1. General Information
Welcome to the School of Medical Sciences
Welcome to your Postgraduate Taught Programme in the School of Medical Sciences within the Faculty of Biology, Medicine and Health at the University of Manchester. The University has a worldwide reputation based on high quality teaching and research, and I am sure that your programme will provide a solid foundation for your future career success.
Within the School and the wider Faculty, our goal is to create an environment that allows you to excel and reach your full potential. Offering access to first-class facilities and strong links with regional health-service providers, our postgraduate programmes are designed to meet the diverse needs of all our students. The curriculum of our taught programmes provides the knowledge and skills you will need in your subject area and all our Masters programmes include an opportunity to carry out an independent research project on topics spanning all areas of biomedical research from molecular to experimental biology and clinical medicine. While subject areas cover a broad range, all our taught programmes have two common aims:
- To develop your skills in your chosen field of study
- To enhance your knowledge within the field you have chosen. Whether you are a graduate, professional or have a clinical background, the programmes have been tailored to meet your specific needs.
As a student of the School of Medical Sciences, you will be expected to take responsibility for your degree, within a supportive environment that fosters your development and helps prepare you for your future career. This handbook will be a useful resource as you progress through your programme. It provides programme-specific information that I am sure that you will find helpful throughout your study. If however, you have questions or would like some further advice, please do not hesitate to contact the people listed in this handbook for further information and assistance.
I wish you every success as you embark upon your programme, and in your future career.
Dr Carol Yates
Director of Postgraduate Taught Education
School of Medical Sciences
Faculty of Biology, Medicine and Health
Updated version
Academic year 2019/20
Points of Contact
|
Programme Director, Examinations Officer & Pathway Lead: Clinical Biochemistry |
Dr Phil Macdonald Senior Lecturer School of Medical Sciences Faculty of Biology, Medicine and Health University of Manchester Philip.macdonald@manchester.ac.uk 0161 275 1606 |
| Clinical Lead | Mrs Katharine Hayden FRCPath Consultant Clinical Biochemist, Clinical Biochemistry MRI, Oxford Road, Manchester M13 9WL katharine.hayden@cmft.nhs.uk 0161 276 4834 |
| Co-Pathway Leads: Clinical Immunology | Dr Jo Pennock Non-clinical Lecturer School of Medical Sciences Faculty of Biology, Medicine and Health University of Manchester joanne.l.pennock@manchester.ac.uk Tel: 0161 275 1582Susana Marinho Co-Lead for Hypersensitivity & Allergy Unit Susana.Marinho@UHSM.NHS.UKDr Nick Barnes Lecturer in Healthcare Science (Clinical Immunology) School of Medical Sciences Faculty of Biology, Medicine and Health University of Manchester nicholas.barnes-2@manchester.ac.uk Tel: 0161 275 4964 |
|
Pathway Lead: Histocompatabilty and Immunogenetics |
Ms Natalia Diaz Burlinson, FRCPath Consultant Clinical Scientist Transplantation Laboratory Manchester Royal Infirmary Oxford Road Manchester M13 9WL natalia.diazburlinson@mft.nhs.uk Tel: 0161 276 6215 |
|
Pathway Lead: Haematology & Transfusion Science |
Dr Nina Dempsey-Hibbert FHEA Senior Lecturer in Blood Sciences School of Healthcare Science John Dalton Building Manchester Metropolitan University Chester Street Manchester M1 5GD Tel: 0161 247 1175 N.Dempsey-Hibbert@mmu.ac.uk |
| Programme Administrator | Ben Bone Programme Administrator School of Medical Sciences Graduate Office 1.485, 1st Floor, Stopford Building University of Manchester 0161 275 5265 clinicalscience@manchester.ac.uk |
| Personal Tutor | To be allocated |
Online Skills Training Resource
The Faculty has developed a skills training resource to support you through your postgraduate taught programme. This online material should supplement the assessed learning material and activities undertaken in your taught programme.
Accessing the online skills resource
You can access Blackboard through the My Manchester portal (http://my.manchester.ac.uk). The skills training resource is available in an academic community space available to all registered PGT students in the Faculty through Blackboard.
If you cannot see these units in your Blackboard please contact your Programme Administrator.
Content
Full details of all these resources can be found in the introduction to each unit. These resources have been designed to give you formative feedback on your progress through them. If you experience any problems and would like to talk to someone please contact your Programme Director. If you have questions about referencing and how it applies to your own work, please contact your Programme Director or dissertation supervisor/module lead.
| Academic Writing | This is an excellent resource that supports you to write your assignments and dissertation. It is split into units that focus on key areas that previous students have found difficult and aims to enhance your academic writing style. |
| Research Methods* | This course is spilt into 3 units that cover introductions to study design, statistics and dissertation skills. It has a number of online quizzes where you can test your knowledge. |
| Statistics* | The course provides a valuable foundation for understanding and interpreting biostatistics. It aims to provide you with the fundamentals of quantitative analysis. |
| Presentation Skills | This short interactive unit is designed to help you to enhance your presentation skills. Regardless of whether you are presenting in public, preparing for conferences, an oral examination or more informal settings this unit will give you the tops tips to improve your delivery. |
| Qualitative Research Methods* | This unit has been designed to give you an introduction to Qualitative Research. |
| SPSS* | This is an introduction to statistics, using SPSS, a popular and comprehensive data analysis software package containing a multitude of features designed to facilitate the execution of a wide range of statistical analyses. |
| Intellectual Property Awareness Resource | This Intellectual Property (IP) awareness resource has been created in order to improve your understanding of IP. Topics include: Types of intellectual property • Copyright and IP clearance • University policy on IP • IP commercialisation • IP in research or consultancy • IP issues to be aware when dealing with academic materials |
* NOTE: the material in this online resource is for reference and formative learning purposes only. In some of your taught programme you may be required to undertake assessed course units for Research Methods, Qualitative Research or Statistics. If your programme involves taught units then you should refer to the Blackboard material relating to that course unit. Please contact your Programme Administrator if you are unsure which material relates to your assessed work. You will still be able to refer to the online skills resource in later years.
Introductory Courses
All students are automatically enrolled onto an introductory unit that provides information on health and safety, academic malpractice and academic literacy. Completion instructions for each of these sections are clearly defined within the course. Completion of the academic malpractice and health and safety sections is mandatory for all students. All assessments must be completed as soon as possible after the programme begins, with the academic malpractice assessment completed before the first piece of coursework is submitted. Completion of these assessments is monitored by the School. All students are also strongly advised to complete the academic literacy section.
Health and Safety
Before you visit the University campus, please take time to read the University’s Health and Safety Policy.
Communication with Students
Please note that only Blackboard, the University e-learning platform and your allocated student university email address will be used as official communication by University staff. It is your responsibility to ensure that you can access and read email from this source.
Students are required to keep the University informed of any change to their personal circumstances such as change of name or address. Changes can be recorded by the student via their own personal online record. It is also essential to inform the Programme Administrator if you do not intend to return to the next session of the course, if, for example, you are moving away.
2. Overview of the Programme
Programme Overview
The MSc Clinical Sciences (Blood Sciences) is designed to provide students with a knowledge and understanding of the theory and practice of the blood sciences (Clinical Biochemistry, Clinical Immunology, Haematology & Transfusion Science and Histocompatibilty & Immunogenetics). To equip students with the transferable, intellectual and professional skills to permit them to develop their academic and professional potential throughout their career by fostering lifelong learning in the pursuit of excellence in scholarship and professional practice.
