basic Science in Paediatric Anaesthesia MEDN60041 (15 credits)
Unit 4: Safeguarding Children and Young People; Ethics and Consent MEDN60032 (15 credits)
PG Diploma Paediatric Anaesthesia (2 yrs P/T)
Requires 4 additional units (an additional 60 credits, making a total of 120).
Course Units
Unit 5: Research Methods DENT61010 (15 credits)
Unit 6: Paediatric Anaesthesia for Special Cases MEDN60051 (15 credits)
Unit 7: Trauma and Acute Surgery MEDN60062 (15 credits)
Unit 8: Paediatric Critical Care and Resuscitation Medicine MEDN60072 (15 credits)
MSc Paediatric Anaesthesia (3 yrs P/T)
Under supervision, students will produce a research dissertation (MEDN60080). This will involve identifying research questions, developing the design of a research project, carrying out the research, analysing the data and then writing up the project. This will usually be in the format of a report based dissertation or systematic review. Submission in another format may be permitted by prior approval by the Programme Director.
Progression between stages is subject to satisfactory performance. You will not be able to progress to the dissertation unless you have successfully completed 120 credits at Masters level.
Aims and Learning Outcomes
The Masters programme aims to:
- Develop practical skills in searching for and appraising different sources of evidence and to develop a theoretical understanding of perspectives on evidence-based or evidence-informed practice.
- Allow students to acquire an understanding of basic epidemiological methods for the purpose of participating in the design of epidemiological studies and critically appraising the medical literature.
- Guide students to be able to identify researchable questions, and formulate appropriate research designs and methods.
- Evaluate safeguarding procedures in children, and apply ethical principles when faced with dilemmas surrounding consent, end of life care and children with complex heath needs.
- Give students an in-depth understanding of neonatal and paediatric anatomy, physiology and pharmacology.
- Utilise theoretical knowledge in anatomy, physiology and pharmacology to justify their practical application in general and regional paediatric anaesthesia
- Compare, appraise and justify particular anaesthetic techniques and management plans for special patient circumstances.
- Revise particular pathologies in children and determine specific anaesthetic conditions or recommend specialist input in the perioperative period.
- Formulate management plans for children presenting with major trauma, burns and acute surgical disease requiring operative intervention.
- Justify and choose treatment options when supporting the respiratory; cardiovascular; renal; neurological and immunological systems of neonates and children in the critical care environment.
- Justify and evaluate current resuscitation guidelines in neonates and paediatrics.
Intended Learning Outcomes of the Programme
A. Knowledge & Understanding
At the end of the programme students should be able to:
- Know about different measures of risk, how to calculate them and how this relates to understanding disease causation
- Know about the uses of routine data, screening and epidemiological surveillance
- Critically evaluate the strengths and weaknesses of a range of qualitative, quantitative and mixed research designs, and examine methods of sampling, data collection
- Explore a range of analytic strategies used to handle, interpret and present qualitative and quantitative data
- Develop and apply practical understanding of clinical governance, medicolegal boundaries and regulations
- Summarise the role of the anaesthetist in child protection procedures/examinations
- Describe and justify the procedures surrounding the death of a child
- Evaluate the effects of peripheral and central neuraxial blockade on the anatomy and physiology of the central nervous system in an infant.
- Assess the airway differences in a neonate and the associated pathologies that may influence anaesthetic management.
- Assess children with specific pathologies and conditions to determine an anaesthetic management plan.
- Revise existing knowledge of known circumstances that require specific adaptations to anaesthetic management.
- Summarise the acute physiological changes occurring in trauma and surgery
- Use the available evidence to formulate appropriate treatment plans for common acute surgical problems in the neonate and the older child
- Understand controversies surrounding paediatric trauma management including fluid, blood product and haemostatic agent use
- Evaluate the current treatment strategies for traumatic brain injury in children
- Revise and critique existing neonatal and paediatric resuscitation guidelines.
- Determine management goals/physiological parameters and targets for children requiring intensive care.
B. Intellectual Skills
At the end of the programme students should be able to:
- Outline the advantages and disadvantages of ecological studies, cross-sectional surveys, case-control studies, cohort studies and intervention studies and explain the meaning of bias, confounding and effect modification
- Understand and apply more contemporary approaches to maximise the potential benefit from scientific enquiry, to improve the way in which health care is provided
- Utilise skills in systematic and creative approaches to problem-solving and decision-making in relation to complex issues
- Develop skills in writing and formulating clear and relevant research questions/hypotheses
- Formulate appropriate research questions, objectives and hypotheses; select appropriate designs and methods to answer research questions
- Critically consider how methodological principles should be operationalized in a proposed research study
- Evaluate different ethical analysis tools, and applies these to ethical dilemmas in clinical practice
- Describe the implications of refusal of treatment in paediatric practice
- Use ethical principles when making decisions regarding children with life-limiting conditions, and critique the use of limitation-of-treatment and not-for-resuscitation orders in paediatric practice
- Critically evaluate established fluid management regimes.
- Explain the rationale for dosing muscle relaxants in babies.
- Explain the pharmacology relating to TIVA in small children.
- Recommend and justify difficult airway management strategies in expected and unexpected circumstances.
- Evaluate the need for input from other paediatric specialties.
- Evaluate current trauma care systems and networks
- Evaluate the different imaging modalities in paediatric trauma, and understand the evolution of current protocols
- Recommend and justify inotrope usage in children requiring cardiovascular support.
- Evaluate the need for input from other paediatric specialties.
C. Practical Skills
At the end of the programme students should be able to:
- Calculate incidence and prevalence rates of diseases within a population and be able to perform age standardisation
- Find existing sources of evidence relevant to clinical and non-clinical health questions
- Be able to critically appraise common research designs and assess the published literature.
- Effectively utilise information technology / health informatics
- Write coherent and well-justified research proposals which address problems/issues relevant to health and social care research
- Analyse the process of consent for anaesthesia and surgery in children
- Critically review anaesthetic documents
- Suspect and initiate the diagnostic process of non-accidental injury in children
- Perform central neuraxial blockade, and justify usage of any additives.
- Justify the safe usage of systemic analgesics (paracetamol, opioids) in babies.
- Choose an appropriate anaesthetic technique for children at risk of malignant hyperthermia.
- Compare the existing tools for pain assessment in children
- Develop plans for pain management in children
- Choose appropriate management plans for children with sepsis requiring critical care.
- Compare and choose methods of advanced respiratory support in children with respiratory failure.
D. Transferable Skills and Personal Qualities
At the end of the programme students should be able to:
- Understand how to apply evidence to inform professional practice and decision-making.
- Understand the strengths and limitations of traditional concepts of evidence-based practice and how these relate to their own work or profession.
- Critically reflect on their own academic performance and utilise a range of strategies to improve these and overcome any particular difficulties
- Demonstrate skills in working collegiately and effectively with others as a member of a team
- Further develop and enhance skills in effective communication to a range of audiences in a variety of settings.
- Explain how to deal with complaints in clinical practice
- Evaluate the issues surrounding confidentiality in medicine
- Explain the risks and benefits of local anaesthesia and general anaesthesia in infants to parents.
- Recommend the advantages and disadvantages of central neuraxial blockade versus peripheral nerve blockade.
- Deduce anaesthetic risk from existing paediatric pathologies and explain this to parents (and children as appropriate).
- Agree perioperative management plans with multidisciplinary teams.
- Critique current guidelines and make recommendations for the treatment of multiple trauma, acute haemorrhage, burns, spinal injury and limb trauma
- Explain management plans to parents in an appropriate way.
- Agree intensive care management plans with multidisciplinary teams.
Progression through the Programme
The diagram below shows progression through the programme, related to the semester dates. Students will be required to attend the allocated teaching days and to undertake the associated assessments. Progression from the PG Cert and the PG Dip will be dependent on successful completion of 60 credits, at the required standard. Similarly, progression from PG Dip to the MSc will depend on successful completion of 120 credits, at Masters Level.
|
Semester 1 |
Semester 2 |
On completion |
|
|
Year 1 |
Unit 1 Unit 2 |
Unit 3 Unit 4 |
Exit PG Cert or Progress to PG Dip |
|
Year 2 |
Unit 5 Unit 6 |
Unit 7 Unit 8 |
Exit PG Dip or Progress to MSc |
|
Year 3 |
Dissertation |
Exit MSc |
|
Unit 1: Fundamentals of Epidemiology POPH 60991 (15 Credits)
In this course students will learn about the history of the discipline of epidemiology, as well as its uses in medical research and in informing health policy. Students will be introduced to common types of observational study designs including; ecological studies, cross-sectional surveys, case-control studies, cohort studies and intervention studies. The course covers the appropriate methods of measuring and comparing risk in each type of study as well as the limitations of epidemiological studies and how to minimise systematic errors when conducting their own investigations.
Unit 2: Evidence Based Practice POPH 60041 (15 Credits)
This course will provide practical skills and theoretical understanding to help you develop evidence-informed practice. The first part of the course will develop your skills in identifying your requirements for evidence and how and where to find existing sources of evidence to inform your professional practice. The second part of the course aims to expand thinking beyond previous applications of evidence-based practice, including a re-assessment of the hierarchy of evidence and the application of problem-based practice.
Unit 3: Applied Basic Science in Paediatric Anaesthesia MEDN 60041 (15 Credits)
The unit is intended to give students an in-depth understanding of neonatal and paediatric anatomy, physiology and pharmacology. The unit will allow the student to utilise theoretical knowledge in these areas to justify their practical application in general and regional paediatric anaesthesia.
Students will revise their knowledge of anatomical differences in neonates and young children and use this knowledge to influence their practice in a clinical context, for example management of neonatal airway pathology; inserting invasive lines with appropriate placement and the relevant differences for performing central neuraxial blockade. The students will evaluate and justify the merits of current fluid management strategies in neonates; small children and those with metabolic conditions. The students will appraise the complexities of TIVA (Total IntraVenous Anaesthesia), muscle relaxants, systemic analgesics and local anaesthetic agents and potential additives to support their clinical application.
Unit 4: Safeguarding Children and Young People; Ethics and Consent MEDN 60032 (15 Credits)
This unit will enable students to describe the safeguarding of children, initiate the diagnostic process of non-accidental injury and explain the contribution of the paediatric anaesthetist. They will discuss the ethical principles used when decisions are made in children with life-limiting conditions undergoing surgery or who are acutely unwell. They will also be to analyse the process of consent for anaesthesia and surgery in children, deal with complaints, critically review anaesthetic documents, and describe the processes surrounding death of a child in the emergency department and in the operating theatre.
Unit 5: Research Methods DENT 61010 (15 Credits)
This unit has been developed to provide you with an introduction to research methods, study design and evidence based practice. It includes both practical and theoretical components.
Many of the topics covered in this unit are dealt with briefly and simply. Topics such as ‘Critical appraisal’ and ‘Evidence based practice’ should be a spring board for you to start developing your own skills in this area. Every aspect of your work at Masters level will be underpinned by your ability to understand and evaluate research. The readings and references that you find in this unit are by way of an introduction. In order to obtain the best marks in assignments or dissertations you will be expected to have read more widely than the course materials. We have taken most of our readings from general sources but you may wish to explore more specific texts from your own discipline.
There are also a number of topics that cover more practical issues, such as library skills. Becoming an efficient and effective user of the University Library (whether online or face to face) will greatly enhance all your future studying.
Unit 6: Paediatric Anaesthesia for Special Cases MEDN 60051 (15 Credits)
The unit is designed to compare, appraise and justify particular anaesthetic techniques and management plans for special patient circumstances, for example difficult airway management in patients with mucopolysaccharidosis or Pierre-Robin sequence. The unit will get the students to revise particular pathologies in children and determine specific anaesthetic conditions or recommend specialist input in the perioperative period.
The unit will explore difficult airway management in children with existing conditions that likely to cause concern to the paediatric anaesthetist. In particular the unit will discuss the anaesthetic management of mucopolysaccharidosis; explore the associated conditions likely to require anaesthetic intervention and explain the concerns and risks to the child’s parents.
The unit will assess the anaesthetic management of known patient and familial conditions that may influence the choice of anaesthetic technique such as Duchenne’s muscular dystrophy, central core disease and malignant hyperthermia. The unit will examine metabolic conditions such as MCADD (Medium-chain acyl-coenzyme A dehydrogenase deficiency) and justify perioperative fluid management plans.
Other conditions included are Congenital HyperInsulinism (CHI) and Cockayne syndrome.
Unit 7: Trauma and Acute Surgery MEDN 60062 (15 Credits)
The unit will enable students to critique current guidelines, weight the available evidence, and make recommendations for the management of multiple trauma, acute haemorrhage, burns, head injury, spinal injury and limb trauma. They will be able to understand the common acute surgical problems in the neonate and the older child, and be able to evaluate the various treatment strategies and develop the most appropriate treatment plan. They must be able to compare the different tools for pain assessment in infants and children, and judge which are the most appropriate. They will ultimately be able to make recommendations for pain management in trauma and postoperatively.
Unit 8: Paediatric Critical Care and Resuscitation Medicine MEDN 60072 (15 Credits)
The unit is designed to enable the students to justify and choose treatment options when supporting the respiratory; cardiovascular; renal; neurological and immunological systems of neonates and children in the critical care environment. The unit will examine management techniques in neonatal intensive care for term and premature babies. The unit will get the students to justify and evaluate current resuscitation guidelines in neonates and paediatrics.
The unit will explore advanced respiratory organ support including high frequency oscillation and ECMO (extracorporeal membrane oxygenation) and their particular indications. The unit will get the students to explain and justify inotrope usage in neonates and children with cardiovascular collapse.
The unit will revise current resuscitation guidance and enable the students to critique the evidence for recommended management at birth (eg delayed cord clamping, oxygen concentration used) and for cooling to prevent brain injury. The unit will examine management strategies employed on the neonatal unit such as the use of xenon in hypoxic ischaemic encephalopathy and treatment of meconium aspiration.
The unit will look at the importance of goal directed therapy for children with sepsis.
MSc Dissertation MEDN 60080 (60 credits)
Under supervision, students will produce a research dissertation. This will involve identifying research questions, developing the design of a research project, carrying out the research, analysing the data and then writing up the project. This will usually be in the format of a report based dissertation or systematic review. Submission in another format may be permitted by prior approval by the programme director.
Course Unit Outlines
Course Unit 1: Fundamentals of Epidemiology
Unit Coordinator: Islay Gemmell
1. COURSE UNIT OVERVIEW
In this course students will learn about the history of the discipline of epidemiology, as well as its uses in medical research and in informing health policy. Students will be introduced to common types of observational study designs including; ecological studies, cross-sectional surveys, case-control studies, cohort studies and intervention studies. The course covers the appropriate methods of measuring and comparing risk in each type of study as well as the limitations of epidemiological studies and how to minimise systematic errors when conducting their own investigations.
2. AIMS
The aim of this course is for students to acquire an understanding of basic epidemiological methods for the purpose of participating in the design of epidemiological studies and critically appraising the medical literature.
3. LEARNING OUTCOMES
On completion of this unit successful students will be able to:
• Summarise the uses of epidemiology in research and practice
• Know about different measures of risk, how to calculate them and how this relates to understanding disease causation
• Calculate incidence and prevalence rates of diseases within a population
• Outline the advantages and disadvantages of ecological studies, cross-sectional surveys, case-control studies, cohort studies and intervention studies
• Explain the meaning of bias, confounding and effect modification
• Be able to perform age standardisation
• Know about the uses of routine data, screening and epidemiological surveillance
4. EMPLOYABILITY SKILLS
Analytical Skills
Students will develop analytical skills by learning about the strengths and limitations of common types of observational study designs such as ecological studies, cross-sectional surveys, case-control studies, cohort studies and intervention studies. They will learn how to critically appraise these studies in the medical literature.
Research
In this module students will develop research skills by learning how to choose the appropriate epidemiological study design to use to answer particular research questions. They will also learn how to analyse data collected in epidemiological studies and how to interpret epidemiological data.
5. TEACHING AND LEARNING METHODS
Online distance learning with course materials provided via the virtual learning environment Blackboard. The course consists of 10 weekly topics with links to external web materials and reference to reading materials. There are also tasks that require students to participate in group discussions – these discussions will be conducted on the online discussion board and moderated by the course unit leader and teaching assistant. At the end of most topics there is a self-test which provides a more in-depth test of students’ understanding of the course material and a guide to the type of question that can be expected in the marked assignment. Automated feedback is provided for the self-tests.
6. ASSESSMENT METHODS
• Mid semester assignment (30%)
• End semester assignment (70%)
7. FEEDBACK METHODS
Students will be provided with personalised feedback for their mid-term and final summative assignments, within 15 working days for mid-term assignments and 20 working days for final submission.
Further opportunities for formative feedback (on non-assessed work) will also be provided during a course unit.
Course Unit 2: Evidence Based Practice
Unit Coordinator: Arpana Verma
1. COURSE UNIT OVERVIEW
This course will provide practical skills and theoretical understanding to help you develop evidence-informed practice. The first part of the course will develop your skills in identifying your requirements for evidence and how and where to find existing sources of evidence to inform your professional practice. The second part of the course aims to expand thinking beyond previous applications of evidence-based practice, including a re-assessment of the hierarchy of evidence and the application of problem-based practice.