The MSc Clinical Science (Blood Sciences) programme is delivered by the University of Manchester (UoM) in collaboration with Manchester Metropolitan University (MMU). All of Year 1 and Years 2 and 3 of the Clinical Biochemistry, Clinical Immunology and Histocompatibility & Immunogenetics specialism pathways are taught by the UoM, with years 2 and 3 of the Haematology and Transfusion Science specialism pathway being delivered by MMU. All teaching will be delivered on the main campuses of UoM and MMU.
Aims of the Programme
- Equip students with knowledge and understanding of the theory and practice of clinical biochemistry, clinical immunology, histocompatibility and immunogenetics, or haematology and transfusion science.
- Produce graduates with a critical understanding of how data generated by blood science service laboratories is employed to develop a clinical diagnosis, and how this information can be logically and systematically employed to deliver effective day to day management of common medical conditions.
- Contribute to innovation, change and service developments in clinical science at both the laboratory and institutional levels by equipping students with a systematic and critical understanding of relevant knowledge, theoretical frameworks and advanced skills.
- Enhance career-long development and promote lifelong learning in students in order to support and enhance best practice in clinical biochemistry, clinical immunology, histocompatibility and immunogenetics, haematology or clinical genetics.
Learning Outcomes of the Programme
Knowledge & Understanding
On completion of the programme students should be able to:
- (All pathways)Demonstrate knowledge of the normal physiology of the major organ systems of the body
- (All pathways) Display a critical understanding of the regulatory processes and practices involved in conducting research in a health service or academic setting.
- (All pathways) Demonstrate a knowledge and critical understanding of the use of internal and external quality assurance systems in health service laboratories
- (All pathways) Display knowledge of the theory and critical understanding of the use of the major analytical techniques employed within the blood science disciplines.
- (Clinical Biochemistry pathway only) Exhibit knowledge of the scientific basis and practice of clinical biochemistry, and a critical understanding the role the discipline plays in the investigation, diagnosis and management of disease.
- (Clinical Immunology pathway only) Exhibit knowledge of the scientific basis and practice of clinical immunology, and a critical understanding the role the discipline plays in the investigation, diagnosis and management of disease.
- (Histocompatibility & Immunogenetics pathway only) Exhibit knowledge of the scientific basis and practice of histocompatibility and immunogenetics, and a critical understanding the role the discipline plays in the investigation, diagnosis and management of disease and in the transplantation services.
- (Haematology & Transfusion Science pathway only) Exhibit knowledge of the scientific basis and practice of haematology, and a critical understanding the role the discipline plays in the investigation, diagnosis and management of disease.
- (All pathways) To systematically and critically employ the knowledge and understanding obtained during the taught component of the programme to address an original research question through the design and undertaking of a comprehensive research project and production of a dissertation.
Intellectual Skills
At the end of the programme students should be able to:
- Critically reflect on and challenge their own practice, the practice of others and the organisation and delivery of blood science services in order to ensure use of appropriate values and best evidence in delivering patient care and management.
- Appraise and interpret information from different sources in order to develop a coherent critical analysis of issues relating to the practice and delivery of blood science services.
- Systematically and objectively evaluate what biomedical parameters need to be established to develop a valid diagnosis of a patient displaying specific clinical symptoms.
- Critically evaluate the performance of new analytical technologies in the context of the specific requirements of the health service.
- To synthesis, analyse and systematically combine information obtained from different sources to develop a defined original research question and then to address it through the development of a coherent research project.
Practical Skills
Students should be able to:
- Effectively communicate with colleagues within the pathology service and clinical staff through the presentation of verbal and written reports
- Collect, collate and record scientific data according to established health service practices
- Contribute to the advancement of effective and timely patient diagnosis through a knowledge and understanding of the multidisciplinary environment of the pathology service within the modern health service.
- Contribute to the strategies for practice development and change at both a team and organisational level to enhance access to and effectiveness of clinical science services.
- Design a scientifically valid experimental strategy to address a specific research question relevant to modern clinical science practice.
Transferable Skills and Personal Qualities
On completion of the programme students should be able to:
- Communicate effectively in a variety of settings with a range of individuals.
- Effectively utilise information technology/health informatics.
- Demonstrate research and enquiry skills by accessing and analysing literature in order to inform and develop practice.
- Work co-operatively and effectively with others as a member of a team.
- Reflect on their own academic and clinical performance and utilise strategies to improve these.
- Use logical and systematic approaches to problem-solving and decision-making.
Programme Structure and Credits
The MSc Clinical Science (Blood Sciences) programme is a part-time programme delivered over three years. The programme is composed of a 120 credit taught component, which consists of 60 credits of core teaching delivered in semester 1 of year 1 and 60 credits of discipline specific teaching delivered in semesters 1 and 2 of years 2 and 3, and a 60 credit research project undertaken in years 2 and 3. The structure of the programme is illustrated in Figure 1.
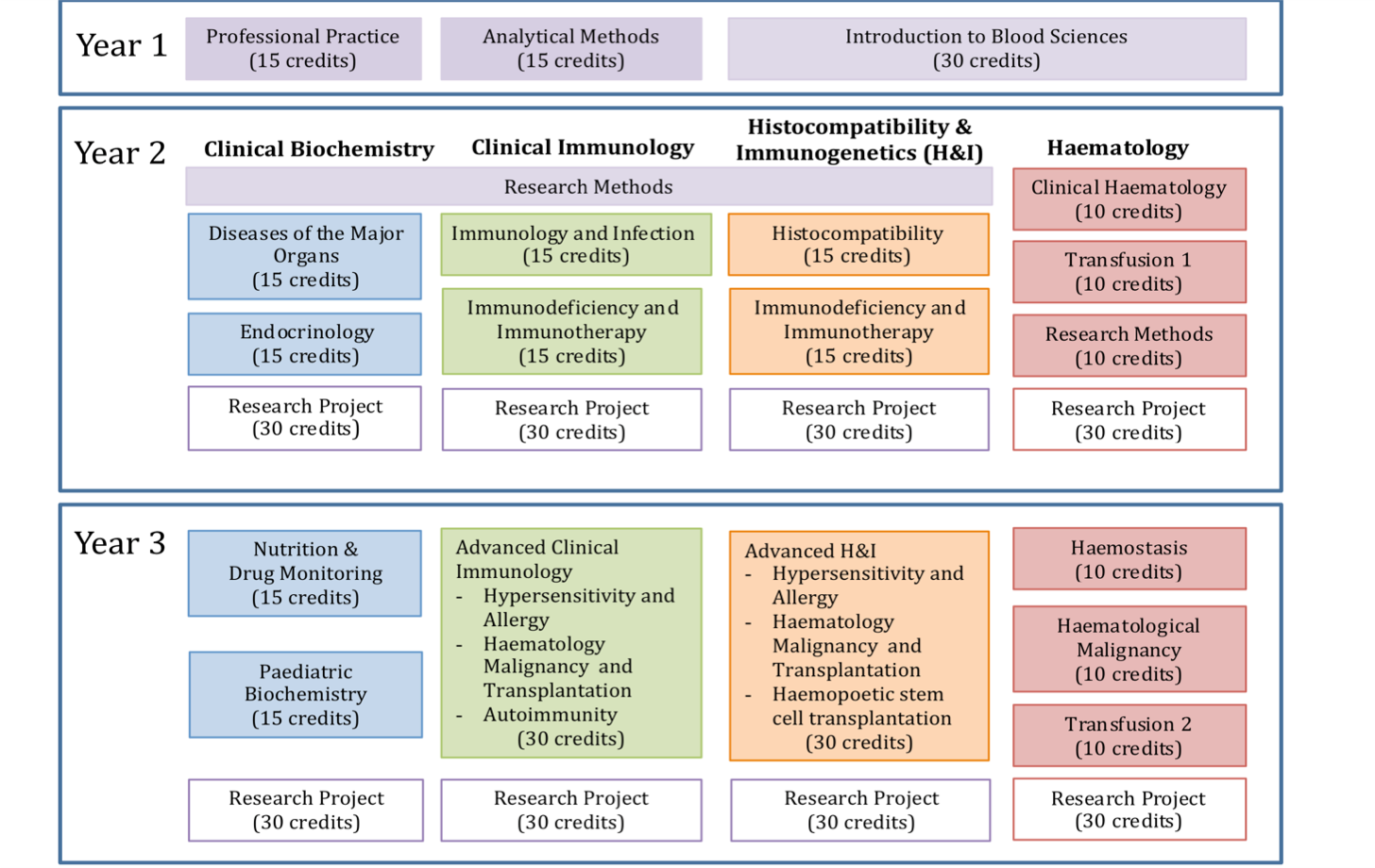
Figure 1. Diagram illustrating the structure of the MSc in Clinical Science (Blood Sciences), highlighting the four subject specific pathways
The units within this section of the programme are compulsory and will be taken by all students registered on the MSc Clinical Science (Blood Sciences).