2. AIMS
To develop practical skills in searching for and appraising different sources of evidence and a theoretical understanding of perspectives on evidence-based or evidence-informed practice.
3. LEARNING OUTCOMES
On completion of this unit, successful students will be able to:
• Find existing sources of evidence relevant to clinical and non-clinical health questions.
• Be able to critically appraise common research designs and assess the published literature.
• Understand how to apply evidence to inform professional practice and decision making.
• Understand the strengths and limitations of traditional concepts of evidence-based practice and how these relate to their own work or profession.
• Understand and apply more contemporary approaches to maximise the potential benefit from scientific enquiry, to improve the way in which health care is provided.
4. EMPLOYABILITY SKILLS
Analytical Skills
Students will be expected to demonstrate an ability search for and analyse the relevance of articles and journals to current evidence based practice.
Innovation/Creativity
Students will be able to identify new opportunities, generate solutions, make improvements and to think creatively and enterprisingly in order to evaluate previous applications of evidence-based practice.
Problem Solving
Students will need to evaluate current practice to demonstrate the ability to apply a logical approach to be able to re-assess the hierarchy of evidence and the application of problem-based practice.
Written Communication
Students will need to be able to communicate their arguments coherently in the assignment questions demonstrating literacy and a strong command of the English language. Students will also be encouraged able to share their experiences and public health anecdotes through social media such as the MPH blog. http://blogs.mhs.manchester.ac.uk/mphblog/
5. SYLLABUS
• Introduction to evidence based practice
• Defining the research question
• Finding the evidence
• Appraising the evidence
• Revisiting approaches to evidence based practice
• Critical perspectives on evidence based practice
• Evidence based practice in action
• How to incorporate the ideals of evidence based practice into contemporary ways of working
6. TEACHING AND LEARNING METHODS
This course involves working through the course notes provided online, linked references and other online sources of information. You will be encouraged to use self-reflection to help you think about the ideas discussed, and take part in discussion board activities. You will be required to develop skills in searching for published literature using electronic databases as part of the course. You should work through the unit in a logical sequence. The calendar in Blackboard will guide you as to what you should be doing and when. It is essential you follow this guidance so that you are doing the same topic at the same time as your fellow students. Participation in the discussion boards and Blogs is greatly encouraged, and generally those students who do participate do better in their assignments.
7. ASSESSMENT METHODS
• Mid-semester assignment (50%) – 2000 words
• End of semester assignment (50%) – 2000 words
8. FEEDBACK METHODS
Students will be provided with personalised feedback for their mid-term and final summative assignments, within 15 working days for mid-term assignments and 20 working days for final submission.
Further opportunities for formative feedback (on non-assessed work) will also be provided during a course unit.
Course Unit 3: Applied Basic Science in Paediatric Anaesthesia
Unit Coordinators: Jacques Diacono and Victoria Barlow
1. COURSE UNIT OVERVIEW
Students will revise their knowledge of anatomical differences in neonates and young children and use this knowledge to influence their practice in a clinical context, for example management of neonatal airway pathology; inserting invasive lines with appropriate placement and the relevant differences for performing central neuraxial blockade. The students will evaluate and justify the merits of current fluid management strategies in neonates; small children and those with metabolic conditions. The students will appraise the complexities of TIVA (Total IntraVenous Anaesthesia), muscle relaxants, systemic analgesics and local anaesthetic agents and potential additives to support their clinical application.
2. AIMS
The unit is intended to give students an in-depth understanding of neonatal and paediatric anatomy, physiology and pharmacology. The unit will allow the students to utilise theoretical knowledge in these areas to justify their practical application in general and regional anaesthesia.
3. LEARNING OUTCOMES
Knowledge and Understanding
• Evaluate the effects of peripheral and central neuraxial blockade on the anatomy and physiology of the central nervous system in a baby.
• Assess the airway differences in a neonate and the associated pathologies that may influence anaesthetic management.
Intellectual Skills
• Critically evaluate established fluid management regimes.
• Explain the rationale for dosing muscle relaxants in babies.
• Explain the pharmacology relating to TIVA in small children.
Practical Skills
• Perform central neuraxial blockade, and justify usage of any additives.
• Justify the safe usage of systemic analgesics (paracetamol, opioids) in babies.
Transferable Skills and Personal Qualities
• Explain the risks and benefits of local anaesthesia and general anaesthesia in babies to parents.
• Recommend the advantages and disadvantages of central neuraxial blockade versus peripheral nerve blockade.
4. TEACHING AND LEARNING METHODS
• Online discussions on weekly cases
• Seminars and lectures during contact days
• Assignments
• Additional reading
5. ASSESSMENT METHODS
• Mid-semester assignment (50%) – powerpoint presentation 30 slides
• End of semester assignment (50%) – 1500 words
• Participation in online discussions – formative
6. FEEDBACK METHODS
Students will receive personalised feedback within 15 working days.
7. INDICATIVE READING LIST
• Smith’s Anesthesia for Infants and Children (9th Edition), Davis & Cladis, Elsevier.
• FDA Drug Safety Communication for General Anaesthetic and Sedation Drugs
www.fda.gov/Drugs/DrugSafety/ucm532356.htm
• Joint professional guidance on the use of general anaesthesia in young children, Association of Paediatric Anaesthetists of Great Britain and Ireland, April 2017. http://www.apagbi.org.uk/sites/default/files/imagecache/Joint%20Professional%20Guidance%20on%20the%20use%20of%20general%20anaesthesia%20in%20young.pdf
• Association of Paediatric Anaesthetists CONSENSUS GUIDELINE ON PERIOPERATIVE FLUID MANAGEMENT IN CHILDREN v 1.1 September 2007 http://www.apagbi.org.uk/sites/default/files/Perioperative_Fluid_Management_2007.pdf
Course Unit 4: Safeguarding Children and Young People; Ethics and Consent
Unit Coordinators: Jacques Diacono and Victoria Barlow
1. COURSE UNIT OVERVIEW
The unit will enable students to describe the safeguarding of children, initiate the diagnostic process of non-accidental injury and explain the contribution of the paediatric anaesthetist. They will discuss the ethical principles used when decisions are made in children with life-limiting conditions undergoing surgery or who are acutely unwell. They will also be able to analyse the process of consent for anaesthesia and surgery in children, deal with complaints, critically review anaesthetic documents, and describe the processes surrounding death of a child in the emergency department and in the operating theatre.
2. AIMS
The unit will enable students to evaluate safeguarding procedures in children, and apply ethical principles when faced with dilemmas surrounding consent, end of life care and children with complex heath needs.
3. LEARNING OUTCOMES
Knowledge and Understanding
• Summarise the role of the anaesthetist in child protection procedures/examinations
• Describe and justify the procedures surrounding the death of a child
• Critique the use of limitation-of-treatment and not-for-resuscitation orders in paediatric practice
Intellectual Skills
• Evaluate different ethical analysis tools, and applies these to ethical dilemmas in clinical practice
• Describe the implications of refusal of treatment in paediatric practice
• Use ethical principles when making decisions regarding children with life-limiting conditions
Practical Skills
• Analyse the process of consent for anaesthesia and surgery in children
• Critically review anaesthetic documents
• Suspect and initiate the diagnostic process of non-accidental injury in children
Transferable Skills and Personal Qualities
• Explain how to deal with complaints in clinical practice
• Evaluate the issues surrounding confidentiality in medicine
4. TEACHING AND LEARNING METHODS
• Online discussions on weekly cases
• Seminars and lectures during contact days
• Assignments
• Additional reading
5. ASSESSMENT METHODS
• Mid-semester assignment (50%) – powerpoint presentation 30 slides
• End of semester assignment (50%) – 1500 words
• Participation in online discussions – formative
6. FEEDBACK METHODS
Students will receive personalised feedback within 15 working days.
7. INDICATIVE READING LIST
- Child protection and the anaesthetist: safeguarding children in the operating theatre 2014 https://www.rcoa.ac.uk/node/17805
- Consent for anaesthesia 2017 https://www.aagbi.org/sites/default/files/AAGBI_Consent_for_anaesthesia_2017_0.pdf
- DNAR decisions in the Perioperative period https://www.aagbi.org/sites/default/files/dnar_09_0.pdf
- Making decisions to limit treatment in life-limiting and life-threatening conditions in children:
- a framework for practice http://adc.bmj.com/content/100/Suppl_2/s1.full.pdf+html
- Online course – Safeguarding children levels 1, 2, and 3 http://www.e-lfh.org.uk/programmes/safeguarding-children/
Course Unit 5: Research Methods
Unit Coordinator: Juliette Kendall and Anne-Marie Glenny
1. COURSE UNIT OVERVIEW
On behalf of Dentistry and the Faculty of Biology, Medicine and Health, we are delighted to welcome you to this new unit.
This unit has been developed to provide you with an introduction to research methods, study design and evidence based practice. It includes both practical and theoretical components. This year students from a number of different disciplines, such as Dentistry, Public health, Primary care and Medical Education will be taking this unit. For all of you we hope that this unit will provide a valuable foundation of study skills and tools which will play a vital role in helping you develop research and critical evaluation skills necessary for your assignment preparation and dissertation writing. Depending on your programmes others of you will go on to study aspects of epidemiology and biostatistics in more depth.
Many of the topics covered in this unit are dealt with briefly and simply. Our aim in this unit is to introduce you to new ideas and concepts. Topics such as ‘Critical appraisal’ and ‘Evidence based practice’ should be a spring board for you to start developing your own skills in this area. Every aspect of your work at Masters level will be underpinned by your ability to understand and evaluate research. The readings and references that you find in this unit are by way of an introduction. In order to obtain the best marks in assignments or dissertations you will be expected to have read more widely than the course materials. We have taken most of our readings from general sources but you may wish to explore more specific texts from your own discipline.
There are also a number of topics that cover more practical issues, such as library skills. Becoming an efficient and effective user of the University Library (whether online or face to face) will greatly enhance all your future studying.
2. AIMS
This unit will produce students who are competent in issues related to the design, execution and interpretation of clinical and clinically-related research. The latter may include medical education, public health and basic-science areas such as genetics, microbiology or biomaterials. It will also provide students with critical appraisal skills so that on a life-long basis they will be able to apply these skills to assess any research evidence that comes before them.
3. LEARNING OUTCOMES
- Understand key epidemiological concepts.
- Understand the structure of, and be able to differentiate between, the common types of epidemiological studies.
- Identify different types of data.
- Understand basic statistical issues needed for the development of a study protocol.
- Understand the key issues to consider when critically appraising different study designs.
- Understand key ethics and research governance documents and legislation, such as the Helsinki Declaration, and legislation such as the UK Data Protection Act.
- Understand procedures relating to obtaining ethical approval for your research, using the UK NHS Ethics Committee system as an example.
- Define evidence based practice and recognise the keys steps involved in its practice.
- Recognise the role of secondary research in EBP (including systematic reviews and clinical guidelines).
- Discuss the role of research in a clinical discipline.
- Explore the development of a research idea from hypothesis through to the drawing of conclusions.
- Make a judgement on the quality of a research article with consideration of implications for clinical practice/future research.
- Discuss issues regarding the implementation of research findings.
4. TEACHING AND LEARNING METHODS
The course will be delivered predominantly through our e-learning platform. A variety of online material will be utilised, including web-based reading, audio presentations, online discussions, tutor feedback, interactive group exercises, self-assessment through multiple choice questionnaires and self-reflection.
Some programmes will also run face-to-face symposiums with a mix of tutor presentations, group work and student presentations. These are open to all students; however no new material will be covered at the events and students not able to attend will not be penalised in any way.
5. ASSESSMENT METHODS
• Mid-semester assignment (35%) – 1500 words
• End of semester assignment (60%) – 2500 words
• Participation in online discussions (5%) – 1 small group task
6. FEEDBACK METHODS
Students will receive personalised feedback within 20 working days.
Course Unit 6: Paediatric Anaesthesia for Special Cases
Unit Coordinators: Jacques Diacono and Victoria Barlow
1. COURSE UNIT OVERVIEW
The unit will explore difficult airway management in children with existing conditions that likely to cause concern to the paediatric anaesthetist. In particular the unit will discuss the anaesthetic management of mucopolysaccharidosis; explore the associated conditions likely to require anaesthetic intervention and explain the concerns and risks to the child’s parents.
The unit will assess the anaesthetic management of known patient and familial conditions that may influence the choice of anaesthetic technique such as Duchenne’s muscular dystrophy, central core disease and malignant hyperthermia. The unit will examine metabolic conditions such as MCADD (Medium-chain acyl-coenzyme A dehydrogenase deficiency) and justify perioperative fluid management plans.
Other conditions included are Congenital HyperInsulinism (CHI) and Cockayne syndrome.
2. AIMS
The unit is designed to compare, appraise and justify particular anaesthetic techniques and management plans for special patient circumstances, for example difficult airway management in patients with mucopolysaccharidosis or Pierre-Robin sequence. The unit will get the students to revise particular pathologies in children and determine specific anaesthetic conditions or recommend specialist input in the perioperative period.
3. LEARNING OUTCOMES
Knowledge and Understanding
• Assess children with specific pathologies and conditions to determine an anaesthetic management plan.
• Revise existing knowledge of known circumstances that require specific adaptations to anaesthetic management.
Intellectual Skills
• Recommend and justify difficult airway management strategies in expected and unexpected circumstances.
• Evaluate the need for input from other paediatric specialties.
Practical Skills
• Choose an appropriate anaesthetic technique for children at risk of malignant hyperthermia.
Transferable Skills and Personal Qualities
• Deduce anaesthetic risk from existing paediatric pathologies and explain this to parents (and children as appropriate).
• Agree perioperative management plans with multidisciplinary teams.
4. TEACHING AND LEARNING METHODS
• Online discussions on weekly cases
• Seminars and lectures during contact days
• Assignments
• Additional reading
5. ASSESSMENT METHODS
• Mid-semester assignment (50%) – powerpoint presentation 30 slides
• End of semester assignment (50%) – 1500 words
• Participation in online discussions – formative
6. FEEDBACK METHODS
Students will receive personalised feedback within 15 working days.
7. INDICATIVE READING LIST
• Smith’s Anesthesia for Infants and Children (9th Edition), Davis & Cladis, Elsevier.
• Paediatric Difficult Airway Guidelines, Difficult Airway Society and Association of Paediatric Anaesthetists, 2015
• https://www.das.uk.com/guidelines/paediatric-difficult-airway-guidelines
• Anaesthesia and airway management in mucopolysaccharidosis. Walker, R et al J Inherit Metab Dis. 2013 Mar;36(2):211-9.
Course Unit 7: Trauma and Acute Surgery
Unit Coordinators: Jacques Diacono and Victoria Barlow
1. COURSE UNIT OVERVIEW
Students will be able to critique current guidelines, weight the available evidence, and make recommendations for the management of multiple trauma, acute haemorrhage, burns, head injury, spinal injury and limb trauma. They will be able to understand the common acute surgical problems in the neonate and the older child, and be able to evaluate the various treatment strategies and develop the most appropriate treatment plan. They must be able to compare the different tools for pain assessment in infants and children, and judge which are the most appropriate. They will ultimately be able to make recommendations for pain management in trauma and postoperatively.
2. AIMS
The unit will enable students to formulate management plans for children presenting with major trauma, burns and acute surgical disease requiring operative intervention.
3. LEARNING OUTCOMES
Knowledge and Understanding
• Summarise the acute physiological changes occurring in trauma and surgery
• Understand controversies surrounding paediatric trauma management including fluid, blood product and haemostatic agent use
• Evaluate the current treatment strategies for traumatic brain injury in children
• Evaluate the different imaging modalities in paediatric trauma, and understand the evolution of current protocols
• Use the available evidence to formulate appropriate treatment plans for common acute surgical problems in the neonate and the older child
Intellectual Skills
• Evaluate current trauma care systems and networks
Practical Skills
• Compare the existing tools for pain assessment in children
• Develop plans for pain management in children
Transferable Skills and Personal Qualities
• Critique current guidelines and make recommendations for the treatment of multiple trauma, acute haemorrhage, burns, spinal injury and limb trauma
4. TEACHING AND LEARNING METHODS
• Online discussions on weekly cases
• Seminars and lectures during contact days
• Assignments
• Additional reading
5. ASSESSMENT METHODS
• Mid-semester assignment (50%) – powerpoint presentation 30 slides
• End of semester assignment (50%) – 1500 words
• Participation in online discussions – formative
6. FEEDBACK METHODS
Students will receive personalised feedback within 15 working days.