Professional Practice (15 credits)
NHS Trainees and qualified NHS staff are required to meet professional standards as defined by Good Scientific Practice and the Health and Care Professions Council (HCPC – the regulatory body). This involves working and training in a safe, lawful and effective manner. High levels of communication skills are required to interact effectively with multidisciplinary clinical teams. It is also crucial to understand the impact that healthcare scientists have in the patient pathway.
This unit will enable trainees to gain the knowledge, skills, experience and tools to develop, improve and maintain high standards of professional practice during their training and beyond. The unit will explore the principles of good clinical practice (GCP), medical ethics, communication, clinical history taking and leadership skills. The unit also provides a broad knowledge and understanding in key areas within healthcare science which are relevant across disciplines by providing an introduction into public health, psychosocial aspects of health and disease, clinical pharmacology/ therapeutics genomics/bioinformatics and medical imaging.
Analytical Methods (15 credits)
This unit provides students with a comprehensive overview of the main analytical technologies and diagnostic platforms employed within the blood science disciplines. The unit will provide the basic fundamental technical background to many of these techniques in order to students to understand how each can be applied in a clinical setting. In addition the unit will provide students with knowledge and understanding of the principles of analysis, quality assurance and point of care testing.
Introduction to the Blood Sciences (30 credits)
The aim of this unit is to provide students with the knowledge to underpin the divisional hospital-based professional rotations they undertake during the first twelve months of the MSC STP curriculum. The unit contains four self-contained modules that are designed to provide students with an introduction to the theory and practice of each of the four main disciplines (Clinical Biochemistry, Clinical Immunology, Haematology & Transfusion Science and Genetics) within the blood sciences division of the healthcare sciences. The unit will provide students with a critical appreciation of the role each of the four blood sciences disciplines play in the diagnosis and management of disease.
For convenience this unit is subdivided into four modules:
- Introduction into Clinical Biochemistry
- Introduction into Clinical Immunology
- Introduction into Haematology and Transfusion Science
- Introduction into Genetics
Discipline Specific Taught Units (60 credits)
This section of the programme permits a student to specialise in a specific blood science discipline either: Clinical Biochemistry, Clinical Immunology, Histocompatibility & Immunogenetics, or Haematology & Transfusion Science. Each specialism pathway consists of a prescribed number of subject specific taught units (see Figure 1).
Please note that for administrative purposes and due to the 15 credit framework employed by the UoM for its Masters programmes the 10 credit Research Methods unit present in the MSC curriculum has been split into two 5 credit blocks, which have been incorporated into the two year 2 clinical units. This administrative reorganisation does not apply to the Haematology & Transfusion Science pathway as MMU uses a 10 credits unit structure for its Masters so can directly comply with the organisation of the MSC curriculum.
All the subject specific units in the Clinical Biochemistry pathway will be delivered by UoM.
Year 2 To be fully compatible with the MSC curriculum these two units delivered in year 2 each nominally contain 5 credits of the research methods generic content.
Diseases of Major Organs (15 credits): This unit will provide students with an in depth understanding of how disorders of the major organs (lungs, kidneys, liver, brain and muscle) impact biochemical parameters such as acid base balance, blood gasses, blood and urine proteins, water and electrolyte balance. In addition, students will gain an in depth insight into the role biochemical investigations play in the diagnosis and management of common cancers. This unit will also equip students with a critical appreciation and understanding of how information obtained through the biochemical investigation of major organ function can be applied to diagnose disease. In addition, this unit will provide students with an appreciation of study design, an introduction to the basic principles of epidemiology and evidence based practice (nominally 5 credits of generic material).
Endocrinology (15 credits):
This clinical unit has been designed to provide you with the knowledge and understanding of the physiology of endocrine glands and the biochemistry tests used to investigate endocrine disorders. The clinical and laboratory investigations used for the diagnosis and management of diabetes will be covered, in addition to endocrine disorders affecting the pituitary, thyroid and adrenal glands and the GI tract. In addition the unit covers the investigation of infertility and endocrine conditions affecting gonadal function.
The unit uses a blended learning approach combining direct teaching with problem-based learning, literature review and clinical case material including interpretation of dynamic function tests to investigate endocrine conditions. The goal of this approach is to enable you to combine the theoretical knowledge with the skills required to provide advice and interpretation of endocrine tests in clinical scenarios
Year 3
Nutrition and Drug Monitoring (15 credits):
Nutrition: Adequate nutrition is fundamental to human health and development. When it goes wrong, major health problems can follow such as diabetes type 2 in obesity, and life-threatening cardio-respiratory problems accompanying severe chronic malnutrition. Clinical Biochemists and other laboratory professionals have a major role to play in evaluating nutritional status, monitoring patients with altered nutritional needs and advising on changes to diets to ensure optimal growth, development and wellbeing
The Nutrition Module of the Life Sciences (Blood Sciences) MSc aims to give students a basic understanding of the fundamentals of human nutrition, the consequences of over- and under-nutrition and the role of the laboratory in determining dietary needs of patients with underlying chronic illnesses affecting absorption, distribution or excretion of macro- and micro-nutrients Students will obtain an understanding of the role trace elements and vitamins in maintaining an individual’s health and wellbeing. They will also gain an appreciation of the importance of clinical and biochemical parameters in diagnosing and managing nutritional disorders. The students will also learn about the biochemistry of haem synthesis and clinical disorders related to defects in the haem synthetic pathway.