7. INDICATIVE READING LIST
• Advanced Paediatric Life Support: A Practical Approach to Emergencies (Advanced Life Support Group) Paperback – 15 Apr 2016 by Advanced Life Support Group
• Smith’s Anesthesia for Infants and Children. 9th Edition. Authors: Peter Davis Franklyn Cladis
• Paediatric Trauma Protocol – Royal College of Radiologists https://www.rcr.ac.uk/system/files/publication/field_publication_files/BFCR(14)8_paeds_trauma.pdf
Course Unit 8: Paediatric Critical Care and Resuscitation Medicine
Unit Coordinators: Jacques Diacono and Victoria Barlow
1. COURSE UNIT OVERVIEW
The unit will explore advanced respiratory organ support including high frequency oscillation and ECMO (extracorporeal membrane oxygenation) and their particular indications. The unit will get the students to explain and justify inotrope usage in neonates and children with cardiovascular collapse.
The unit will revise current resuscitation guidance and enable the students to critique the evidence for recommended management at birth (eg delayed cord clamping, oxygen concentration used) and for cooling to prevent brain injury. The unit will examine management strategies employed on the neonatal unit such as the use of xenon in hypoxic ischaemic encephalopathy and treatment of meconium aspiration.
The unit will look at the importance of goal directed therapy for children with sepsis.
2. AIMS
The unit is designed to enable the students to justify and choose treatment options when supporting the respiratory; cardiovascular; renal; neurological and immunological systems of neonates and children in the critical care environment. The unit will examine management techniques in neonatal intensive care for term and premature babies. The unit will get the students to justify and evaluate current resuscitation guidelines in neonates and paediatrics.
3. LEARNING OUTCOMES
Knowledge and Understanding
• Revise and critique existing neonatal and paediatric resuscitation guidelines.
• Determine management goals/physiological parameters and targets for children requiring intensive care.
Intellectual Skills
• Recommend and justify inotrope usage in children requiring cardiovascular support.
• Evaluate the need for input from other paediatric specialties.
Practical Skills
• Choose appropriate management plans for children with sepsis requiring critical care.
• Compare and choose methods of advanced respiratory support in children with respiratory failure.
Transferable Skills and Personal Qualities
• Explain management plans to parents in an appropriate way.
• Agree intensive care management plans with multidisciplinary teams.
4. TEACHING AND LEARNING METHODS
• Online discussions on weekly cases
• Seminars and lectures during contact days
• Assignments
• Additional reading
5. ASSESSMENT METHODS
• Mid-semester assignment (50%) – powerpoint presentation 30 slides
• End of semester assignment (50%) – 1500 words
• Participation in online discussions – formative
6. FEEDBACK METHODS
Students will receive personalised feedback within 15 working days.
7. INDICATIVE READING LIST
• The UK collaborative randomised Trial of Neonatal ECMO. Lancet 1996;348:75-82
• Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes McDonald SJ, Middleton P, Dowswell T, Morris PS.Cochrane Database of Systematic Reviews. 2013; Issue 7. Art. No.: CD004074
• Advanced Paediatric Life Support: A Practical Approach to Emergencies (APLS) 6th Edition 2016, Wiley-Blackwell
• Resuscitation and support of transition of babies at birth, Resuscitation Council UK 2015 https://www.resus.org.uk/resuscitation-guidelines/resuscitation-and-support-of-transition-of-babies-at-birth/
3. Teaching, Learning and Assessment
Coursework and Assessment
Assessment will take place through coursework, for which there are 3 elements:
1. Participation in the Discussion Board
2. Unit Assignments
3. Dissertation
Each unit is assessed as a discrete entity, resulting in a final mark for that individual unit. At the end of the academic years 1 and 2, students will have final marks for the 4 individual units, each of which will be considered by the Board of Examiners in August.
Discussion Board
Individuals will be given the opportunity to participate in the online discussions, and this forms part of continuous development. Students must engage in at least 80% of the questions posted on Blackboard.
Unit Assignments
There will be two assignments per unit. They will generally be in the form of PowerPoint presentation or a short discursive essay.
Dissertation
(see separate dissertation handbook)
Please refer to your Blackboard unit spaces for more information regarding coursework and assessment, including submission deadlines: https://my.manchester.ac.uk/
Research Projects
In the final year, each student will submit a written dissertation in the format of a report based dissertation or systematic review. Submission in another format may be permitted by prior approval by the programme director.
Postgraduate Taught Degree Regulations for Students
Postgraduate Taught degrees at the University of Manchester are based on the National Framework for Higher Education Qualifications (FHEQ). This framework requires students to achieve credit at masters’ level in order to get an award. For a standard postgraduate taught Masters programme this will normally mean passing 180 credits. A standard postgraduate diploma will normally have 120 credits and a postgraduate certificate 60 credits. The way in which you study these credits will be defined later in the programme handbook and the programme specification.
The University sets standards relating to your performance on every unit but also on your progression through the programme. The programme and course unit specifications will set out the requirements for passing the credit on individual units.
Postgraduate Taught Degree Regulations
Please find below the link to the degree regulations:
Postgraduate Taught Degree Regulations (for new PGT students registering from September 2016)
The following guidance should be read in conjunction with the Introduction to the Postgraduate Degree Regulations for Students:
http://www.tlso.manchester.ac.uk/degree-regulations/
Criteria for Awards
Award of Masters Degree
The award of Master degree is based upon credit accumulation using a pass mark of 50%.
Distinction
Exceptional achievements over the course of the Programme according to the taught masters marking scheme will be rewarded with the degree of Masters with Distinction.
To obtain a Distinction, students must have:
- accrued 180 credits;
- have passed all units with no compensations or referrals;
- have achieved an overall weighted average of 70% or more across the programme;
Students who have compensated or have been referred in any course units are not eligible for the award of Distinction. In addition, the dissertation must be submitted by the end of the period of programme, unless there are significant mitigating circumstances, approved in advance for missing the end of programme deadline.
Merit
To obtain a Merit, students must have accrued 180 credits AND have achieved an overall weighted average of 60% or more across the programme, including any provision made for compensated or referred units.
Pass
To obtain a pass, students must have accrued 180 credits including any provision made for compensated or referred units.
Progression
To progress to the dissertation / research element of the Masters programme, students must have passed all taught units (120 credits).
Award Postgraduate Diploma
To obtain a Postgraduate Diploma award, students must have accrued 120 credits (as specified by the programme) including any provision made for compensated or referred units.
Award Postgraduate Certificate
To obtain a Postgraduate Certificate award students must have accrued 60 credits (as specified by the programme) including any provision made for compensated or referred units.
Unless otherwise specified in the exemptions, the awards of Postgraduate Diploma and Postgraduate Certificate degree are based upon credit accumulation using a pass mark of 40% for which there is no classification other than pass/fail.
Exit Awards
Exit awards are available for students who do not satisfy the criteria for the programme they are registered on or who needs to exit the programme early due to unforeseen circumstances.
To be considered for a PG Diploma (120 credits; exit point) students must have accrued 120 credits across the programme.
To be considered for a PG Certificate (60 credits; exit point) students must have accrued 60 credits across the programme.
Please note the pass mark for course units making up the Postgraduate Diploma and Certificate exit awards is 40%.
Compensation
Masters Degree
Students may be awarded compensated credit if they receive fail marks in the range 40‑49% in no more than 30 credits in the taught component.
Postgraduate Diploma
Students may be awarded compensated credit if they receive fail marks in the range 30‑39% in no more than 30 credits in the taught component.
Postgraduate Certificate
Students may be awarded compensated credit if they receive fail marks in the range 30‑39% in no more than 15 credits in the taught component.
The combined total number of credits compensated and referred cannot exceed half the taught credits.
Compensated credit retains the original failed mark for the course unit and this is used in the weighted average for the calculation of the final classification/award.
Please note that some programmes do not allow compensation. Please refer to the ‘Programme Exemptions to PGT Degree Regulations’ section of the handbook where specific exemptions applicable to the programme will be listed.
Reassessment
Where the overall unit mark is below the compensation zone (40% for Masters and 30% for Postgraduate Diploma/Certificate) OR the number of compensatable fails (30 credits for Masters/Diploma and 15 credits for Postgraduate Certificate) has been exceeded, reassessment may be taken.
Reassessment as a result of a fail is known as a “Referral”. Reassessment as a result of approved and verified mitigating circumstances is known as “Deferral” and may be permitted where students are reassessed as a first attempt, for which no penalty applies.
Students may be referred in up to half of the total taught credits. The combined total number of credits referred and compensated cannot exceed half the taught credits. Decisions with regard to which components should be reassessed are made by the Examination Board. When a student is referred they will normally be permitted to retake the assessment/exam on one further occasion.
At the recommendation of the Board of Examiners, students will normally be allowed one resubmission of a failed dissertation or project and this will normally be within four months of the date of the publication of the result. For September 2016 starters only, failed PGT dissertations can only be re-submitted if they achieve a mark of 30 or above. The Board of Examiners, in agreement with the External Examiner may, exceptionally, decide not to allow resubmission.
The pass mark for a reassessment is the same as the first attempt (i.e. 50% for masters and 40% for Postgraduate Diploma/Certificate).When a reassessment is passed, the mark is capped at the lowest compensatable fail mark (i.e. 40R for Masters and 30R for Postgraduate Diploma/Certificate), unless the previous mark was within the compensation zone, in which case the original mark will stand with a suffix ‘R’. This mark is used in the weighted average/total mark for the final award. The capped mark is applied to the whole unit and not the failed component.
Referrals may also be compensated providing the number of quota of compensations has not been exceeded. When a student’s referral mark is in the compensation zone (and the student/unit is eligible for compensation), the student’s mark will be capped at the lowest compensatable fail mark (i.e. 40R for Masters and 30R for Postgraduate Diploma/Certificate).
Please note that some programmes do not allow referrals. Please refer to the ‘Programme Exemptions to PGT Degree Regulations’ section of the handbook where specific exemptions applicable to the programme will be listed.
Guidance for Presentation of Taught Masters Dissertations
The University of Manchester guidance on presentation of taught Masters Dissertations is available at:
Guidance for the presentation of Taught Masters dissertations
The guidance explains the required presentation of the dissertation, and failure to follow the instructions in the guidance may result in the dissertation being rejected by the examiners.
Turnitin and Plagiarism
Plagiarism and Other Forms of Academic Malpractice
Academic malpractice is any activity - intentional or otherwise - that is likely to undermine the integrity essential to scholarship and research. It includes plagiarism, collusion, fabrication or falsification of results, and anything else that could result in unearned or undeserved credit for those committing it. Academic malpractice can result from a deliberate act of cheating or may be committed unintentionally. Whether intended or not, all incidents of academic malpractice will be treated seriously by the University.
The Faculty of Biology Medicine and Health have designed a learning module to raise your awareness of academic malpractice and how it can occur in general writing during your studies. This resource can be accessed via Blackboard - SMS Introductory Course and must be completed before you submit your first piece of academic writing for assessment.
The University provides workshops and online training via My Learning Essentials: http://www.library.manchester.ac.uk/using-the-library/students/training-and-skills-support/my-learning-essentials/
University of Manchester guidance to students on plagiarism and other forms of academic malpractice is available at:
http://www.regulations.manchester.ac.uk/guidance-to-students-on-plagiarism-and-other-forms-of-academic-malpractice/
The full guidance document can be viewed here: http://documents.manchester.ac.uk/display.aspx?DocID=2870
Academic Malpractice: Procedure for the Handling of Cases can be found at: http://documents.manchester.ac.uk/DocuInfo.aspx?DocID=639
Turnitin
The University uses electronic systems for the purposes of detecting plagiarism and other forms of academic malpractice and for marking. Such systems include TurnitinUK, the plagiarism detection service used by the University.
As part of the formative and/or summative assessment process, you may be asked to submit electronic versions of your work to TurnitinUK and/or other electronic systems used by the University (this requirement may be in addition to a requirement to submit a paper copy of your work). If you are asked to do this, you must do so within the required timescales.
The School also reserves the right to submit work handed in by you for formative or summative assessment to TurnitinUK and/or other electronic systems used by the University.
Please note that when work is submitted to the relevant electronic systems, it may be copied and then stored in a database to allow appropriate checks to be made.
Mitigating Circumstances
Mitigating circumstances are personal or medical circumstances which are unforeseeable and unpreventable that could have a significant adverse effect on your academic performance. You should only submit a mitigating circumstances application if you consider it serious enough, and the timing critical, to have affected your performance in your assessed work and examinations.
Request for mitigation must be submitted to your programme administrator, in advance of your assessment submission deadline or exam. Requests for mitigation submitted after the assessment or exam (except those requests made as a result of circumstances that have arisen during the course of that assessment period) will not be considered without a credible and compelling explanation as to why the circumstances were not known before the beginning of the assessment period or why you were unable to complete or submit an application prior to the assessment or exam. Please note that not informing the University of circumstances due to personal feelings of embarrassment and pride, or having concerns over the confidential treatment of requests for mitigation, are not considered to be credible and compelling explanations
All mitigating circumstances applications must be supported by independent third party evidence. The type of evidence required will vary according to the nature of the circumstances. Examples of evidence include a doctor or other health professional’s letter, counsellor’s letter, self-certification form signed by your GP or GP’s Medical Practice (for illnesses of 7 days and under only). Please note that it is a University policy that the self-certification form must be signed by a GP; we cannot accept forms which have not been signed by a GP. Please note that if evidence has not been received within 2 weeks of the submission of your form, and you have not contacted them to inform them of any delay, your application will be refused and no further action will be taken.
Please ensure that you password protect or encrypt your mitigating circumstances form and supporting evidence before sending to your programme administrator.
Any requests for mitigation will be considered confidentially by a mitigating circumstances panel or sub-panel. Where a request for mitigation is supported, a recommendation will be made to the exam board for them to decide on the best course of action for the student.
You are advised to consult the following guidance, which directs you to seek advice and support before and whilst submitting a request for mitigation.
The University form and guidance for students, is available at: http://www.regulations.manchester.ac.uk/basic-guide-mitigating-circumstances/
For further information about the process and acceptable grounds for mitigation see: Mitigating Circumstances Policy & Procedures: http://documents.manchester.ac.uk/DocuInfo.aspx?DocID=4271
Please be advised that any requests need to be submitted by midday the day before the pre-arranged Mitigating Circumstances meeting.
24th October 2018
28th November 2018
9th January 2019
20th February 2019
20th March 2019
24th April 2019
22nd May 2019
19th June 2019
Late Submission Penalty (Including Dissertation)
Work submitted after the deadline without prior approval shall be subject to the following penalties:
The mark awarded for the piece of work will be reduced by:
· 10 marks if up to 24 hours late (1 day)
· 20 marks if up to 48 hours late (2 days)
· 30 marks if up to 72 hours late (3 days)
· 40 marks if up to 96 hours late (4 days)
· 50 marks if up to 120 hours late (5 days)
A zero mark will be awarded if the piece of work is more than 5 days late.
The sliding scale does not apply to referred assessment, where late submission will automatically receive a mark of zero.
For further information see: Policy on Submission of Work for Summative Assessment on Taught Programmes
Assignment Word Count (including the dissertation)
In accordance with the University Policy on Marking:
Each written assignment has a word limit which you must state at the top of your first page. It is acceptable, without penalty, for you to submit an assignment within a range that is plus 10% of this limit. If you present an assignment with a word count exceeding the specified limit+10%, the assignment will be marked but 1% will be deducted from this mark for every 100 words over the limit given.
For an original word limit that is 1000 words and an assignment that is marked out of 100. If a submission is made that is 1101 words then it exceeded the 10% leeway, and is more than 100 words over the original limit and should receive a 1 mark deduction.
In accordance with accepted academic practice, when submitting any written assignment for summative assessment, the notion of a word count includes the following without exception:
· All titles or headings that form part of the actual text. This does not include the fly page or reference list.
· All words that form the actual essay.
· All words forming the titles for figures, tables and boxes, are included but this does not include boxes or tables or figures themselves.
· All in-text (that is bracketed) references.
· All directly quoted material.
Certain assessments may require different penalties for word limits to be applied. For example, if part of the requirement for the assessment is conciseness of presentation of facts and arguments. In such cases it may be that no 10% leeway is allowed and penalties applied may be stricter than described above. In such cases the rules for word count limits and the penalties to be applied will be clearly stated in the assessment brief and in the submission details for that assessment.
Fitness to Practise
Postgraduate students at The University of Manchester, who are qualified health or social care professionals (e.g. doctor, dentist, nurse, social worker) registered by a healthcare or social care regulatory body (e.g. General Medical Council, General Dental Council, Nursing & Midwifery Council, Social Care Council) are expected to behave at all times, in a way that is consistent with the recommendations, or code of practice, of the relevant professional regulatory body.
Postgraduate students need to be aware that in the event of misconduct, dishonesty, unprofessional behaviour, or other behaviour or illness (e.g. mental health illness) that raises the possibility that the student’s fitness to practise may be impaired, the University has a duty to protect the public and to inform the relevant professional regulatory body.
This means, for example, that where a student has been found to be dishonest (e.g. plagiarism, collusion, falsification of research data or other forms of cheating) the matter may be reported by the University to the relevant professional regulatory body. Students who are dishonest not only risk failing to be awarded the intended degree, but also place at risk their whole professional career.