Drug monitoring: The use of drugs in the treatment of disease is at the foundation of modern medicine. This part of the unit is designed to give you an overview of the absorption, distribution, metabolism and excretion of drugs. Using these principles the unit then progresses into other areas for you to develop an understanding of therapeutic drug monitoring, overdose, abuse, pharmacogenetics and forensic toxicology. Clinical Scientists have a central role to play in the interpretation of drug assays, the advice given to clinical teams and the actions taken on the basis of these results.
The course material is a mixture of formal lectures and presentations of clinical cases.
The unit will equip students with a knowledge and understanding of basic pharmacokinetics and pharmacogenetics, and acquire an understanding of the principles and toxicology and drug monitoring.
Paediatric Biochemistry (15 credits):
The unit provides grounding in clinical biochemistry specifically relevant to paediatric populations from birth through the neonatal period, infancy, childhood and adolescence. It covers areas of clinical biochemistry of particular relevance to paediatrics and students will learn that whilst some biochemical tests may be clinically relevant in patients of all ages their interpretation or likely diagnoses are different in paediatric and adult populations.
The module includes an overview of the physiological changes to mother and fetus during pregnancy and complications which can occur and a session on electrolyte and acid-base problems in the neonate. Other specific areas covered include hypoglycaemia, hyperammonaemia and neonatal hyperbilirubinaemia. There is also a strong focus on paediatric endocrine disorders taught predominantly via case based sessions. The students are also introduced to the principles and practice of newborn screening and the major categories of inherited metabolic disorders, such as organic acidurias, amino acid disorders, peroxisomal, lysosomal and mitochondrial disorders.
The unit aims to provide the student with an understanding of the key issues of interpretation in paediatric biochemistry, particularly the concept that children and babies are not merely small adults. It also aims to give the student an overview of the nature, modes of presentation and methods of diagnosis for the key inherited metabolic disorders.
All the subject specific units in the Clinical Immunology pathway will be delivered by UoM, with the exception of Haematological Malignancies and Transplantation, which will be delivered at MMU.
Year 2
To be fully compatible with the MSC curriculum these two units delivered in year 2 each nominally contain 5 credits of research methods generic content.
Immunology & Infection (15 credits): This unit provides students with a knowledge and understanding of the scientific basis of immunity, and provide students with a good understanding of how the immune system functions in response to both infection and cancer. The student will become familiar with methods and strategies to investigate the immune system in infection and malignancy, and the clinical significance of results in relation to infection and malignancy. In addition, this unit will provide students with an appreciation of study design, an introduction to the basic principles of epidemiology and evidence based practice (nominally 5 credits of generic material).
Immunodeficiency & Immunotherapy (15 credits): This unit will provide the student with knowledge and understanding of the causes of immunodeficiency. They will understand the clinical presentation and investigation of a range of immunodeficient conditions and the principles and practice of immunotherapy. They will become familiar with methods and strategies to investigate immunodeficiency and gain experience of the interpretation of patient results in a variety of clinical settings. The unit will also provide students with an introduction to biostatistics and their use in data analysis (nominally 5 credits of generic material).
Year 3
In year 3 there is one 30 credit unit called Advanced Clinical Immunology, which comprises three 10 credit modules.
Hypersensitivity & Allergy (nominally 10 credits): This unit will provide the student with knowledge and understanding of the mechanism of hypersensitivity and allergy. They will understand the clinical presentation and investigation of a range of associated conditions. They will become familiar with methods and strategies to investigate hypersensitivity and allergy and gain experience of the interpretation of patient results in a variety of clinical settings.
Haematological Malignancies & Transplantation (nominally 10 credits): This unit equips students with knowledge and understanding of the pathophysiology, clinical presentation and management of patients with haematological malignancies. Furthermore, the unit will provide students with knowledge of the scientific basis of organ transplantation and an understanding of principles and practice of organ transplantation.
Autoimmunity (nominally 10 credits): This module will provide the student with knowledge and understanding of the mechanism of autoimmunity. They will understand the clinical presentation and investigation of a range of autoimmune disease. They will become familiar with methods and strategies to investigate autoimmunity and gain experience of the interpretation of patient results in a variety of clinical settings.
Histocompatibilty & Immunogenetics
All the subject specific units in the Histocompatibility and Immunogenetics pathway will be delivered by UoM, with the exception of Haematological Malignancies and Transplantation, which will be delivered at MMU.
Year 2
To be fully compatible with the MSC curriculum these two units delivered in year 2 each nominally contain 5 credits of research methods generic content.
Histocompatibility (15 credits): The overall aim of this unit is to provide students with knowledge and understanding of the scientific basis of organ transplantation. They will understand the clinical preparation of patients for organ transplantation and the principles and practice of immunogenetics. They will become familiar with methods that support transplantation and gain experience of the interpretation of patient results in a variety of clinical settings. In addition, this unit will provide students with an appreciation of study design, an introduction to the basic principles of epidemiology and evidence based practice (nominally 5 credits of generic material).
Immunodeficiency & Immunotherapy (15 credits): This unit will equip students with a knowledge and understanding of the principles and practice of immunotherapy. In addition, it will provide students with knowledge of the scientific basis of immunodeficiency and an understanding of the clinical investigation of a range of immunodeficiency. The unit will also provide students with an introduction to the use of biostatistics in data analysis (nominally 5 credits of generic material).
Year 3
In year 3 there is one 30 credit unit called Advanced Histocompatibility and Immunogenetics, which comprises three 10 credit modules.
Hypersensitivity & Allergy (nominally 10 credits): This unit will equip students with knowledge of the scientific basis of hypersensitivity and allergy and an understanding of the clinical presentation and investigation of common disorders associated with each.
Haematological Malignancies & Transplantation (nominally 10 credits): This unit equips students with knowledge and understanding of the pathophysiology, clinical presentation and management of patients with haematological malignancies. Furthermore, the unit will provide students with knowledge of the scientific basis of organ transplantation and an understanding of principles and practice of organ transplantation.
Haemopoetic Stem Cell Transplantation (nominally 10 credits): This unit will equip students with a knowledge and understanding of stem cell donation, testing, harvesting and monitoring and a common clinical disorders associated with stem cell transplantation.
Haematology & Transfusion Science
At the beginning of year 2 students on this pathway switch their registration from UoM to MMU, which means they will come under the postgraduate rules and regulations employed by MMU. All taught units in years 2 and 3 of the Haematology pathway are delivered by MMU. In addition the research project will be overseen by MMU.
Year 2
Research Methods (10 credits): This unit will provide students with an appreciation of study design, an introduction to the basic principles of epidemiology and evidence based practice. The unit will also provide students with an introduction to the use of biostatistics in data analysis.
Clinical Haematology (10 credits): This unit will equip students with knowledge and understanding of a range of disorders the pathophysiology and clinical presentation of a range of disorders associated with abnormalities of red cells, white cells and other haemostatic factors.
Transfusion 1 (10 credits): This unit will provide students with knowledge of blood groups and their clinical significance. Furthermore, it will give students a critical appreciation of the regulatory frameworks and safety issues associated with blood transfusion and handling of blood products.
Year 3
Haematological Malignancy (10 credits): This unit equips students with knowledge and understanding of the pathophysiology, clinical presentation and management of patients with haematological malignancies.
Haemostasis (10 credits): This unit will provide students with a knowledge and understanding of pathophysiology and clinical presentation of a range of acquired and genetic bleeding and thrombotic disorders.
Transfusion 2 (10 credits) This unit is designed to provide students with a knowledge and understanding of the essential concepts of transfusion science and the strategies and methods for laboratory diagnosis and treatment of transfusion related and immune disorders.
Research Project and Dissertation (60 credits)
This permits students to develop and refine core research and transferable skills in addition to expanding their knowledge and understanding of either: clinical biochemistry, clinical immunology, histocompatibility & immunogenetics, or haematology & transfusion science.
The research project will usually be completed during years 2 and 3 of the course. The project can be undertaken full-time over 8-10 weeks or a part-time over an extended period. The programme expects employers to allow students sufficient “protected” time to complete their projects within the time frame outlined above. If a student is having difficulties he/she should immediately contact their Personal Advisor or the Programme Director.
At the end of the research project you will have to produce a dissertation. You should expect some help from your project supervisor in writing the report. Obviously, the extent of this help may be reflected in the final mark, but as a rule your project supervisor will be expected to read and comment on a first draft of the report. You should however provide your supervisor with adequate notice when submitting your draft report since they have many calls on their time. You will find it helps to prepare figures and to work on aspects of your report throughout your research project, rather than leaving it until the end before you start writing.
It is important to remember that one of your markers will not be closely aware of your projects. It is therefore important to provide clear and concise write-ups. Given that projects will vary in the number and size of figures/images, the fairest and most consistent method to standardise the length is to impose a word limit.
Please refer to the Blood Science dissertation handbook for guidance on Masters level dissertations. The dissertation handbook can be found on the Community Space on Blackboard.
For any mitigating circumstances relating to the research project and dissertation, please refer to the Mitigating Circumstances Guidance for Students: http://www.tlso.manchester.ac.uk/map/teachinglearningassessment/assessment/sectionc-reachingdecisionsfromassessment/mitigatingcircumstancesguidanceforstudents/
3. Teaching, Learning and Assessment
Coursework and Assessment
Please refer to your Blackboard unit spaces for more information regarding coursework and assessment, including submission deadlines: https://my.manchester.ac.uk/
Postgraduate Taught Degree Regulations for Students
Students should familiarise themselves with the degree regulations for Postgraduate Taught Degrees by clicking on this link http://www.regulations.manchester.ac.uk/postgraduate-degree-regulations/ or reading the University document here: Introduction to the Postgraduate Degree Regulations for Students
Please note that students cannot progress to the MSc Paediatric Anaesthesia dissertation unless they have successfully completed 120 credits at Masters Level.
Programme Exemptions to PGT Regulations
Please be aware that the MSc Clinical Science (Blood Science) has some higher requirements to the University degree regulations and details of these are outlined below.
The programme employs a 50% pass rate across all levels & pathways (i.e. PGCert/PGDip/MSc).
The programme does not permit compensation rules to be applied to any course unit.
As per professional body requirements resit pass marks will be recorded on the transcripts as 50R. However the actual awarded mark as described in the ‘Reassessment’ section above (i.e. 40-49R) will be used to calculate the overall weighted average and degree classification.
Guidance for Presentation of Taught Masters Dissertations
The University of Manchester guidance on presentation of taught Masters Dissertations is available at:
Guidance for the presentation of Taught Masters dissertations
The guidance explains the required presentation of the dissertation, and failure to follow the instructions in the guidance may result in the dissertation being rejected by the examiners.
Detailed Format for Writing a Masters Dissertation
The dissertation should be prepared in line with the University of Manchester’s Guidance for the Presentation of Taught Masters Dissertations. The document is available via the following link: http://documents.manchester.ac.uk/display.aspx?DocID=2863
As a guide, excluding bibliography, glossaries and appendices, the length of the report should be 50 – 60 pages.
Additional information that needs to be provided with the Dissertation includes:
Introduction and aims: This section should provide information about the background to the project. The main aim of the Introduction is to inform the reader why the area of research is important, and how the project contributes to the research field. This section should end with one or two paragraphs that clearly state the overall aims (e.g. what hypothesis will be tested?) and the key objectives (e.g. what experiments will be performed?) of the project. The Introduction should be self-contained and should not require the reader to access additional material in order to understand it. Neither should it be a leisurely review of the field. It should be limited to around 6-10 pages of typescript. The referencing of reviews to cover large areas of literature is appropriate. However, research that is directly relevant to the project should be referenced in full as primary research papers. The use of figures to illustrate concepts or previous work is encouraged. It is best that figures are originals. Where unavoidable, figures may be copied or adapted from journals, in which case they must be cited in full within the legend.
In summary, it is important to identify in the Introduction:
- The research topic or area;
- The question or questions being addressed, and why they are important;
- The purpose of the project. In most cases, the project should seek to test a hypothesis. Some projects may be more observational, in which case it is important to identify how these observations will be utilised to advance the field.
Materials and Methods: This should provide a description of the experimental systems and designs employed to obtain data, the materials used (including suppliers), and the methods of data and statistical analysis. Detail should be sufficient for others to repeat the work and to demonstrate that the student has understood the methods used. The key here is to appreciate which methodologies require detailed descriptions and which standard procedures can be dealt with quickly by referencing previous publications or manufacturers’ instructions:
- There is no need to describe at length many standard laboratory procedures. For example, cell culture could be described by: “HeLa cells were grown in a 5% CO2 environment, in DMEM supplemented with 10% FBS and containing penicillin (x U/ml) and streptomycin (x U/ml).” Methods of cell splitting etc. need not be referred to unless they are intrinsic to the design of experiments.
- Many standard protocols use kits. These can be described by identifying the kit and stating that methods were followed according to the manufacturer’s instructions (with details of any modifications).
Results: A detailed description of the results and findings. These should not endlessly re-state the aims of the project but should provide sufficient information to allow the reader to ascertain the aim of each experiment/method development and what the result was. The results are often best divided into sections, each with a theme.
The text should be supported with figures and tables. These should be placed in the appropriate position within the main body of the report, i.e. immediately following the first reference to each table or figure, and not all put at the end of the report. Tables and Figures should be self-contained with appropriately detailed legends and it should normally not be necessary to describe every aspect of the table/figure in the text. There may however be occasions when you want to draw the reader to specific components of the Table/Figure (for example, “note differences between columns X and Y in Table II”, or “note the asterisked bands in lane 6 of Figure 4” etc).
Tables should be numbered consecutively. They must have an informative heading and an explanatory legend. These should make the general meaning comprehensible without reference to the text. Consider the layout carefully so the significance of the data can be grasped readily. Statistics should be quoted where appropriate. Units in which the results are expressed should be given at the top of each column.
Figures should also be numbered consecutively and should contain appropriate headings, annotations and legends. Do not make the figures over complicated by presenting too many sets of data. On graphs, each line should have a separate symbol and error bars should be shown where appropriate. Unless there are special reasons, do not present the same data in more than one form.
Discussion: The Discussion should not be a paraphrasing of the results and is normally headed only by a brief summary of your findings. The Discussion should consist of a logical flow of arguments and reasoning that explains and expands upon the results in simple English, and identifies their relevance to published findings. You will be expected here to refer mainly to primary papers in the literature. The Discussion also provides an opportunity for you to defend your conclusions, identify how experiments could have been improved upon, and to discuss how the project might develop given more time.
Conclusions: A short summary will identify whether the approaches used have been successful and whether the aims that the student set originally have been achieved.