Information on Fitness to Practise related matters can be found at: www.tlso.manchester.ac.uk/appeals-complaints/fitnesstopractise
Academic Appeals, Complaints, Conduct and Discipline
Academic Appeals
- Students have a right of appeal against a final decision of an Examination Board, or a progress committee, or a graduate committee or equivalent body which affects their academic status or progress in the University.
- Students thinking of appealing should first discuss the matter informally with an appropriate member of staff, in order to better understand the reason for the result or decision.
- Should you wish to proceed to a formal appeal, this must be submitted within the timeframe outlined in the Academic Appeals Procedure to the Faculty Appeals and Complaints Team, Room 3.21, Simon Building, University of Manchester, M13 9PL (e-mail: FBMHappealsandcomplaints@manchester.ac.uk).
- The Academic Appeals Procedure (Regulation XIX) and associated documents, including the form on which formal appeals should be submitted, can be found at regulations.manchester.ac.uk/academic
Student Complaints
- The University’s Student Complaints Procedure (Regulation XVIII) and associated documents, including a complaints form, can be found at www.regulations.manchester.ac.uk/academic
- University has separate procedures to address complaints of bullying, harassment, discrimination and/or victimisation - see https://www.reportandsupport.manchester.ac.uk/
- Students thinking of submitting a formal complaint should, in most instances, attempt informal resolution first (see the procedure). Formal complaints should be submitted on the relevant form to Faculty Appeals and Complaints Team, Room 3.21, Simon Building, University of Manchester, M13 9PL (e-mail: FBMHappealsandcomplaints@manchester.ac.uk).
Conduct and Discipline of Students
- General University information on the Conduct and Discipline of Students can be found at http://www.staffnet.manchester.ac.uk/bmh/teaching/teaching-activity/fitness-to-practise/
- Faculty policies for students on Communication and Dress Code, Social Networking and Drugs & Alcohol can be found at:
- http://documents.manchester.ac.uk/display.aspx?DocID=29038 (Communication and Dress Code)
- http://documents.manchester.ac.uk/display.aspx?DocID=29039 (Drugs & Alcohol)
- http://documents.manchester.ac.uk/display.aspx?DocID=29040(Social Networking)
- Information on Academic Malpractice and how to avoid it can be found at http://www.regulations.manchester.ac.uk/guidance-to-students-on-plagiarism-and-other-forms-of-academic-malpractice/
4. Student Progression
Monitoring Attendance and Wellbeing of Students
The programme director and teaching staff will monitor the work and attendance of students on the programme. This is for your benefit and helps to ensure you are coping with the work. Regular or a pattern of non-attendance and/or engagement will result in you being contacted by the School to meet with your programme director. Following this, further action will be taken if there isn’t a significant improvement in attendance.
For further information see:
Regulation XX Monitoring Attendance and Wellbeing of Students
The University offers a range of advice and support to students experiencing problems with attendance. Further information can be found in the A-Z of Student Services: http://www.studentnet.manchester.ac.uk/crucial-guide/
You can also speak to your Programme Director and/or Academic Advisor.
What to do if you are absent
In case of illness you should supply a doctor’s certificate or, if the illness is brief, a self-certification. If you are absent for other reasons then you should write a letter to the Programme Director explaining the circumstances. Medical certificates or letters should be given in person or sent to the Programme Administrator. Whatever your reason for being away, tell your supervisor about it and make any necessary arrangements to catch up with work you have missed.
Special Permissions
Interruptions to programme and extensions to writing up
It is the expectation of the University that postgraduate taught students pursue their studies on a continuous basis for the stipulated duration of their programme. However, it is recognised that students may encounter personal difficulties or situations which may seriously disrupt or delay their studies. In some cases, an interruption or extension to your programme of study may be the most sensible option.
Students who wish to interrupt the programme or extend to write up the dissertation should initially discuss their plans and reasons with the Programme Director and/or their Academic Advisor.
Students should also provide documentary evidence when appropriate, for example, doctor’s letter, sick note etc.
The forms required for formal application are available from your Programme Administrator.
Withdrawal from the Programme
Students who are considering withdrawing from the programme should discuss this in the first instance with the Programme Director.
If arrangements for withdrawal need to be made, this will be handled by the Programme Administrator, who will manage communication with the Fees and Records Departments and other University bodies as appropriate OR Students may liaise directly with the Programme Administrator who will communicate this information directly to the University Student Services Centre.
5. Student Support
Student Support and Guidance
Student support and guidance within the programme
Support and advice is available to all students both formally and informally from the Programme Directors, the Programme Administrator and research project supervisors.
If you have any queries or would like to discuss any issues at all – academic, administrative, technical or personal – please do not hesitate to get in touch. All personal issues will be dealt with confidentially.
If we are unable to help you directly, we can put you in touch with many of the support services that are available to students of the University through our Student Services Centre. You can approach these services independently, without the involvement of programme staff. Use the A-Z of Student Services Guide as an additional source of information.
Student support for the dissertation
During the research project and writing up of the dissertation, students will have individual support from their research project supervisor and scheduled structured sessions to monitor their progress and provide support, with help being offered if any problems are being encountered. In addition, students are made aware that they have the option of contacting the programme directors at any time if they are experiencing difficulties, whether this is in relation to their project, or indeed, with regard to any other issue of relevance.
Student support from the University
The University offers a range of support and guidance services to students, for example, Student Health Service, Student Union Advice Centre, Student Counselling and Careers Advice. Details of all these services can be obtained from the A-Z of Student Services
Counselling Service
The counselling service is available for all students. It is free and consists of a team of professional counsellors. The service provides confidential counselling for anyone who wants help with personal problems affecting their work or well-being.
The service is open 9.00am to 5.00pm Monday to Friday all year round except public holidays.
http://www.studentnet.manchester.ac.uk/counselling/
Occupational Health
Occupational Health is a specialised area of medicine concerned with the way in which an individual’s health can affect his or her ability to do a job and to study and conversely how the work environment can affect an individual’s health. Their aim is to promote the physical, mental and social well-being of students and to reduce the incidence of ill-health arising from exposure to work place hazards.
http://www.occhealth.manchester.ac.uk/
Students Union Advice Centre
The Students Union has advisers who can help with any matter ranging from finances to housing and beyond. On the South Campus, the Advice Centre is on the first floor in the Student Union Building, and is open Monday to Friday, 10.00am to 4.00pm, term time and vacation. There is no need to make an appointment.
Disability Advisory and Support Service (DASS)
The University of Manchester welcomes students with a disability or specific learning difficulties. The University has a Disability Advisory and Support Service, who can supply further information and DASS advisors will be pleased to meet you to discuss you needs. DASS will liaise with your School through the Disability Coordinator to make the necessary arrangements for your support during your time in Manchester.
The DASS office can also provide a copy of the University’s Disability Statement, ‘Opportunities for Students with Additional Support Needs at the University of Manchester’ which sets out the policy and provision for students with a disability.
DASS Contact Details:-
Location: 2nd Floor, University Place
Email: dass@manchester.ac.uk; Phone: 0161 275 7512
Text: 07899 658 790; Website: www.dass.manchester.ac.uk
Disability Coordinator Contact Details:-
Name: Wendy Gregson (0161 306 7972) & Nick Cunningham (0161 275 1344)
Email: dc.medicalsciences.pgt@manchester.ac.uk
Looking after yourself and your patients during Ramadan
The Faculty of Biology, Medicine and Health has produced guidance for healthcare students on fasting and caring: Fasting and Caring - Looking after yourself and your patients during Ramadan: guidance for health care students.
6. Student Representation and Feedback
Student Representation and Feedback
Students, in consultation with the Programme Administrator, should arrange an informal election of their Student Representative near the beginning of the academic year. If more than one person is interested in the role, then each candidate is asked to write a short proposal which is circulated to the student body, and an election is held.
The overall responsibilities of the Student Representative are
- to liaise between staff and students about matters of concern
- to provide two-way feedback on programme and teaching quality
- to promote active student involvement in the development of the programme
- to identify student issues and needs on the programme
- to attend programme committee meetings representing the student voice
- to find effective ways to feedback the outcomes of meetings to the student body
- to attend relevant student representative training
- to liaise with other Student Representatives to gain support and ideas
- to become established as a central point for information and guidance for students in the group.
Student representatives are not required to get involved with fellow students’ personal problems, academic difficulties, or individual student allegations of unfair or inappropriate treatment.
Confidentiality is imperative when dealing with student issues. The representative is chosen by fellow students and has their trust, and must maintain it. Any discussion of an individual student’s situation with a third party requires their consent beforehand.
7. Programme Management
Programme Management and Committee Structure
Programme Management
The programme is managed and operated in accordance with the policies, principles, regulations and procedures of the University of Manchester.