References: There should be a single reference section at the end of the document. References must be cited in full (all author names and initials, date, title, journal, volume, pages). References can be cited in the text either by author and date (e.g. Smith, 1996 or Smith and Brown, 1980 or Smith et al., 1990) or by numbering e.g. (34). You are encouraged to use a referencing software package such as Endnote or Reference Manager.
Acknowledgements: You may wish to acknowledge the people who have helped you in your project.
Appendices etc: Appendices are useful ways to include supplementary data (e.g. DNA sequences) without breaking the flow of the dissertation. Buffer compositions are best described in parentheses within the Methods section, but their inclusion in an appendix is acceptable. Abbreviations should be listed on a separate page, preferably after the Table of Contents. Terms that are abbreviated should be used 3 or more times in the text. They should be written in full the first time they are used, followed by the abbreviation in parenthesis.
Turnitin and Plagiarism
Plagiarism and Other Forms of Academic Malpractice
Academic malpractice is any activity - intentional or otherwise - that is likely to undermine the integrity essential to scholarship and research. It includes plagiarism, collusion, fabrication or falsification of results, and anything else that could result in unearned or undeserved credit for those committing it. Academic malpractice can result from a deliberate act of cheating or may be committed unintentionally. Whether intended or not, all incidents of academic malpractice will be treated seriously by the University.
The Faculty of Biology Medicine and Health have designed a learning module to raise your awareness of academic malpractice and how it can occur in general writing during your studies. This resource can be accessed via Blackboard - SMS Introductory Course and must be completed before you submit your first piece of academic writing for assessment.
The University provides workshops and online training via My Learning Essentials
Please refer to the University of Manchester guidance to students on plagiarism and other forms of academic malpractice
The full guidance document can be viewed here: http://documents.manchester.ac.uk/display.aspx?DocID=2870
Academic Malpractice: Procedure for the Handling of Cases can be found at: http://documents.manchester.ac.uk/DocuInfo.aspx?DocID=639
Turnitin
The University uses electronic systems for the purposes of detecting plagiarism and other forms of academic malpractice and for marking. Such systems include TurnitinUK, the plagiarism detection service used by the University.
As part of the formative and/or summative assessment process, you may be asked to submit electronic versions of your work to TurnitinUK and/or other electronic systems used by the University (this requirement may be in addition to a requirement to submit a paper copy of your work). If you are asked to do this, you must do so within the required timescales.
The School also reserves the right to submit work handed in by you for formative or summative assessment to TurnitinUK and/or other electronic systems used by the University.
Please note that when work is submitted to the relevant electronic systems, it may be copied and then stored in a database to allow appropriate checks to be made.
Mitigating Circumstances
Mitigating circumstances are personal or medical circumstances which are unforeseeable and unpreventable that could have a significant adverse effect on your academic performance. You should only submit a mitigating circumstances application if you consider it serious enough, and the timing critical, to have affected your performance in your assessed work and examinations.
Request for mitigation must be submitted to your programme administrator, in advance of your assessment submission deadline or exam. Requests for mitigation submitted after the assessment or exam (except those requests made as a result of circumstances that have arisen during the course of that assessment period) will not be considered without a credible and compelling explanation as to why the circumstances were not known before the beginning of the assessment period or why you were unable to complete or submit an application prior to the assessment or exam. Please note that not informing the University of circumstances due to personal feelings of embarrassment and pride, or having concerns over the confidential treatment of requests for mitigation, are not considered to be credible and compelling explanations
All mitigating circumstances applications must be supported by independent third party evidence. The type of evidence required will vary according to the nature of the circumstances. Examples of evidence include a doctor or other health professional’s letter, counsellor’s letter, self-certification form signed by your GP or GP’s Medical Practice (for illnesses of 7 days and under only). Please note that it is a University policy that the self-certification form must be signed by a GP; we cannot accept forms which have not been signed by a GP. Please note that if evidence has not been received within 2 weeks of the submission of your form, and you have not contacted them to inform them of any delay, your application will be refused and no further action will be taken.
Please ensure that you password protect or encrypt your mitigating circumstances form and supporting evidence before sending to your programme administrator.
Any requests for mitigation will be considered confidentially by a mitigating circumstances panel or sub-panel. Where a request for mitigation is supported, a recommendation will be made to the exam board for them to decide on the best course of action for the student.
You are advised to consult the following guidance, which directs you to seek advice and support before and whilst submitting a request for mitigation.
The University form and guidance for students is available on the web: A Basic Guide to Mitigating Circumstances.
For further information about the process and acceptable grounds for mitigation see: Mitigating Circumstances Policy & Procedures: http://documents.manchester.ac.uk/DocuInfo.aspx?DocID=4271
Please be advised that any requests need to be submitted by midday the day before the pre-arranged Mitigating Circumstances meeting.
23rd October 2019
27th November 2019
8th January 2020
19th February 2020
18th March 2020
22nd April 2020
20th May 2020
17th June 2020
Late Submission Penalty (Including Dissertation)
Work submitted after the deadline without prior approval will be subject to a late penalty in accordance with the University Policy on Submission of Work for Summative Assessment on Taught Programmes. The penalty applied is 10% of available marks deducted per day/24 hours (from the time of the original or extended deadline), until the assignment is submitted or no marks remain.
Penalties for late submission relate to 24 hours/calendar days, so include weekends and weekdays, as well as bank holidays and University closure days.
The mark awarded for the piece of work will be reduced by:
10% of the available marks deducted if up to 24 hours (1 day) late
20% of the available marks deducted if up to 48 hours (2 days) late
30% of the available marks deducted if up to 72 hours (3 days) late
40% of the available marks deducted if up to 96 hours (4 days) late
50% of the available marks deducted if up to 120 hours (5 days) late
60% of the available marks deducted if up to 144 hours (6 days) late
70% of the available marks deducted if up to 168 hours (7 days) late
80% of the available marks deducted if up to 192 hours (8 days) late
90% of the available marks deducted if up to 216 hours (9 days) late
100% of the available marks deducted if up to 240 hours (10 days) late
If the assessment is submitted within 10 days of the deadline the assessment should be marked and feedback to the student provided. If this mark before the penalty is applied reaches the appropriate pass mark but the applied penalty results in a fail of the assessment, the student should not be required to resit the assessment as the original mark can be taken as the resit mark. Further information and examples can be found in the Policy and associated Guidance documents.
For work submitted more than 10 days late, it is regarded as a non-submission and need not be marked. In this case a mark of zero will be awarded and normal resit regulations will apply.
The sliding scale should only be applied to first-sit submissions. For all referred (resit) assessment, any late submission will automatically receive a mark of zero.
For further information:
Policy on the Submission of Work for Summative Assessment on Taught Programmes
Assignment Word Count (Including Dissertation)
In accordance with the University Policy on Marking:
Each written assignment has a word limit which you must state at the top of your first page. It is acceptable, without penalty, for you to submit an assignment within a range that is plus 10% of this limit. If you present an assignment with a word count exceeding the specified limit+10%, the assignment will be marked but 1% will be deducted from this mark for every 100 words over the limit given.
For an original word limit that is 1000 words and an assignment that is marked out of 100. If a submission is made that is 1101 words then it exceeded the 10% leeway, and is more than 100 words over the original limit and should receive a 1 mark deduction.