Programme Directors relate to the School and Faculty Postgraduate Teaching Committees on matters relating to admissions, exams, reviews and approval of new programmes and units, quality assurance etc. and policy issues of broad relevance to the Graduate School.
The Programme Committee will meet each semester and consist of the Programme Director, Programme Administrator, Programme Committee members and the unit co-ordinators.
The remit of the committee will be to:
- Oversee the teaching, assessment and examining arrangements;
- Monitor cohort progression including failure rate, withdrawal rate;
- Evaluate the extent to which the learning outcomes are achieved by students;
- Monitor, maintain and enhance standards of all aspects of the programme;
- Evaluate the effectiveness of the curriculum and of assessment in relation to programme learning outcomes;
- Evaluate the effectiveness and relevance of the teaching and learning methods employed;
- Review and revise the programme in the light of any relevant Quality Assurance Agency (QAA) benchmarks, any other relevant external and/or professional requirements and developing knowledge in the subject area;
- Receive, consider and respond to feedback from students, employers and external examiners;
- Where the need for change is identified, effect the changes quickly and efficiently;
- Produce an annual action plan via annual monitoring;
- Produce reports for periodic review
- Produce relevant information for an Institutional Audit;
- Review programme documentation, e.g., programme handbooks, programme specifications, promotional literature and programme website;
- Ensure suitable and efficient arrangements are in place for recruitment, admission and induction.
Committee Structure
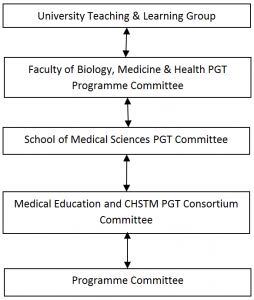
The Programme Committee acts as a curriculum development team for the Programme. The Programme Committee will report to a School, or Department, or Faculty level committee. The Programme Director is responsible for the management of the programme, and the Programme Committee is established to support the Programme Director in the carrying out of their responsibilities.
The role of the External Examiner
External Examiners are individuals from another institution or organisation who monitor the assessment processes of the University to ensure fairness and academic standards. They ensure that assessment and examination procedures have been fairly and properly implemented and that decisions have been made after appropriate deliberation. They also ensure that standards of awards and levels of student performance are at least comparable with those in equivalent higher education institutions.
External Examiners’ reports
External Examiners’ reports relating to this programme will be shared with student representatives at the programme committee, where details of any actions carried out by the programme team/School in response to the External Examiners’ comments will be discussed. Students should contact their student representatives if they require any further information about External Examiners’ reports or the process for considering them.
External Examiner Details
The External Examiner for this programme is Dr Andrew Smith, Consultant Anaesthetist, University Hospital of Morecambe Bay NHS Trust (subject to approval).
Please note that it is inappropriate for students to make direct contact with External Examiners under any circumstances, in particular with regards to a student’s individual performance in assessments. Other appropriate mechanisms are available for students, including the University’s appeals or complaints procedures and the UMSU Advice Centre. In cases where a student does contact an External Examiner directly, External Examiners have been requested not to respond to direct queries. Instead, External Examiners should report the matter to their School contact who will then contact the student to remind them of the other methods available for students. If students have any queries concerning this, they should contact their Programme Office (or equivalent).
8. Learning Resources
Learning Resources
Libraries
All registered students may become members of the University of Manchester Library on the main campus.
Up-to-date news about the library is available here.
IT Services and eLearning
IT Services Support Centre online
Details can be found at: http://www.itservices.manchester.ac.uk/help/
Login to the Support Centre online to log a request, book an appointment for an IT visit, or search the Knowledge Base.
Telephone: +44 (0)161 306 5544 (or extension 65544). Telephone support is available 24 hours a day, seven days a week.
In person: Walk-up help and support is available at the Joule Library, Main Library or Alan Gilbert Learning Commons:
Use Support Centre online for support with eLearning, from where you may make a request, report a fault, or search the Knowledge Base. The email address is: elearning@manchester.ac.uk
Blackboard
Blackboard, the University's 'virtual learning environment', will be used for online teaching.
What is Blackboard?
Blackboard is a web-based system that complements and builds upon traditional learning methods used at The University of Manchester. By using Blackboard you can
- view course materials and learning resources,
- communicate with lectures and other students,
- collaborate in groups,
- get feedback
- submit assignments
- monitoring your own progress at a time and place of your own convenience.
Training in the use of software
The Faculty eLearning team have produced a short introduction to Blackboard for new students. The recording is hosted in two places: the VLS and on YouTube:
The recording is just over seven minutes long and covers most of the commonly used tools in Blackboard.
9. Useful Links
Academic and Student Support Policies
Academic Support Policies
A list of University Policies and documents can be found at:http://documents.manchester.ac.uk/list.aspx
Academic Appeals (Regulation XIX)
http://documents.manchester.ac.uk/DocuInfo.aspx?DocID=187
Academic Malpractice: Procedure for the Handling of Cases
http://documents.manchester.ac.uk/DocuInfo.aspx?DocID=639
Basic Guide to Student Complaints
http://documents.manchester.ac.uk/display.aspx?DocID=23875
Conduct and Discipline of Students (Regulations XVII)
http://documents.manchester.ac.uk/DocuInfo.aspx?DocID=6530
General University information on the Conduct and Discipline of Students can be found at www.tlso.manchester.ac.uk/appeals-complaints/conductanddisciplineofstudents/.
Faculty policies for students on Communication and Dress Code, Social Networking and Drugs & Alcohol can be found at:
- http://documents.manchester.ac.uk/display.aspx?DocID=29038 (Communication and Dress Code)
- http://documents.manchester.ac.uk/display.aspx?DocID=29039 (Drugs & Alcohol)
- http://documents.manchester.ac.uk/display.aspx?DocID=29040(Social Networking)
Information on Academic Malpractice and how to avoid it can be found at
http://www.regulations.manchester.ac.uk/guidance-to-students-on-plagiarism-and-other-forms-of-academic-malpractice/
Data Protection
http://www.manchester.ac.uk/aboutus/documents/privacy/
Guidance for the Presentation of Taught Masters Dissertations
http://documents.manchester.ac.uk/display.aspx?DocID=2863
Guidance to Students on Plagiarism and Other Forms of Academic Malpractice
http://documents.manchester.ac.uk/display.aspx?DocID=2870
Policy on Submission of Work for Summative Assessment on Taught Programmes
http://documents.manchester.ac.uk/display.aspx?DocID=24561
Policy on Mitigating Circumstances
http://documents.manchester.ac.uk/display.aspx?DocID=4271
Mitigating Circumstances Guidance for Students
http://documents.manchester.ac.uk/display.aspx?DocID=23886
PGT Degree Regulations
http://documents.manchester.ac.uk/display.aspx?DocID=29208
Policy on Feedback to Undergraduate and Postgraduate Taught Students
http://documents.manchester.ac.uk/DocuInfo.aspx?DocID=6518
Student Complaints Procedure
http://documents.manchester.ac.uk/DocuInfo.aspx?DocID=1893
Student Charter
http://www.studentnet.manchester.ac.uk/enhancing-my-experience/charter
Work and Attendance of Students (Regulation XX)
http://documents.manchester.ac.uk/display.aspx?DocID=1895
A-Z of Student Services
http://www.studentnet.manchester.ac.uk/crucial-guide/
Accommodation
http://www.accommodation.manchester.ac.uk/
Blackboard
Students should access Blackboard via my Manchester at https://my.manchester.ac.uk
Careers Service
http://www.careers.manchester.ac.uk/
Counselling Service
https://www.counsellingservice.manchester.ac.uk/
Disability Advisory and Support Service
http://www.dass.manchester.ac.uk/
University Language Centre – Study English - Tel: 0161 306 3397
http://www.languagecentre.manchester.ac.uk/study-english/
Equality, Diversity and Inclusion for Staff and Students
http://www.manchester.ac.uk/aboutus/equalityanddiversity/
Health & Fitness
http://www.sport.manchester.ac.uk/
Health & Safety Policy
http://documents.manchester.ac.uk/display.aspx?DocID=654
International Advice Team
http://www.manchester.ac.uk/international/support/advice/
IT and eLearning Support
http://bmh-elearning.org/technical-support/
Mature Students Guide
http://documents.manchester.ac.uk/display.aspx?DocID=18122
Occupational Health Services for Students
http://www.occhealth.manchester.ac.uk/postgraduates/
Personal Development Planning
http://www.tlso.manchester.ac.uk/personaldevelopmentplanning/
A Personal Safety Guide for International Students
http://www.studentnet.manchester.ac.uk/medialibrary/study/safety-international-student-guide.pdf
Students Union
http://manchesterstudentsunion.com/