In accordance with accepted academic practice, when submitting any written assignment for summative assessment, the notion of a word count includes the following without exception:
- All titles or headings that form part of the actual text. This does not include the fly page or reference list
- All words that form the actual essay
- All words forming the titles for figures, tables and boxes, are included but this does not include boxes or tables or figures themselves
- All in-text (that is bracketed) references
- All directly quoted material
Certain assessments may require different penalties for word limits to be applied. For example, if part of the requirement for the assessment is conciseness of presentation of facts and arguments. In such cases it may be that no 10% leeway is allowed and penalties applied may be stricter than described above. In such cases the rules for word count limits and the penalties to be applied will be clearly stated in the assessment brief and in the submission details for that assessment.
Academic Appeals, Complaints, Conduct and Discipline
Academic Appeals
- Students have a right of appeal against a final decision of an Examination Board, or a progress committee, or a graduate committee or equivalent body which affects their academic status or progress in the University.
- Students thinking of appealing should first discuss the matter informally with an appropriate member of staff, in order to better understand the reason for the result or decision.
- Should you wish to proceed to a formal appeal, this must be submitted within the timeframe outlined in the Academic Appeals Procedure to the Faculty Appeals and Complaints Team, Room 3.21, Simon Building, University of Manchester, M13 9PL (e-mail: FBMHappealsandcomplaints@manchester.ac.uk).
- The Academic Appeals Procedure (Regulation XIX) and associated documents, including the form on which formal appeals should be submitted, can be found at www.regulations.manchester.ac.uk/academic
Student Complaints
- The University’s Student Complaints Procedure (Regulation XVIII) and associated documents, including a complaints form, can be found at www.regulations.manchester.ac.uk/academic
- The University has separate procedures to address complaints of bullying, harassment, discrimination and/or victimisation - see https://www.reportandsupport.manchester.ac.uk/
- Students thinking of submitting a formal complaint should, in most instances, attempt informal resolution first (see the procedure). Formal complaints should be submitted on the relevant form to Faculty Appeals and Complaints Team, Room 3.21, Simon Building, University of Manchester, M13 9PL (e-mail: FBMHappealsandcomplaints@manchester.ac.uk).
Conduct and Discipline of Students
- General University information on the conduct and discipline of students can be found at www.tlso.manchester.ac.uk/appeals-complaints/conductanddisciplineofstudents/
- Faculty policies for students on communication and dress code, social networking. and drugs and alcohol can be found at:
- http://documents.manchester.ac.uk/display.aspx?DocID=29038 (Communication and Dress Code)
- http://documents.manchester.ac.uk/display.aspx?DocID=29039 (Drugs and Alcohol)
- http://documents.manchester.ac.uk/display.aspx?DocID=29040 (Social Networking)
- Information on Academic Malpractice and how to avoid it can be found at http://www.regulations.manchester.ac.uk/guidance-to-students-on-plagiarism-and-other-forms-of-academic-malpractice/
- In accordance with the Policy on Submission of Work for Summative Assessment on Taught Programmes, ‘All typed summative assessment, including dissertations, should be submitted online and subjected to plagiarism detection software, where appropriate’.
Preparing for Your Exams
Practice exam questions will be made available to you within the appropriate course unit space on Blackboard.
All aspects of the course unit are eligible for assessment/examination unless stated otherwise by the programme director. On some occasions speakers/lecturers may advise you that particular elements are not examinable – PLEASE IGNORE THIS! However, please note it is not appropriate for us to offer specific guidance on what will and will not be examined.
Do:
- Ensure you arrive at least 15 minutes before the exam start time.
- If you are delayed and may not be able to arrive for the exam start time please notify the programme team.
- ALWAYS BRING A CALCULATOR; your invigilator will be able to advise you at the start of the exam whether or not calculators are permitted for that paper. NB It is not the University’s responsibility to provide calculators in an examination.
Exam Timetable Information, Locations and Equipment
All exams except for Year 1 Professional Practice* are arranged by the programme team. Therefore, details of your Exam date, location and time will be made available by your programme administrator normally through the programme community space on Blackboard / via email during the academic year.
*The location for the Year 1 Professional Practice exam will also be shown in your My Manchester area as the exam is arranged by the University Exams team.
We aim to make grades available within 15 working days of the assignment submission or exam date. We aim to give feedback on written assignments (feedback may be sent by either academic or administrative staff). Feedback comments for Examinations are available on request.
Grades for all assessed work are released via the Campus Solutions Student System which can be accessed via the My Manchester area https://my.manchester.ac.uk.
Within the Student System navigate via Self Service>Student Center>Academics>Assignments
All grades are subject to final ratification at Examination Board.
If you are unable to sit an Examination or feel that your ability to revise / prepare for an Examination has been affected, then you must notify your programme administrator before the Exam date.
A mitigating circumstances form and appropriate evidence (e.g. medical certification) will need to be submitted to your programme administrator. Students with approved mitigating circumstances may be offered the opportunity to sit the Examination at a later date to be agreed by the Programme Director. Where students with approved mitigating circumstances decline the option of deferring their examination there will be no adjustment applied to the mark obtained, however if the student achieves a mark below 50 (i.e. fail mark) the student may be allowed to re-take the examination at a later date as a first attempt without penalty.
4. Student Progression
Monitoring Attendance and Wellbeing of Students
The programme director and teaching staff will monitor the work and attendance of students on the programme. This is for your benefit and helps to ensure you are coping with the work. Regular or a pattern of non-attendance and/or engagement will result in you being contacted by the School to meet with your programme director. Following this, further action will be taken if there isn’t a significant improvement in attendance.
For further information see:
Regulation XX Monitoring Attendance and Wellbeing of Students
The University offers a range of advice and support to students experiencing problems with attendance. The A-Z of Services can be found on the MyManchester website. Here you can find a information on a wide range of topics such as library services, disability support and careers advice.
You can also speak to your Programme Director and/or Academic Advisor.
What to do if you are absent
In case of illness you should supply a doctor’s certificate or, if the illness is brief, a self-certification. If you are absent for other reasons then you should write a letter to the Programme Director explaining the circumstances. Medical certificates or letters should be given in person or sent to the Programme Administrator. Whatever your reason for being away, tell your supervisor about it and make any necessary arrangements to catch up with work you have missed.
Special Permissions
Interruptions to programme and extensions to writing up
It is the expectation of the University that postgraduate taught students pursue their studies on a continuous basis for the stipulated duration of their programme. However, it is recognised that students may encounter personal difficulties or situations which may seriously disrupt or delay their studies. In some cases, an interruption or extension to your programme of study may be the most sensible option.
Students who wish to interrupt the programme or extend to write up the dissertation should initially discuss their plans and reasons with the Programme Director and/or their Academic Advisor.
Students should also provide documentary evidence when appropriate, for example, doctor’s letter, sick note etc.
The forms required for formal application are available from your Programme Administrator.
Withdrawal from the Programme
Students who are considering withdrawing from the programme should discuss this in the first instance with the Programme Director.
If arrangements for withdrawal need to be made, this will be handled by the Programme Administrator, who will manage communication with the Fees and Records Departments and other University bodies as appropriate OR Students may liaise directly with the Programme Administrator who will communicate this information directly to the University Student Services Centre.
5. Student Support and Guidance
Student Support and Guidance
Student support and guidance within the programme
Support and advice is available to all students both formally and informally from the Programme Directors, the Programme Administrator and research project supervisors.
If you have any queries or would like to discuss any issues at all – academic, administrative, technical or personal – please do not hesitate to get in touch. All personal issues will be dealt with confidentially.
If we are unable to help you directly, we can put you in touch with many of the support services that are available to students of the University through our Student Services Centre. You can approach these services independently, without the involvement of programme staff. Use the A-Z of Student Services Guide as an additional source of information.
Student support for the dissertation
During the research project and writing up of the dissertation, students will have individual support from their research project supervisor and scheduled structured sessions to monitor their progress and provide support, with help being offered if any problems are being encountered. In addition, students are made aware that they have the option of contacting the programme directors at any time if they are experiencing difficulties, whether this is in relation to their project, or indeed, with regard to any other issue of relevance.
Student support from the University
The University offers a range of support and guidance services to students, for example, Student Health Service, Student Union Advice Centre, Student Counselling and Careers Advice. Details of all these services can be obtained from the A-Z of Student Services
Counselling Service
The Counselling Service is available for all students. It is free and consists of a team of professional counsellors. The service provides confidential counselling for anyone who wants help with personal problems affecting their work or well-being.
The service is open 9.00am to 5.00pm Monday to Friday all year round except public holidays.
Occupational Health
The Occupational Health service is a specialised area of medicine concerned with the way in which an individual’s health can affect his or her ability to do a job and to study and conversely how the work environment can affect an individual’s health. Their aim is to promote the physical, mental and social well-being of students and to reduce the incidence of ill-health arising from exposure to work place hazards.
Students Union Advice Centre
The Students Union has advisers who can help with any matter ranging from finances to housing and beyond. On the South Campus, the Advice Centre is on the first floor in the Student Union Building, and is open Monday to Friday, 10.00am to 4.00pm, term time and vacation. There is no need to make an appointment.
Academic Success Programme
You’re studying at the University of Manchester – congratulations! Writing and speaking Academic English can be challenging, even for native speakers. Our team of experienced tutors are here to support you, and will help boost your confidence to work independently in English through a series of interactive workshops - freely available to all University of Manchester students.
To find out more, and to register, please go to www.manchester.ac.uk/academicsuccessprogramme
Personal Advisor
Each student will be allocated a personal advisor whose responsibility will include pastoral care in addition to mentoring and monitoring the student’s academic and personal development progress during the programme. Students should make every effort to meet/contact their advisors at least every 3 months to discuss any problems. The progress of the project will also be discussed at these meetings (as well as progress on the programme more generally) but the supervision of the project is the responsibility of the project supervisor.
Disability Advisory and Support Service (DASS)
The University of Manchester welcomes students with a disability or specific learning difficulties. The University has a Disability Advisory and Support Service, who can supply further information and DASS advisors will be pleased to meet you to discuss you needs. DASS will liaise with your School through the Disability Coordinator to make the necessary arrangements for your support during your time in Manchester.
The DASS office can also provide a copy of the University’s Disability Statement, ‘Opportunities for Students with Additional Support Needs at the University of Manchester’ which sets out the policy and provision for students with a disability.
DASS Contact Details:-
Location: 2nd Floor, University Place
Email: dso@manchester.ac.uk; Phone: 0161 275 7512
Text: 07899 658 790; Website: www.dso.manchester.ac.uk/
Disability Coordinator Contact Details:-
Name: Kay Gardner (0161 306 7978) & Wiktoria Obidniak-Marciniak (0161 306 5519)
Email: kay.gardner@manchester.ac.uk or wiktoria.obidniak-marciniak@manchester.ac.uk
Religious Observance and Looking after yourself and your patients during Ramadan
Policy on Religious Observance:
- University Policy
- The Faculty of Biology, Medicine and Health has produced guidance for healthcare students on fasting and caring: Fasting and Caring - Looking after yourself and your patients during Ramadan: guidance for health care students.
6. Student Representation and Feedback
Student Representation and Feedback
Students, in consultation with the Programme Administrator, should arrange an informal election of their Student Representative near the beginning of the academic year. If more than one person is interested in the role, then each candidate is asked to write a short proposal which is circulated to the student body, and an election is held.
The overall responsibilities of the Student Representative are
- to liaise between staff and students about matters of concern
- to provide two-way feedback on programme and teaching quality
- to promote active student involvement in the development of the programme
- to identify student issues and needs on the programme
- to attend programme committee meetings representing the student voice
- to find effective ways to feedback the outcomes of meetings to the student body
- to attend relevant student representative training
- to liaise with other Student Representatives to gain support and ideas
- to become established as a central point for information and guidance for students in the group.
Student representatives are not required to get involved with fellow students’ personal problems, academic difficulties, or individual student allegations of unfair or inappropriate treatment.
Confidentiality is imperative when dealing with student issues. The representative is chosen by fellow students and has their trust, and must maintain it. Any discussion of an individual student’s situation with a third party requires their consent beforehand.
7. Programme Management
Programme Management and Committee Structure
Programme Management
The programme is managed and operated in accordance with the policies, principles, regulations and procedures of the University of Manchester.
Programme Directors relate to the School and Faculty Postgraduate Teaching Committees on matters relating to admissions, exams, reviews and approval of new programmes and units, quality assurance etc. and policy issues of broad relevance to the Graduate School.
The Programme Committee will meet each semester and consist of the Programme Director, Programme Administrator, Programme Committee members and the unit co-ordinators.
The remit of the committee will be to:
- Oversee the teaching, assessment and examining arrangements;
- Monitor cohort progression including failure rate, withdrawal rate;
- Evaluate the extent to which the learning outcomes are achieved by students;
- Monitor, maintain and enhance standards of all aspects of the programme;
- Evaluate the effectiveness of the curriculum and of assessment in relation to programme learning outcomes;
- Evaluate the effectiveness and relevance of the teaching and learning methods employed;
- Review and revise the programme in the light of any relevant Quality Assurance Agency (QAA) benchmarks, any other relevant external and/or professional requirements and developing knowledge in the subject area;
- Receive, consider and respond to feedback from students, employers and external examiners;
- Where the need for change is identified, effect the changes quickly and efficiently;
- Produce an annual action plan via annual monitoring;
- Produce reports for periodic review
- Produce relevant information for an Institutional Audit;
- Review programme documentation, e.g., programme handbooks, programme specifications, promotional literature and programme website;
- Ensure suitable and efficient arrangements are in place for recruitment, admission and induction.
Committee Structure
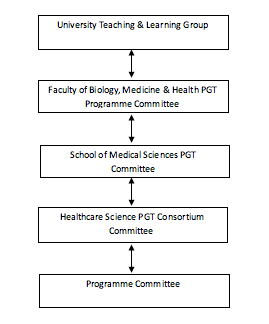
The Programme Committee acts as a curriculum development team for the Programme. The Programme Committee will report to a School, or Department, or Faculty level committee. The Programme Director is responsible for the management of the programme, and the Programme Committee is established to support the Programme Director in the carrying out of their responsibilities.
The role of the External Examiner
External Examiners are individuals from another institution or organisation who monitor the assessment processes of the University to ensure fairness and academic standards. They ensure that assessment and examination procedures have been fairly and properly implemented and that decisions have been made after appropriate deliberation. They also ensure that standards of awards and levels of student performance are at least comparable with those in equivalent higher education institutions.
External Examiners’ reports
External Examiners’ reports relating to this programme will be shared with student representatives and details of any actions carried out by the programme team/School in response to the External Examiners’ comments will be discussed. Students should contact their student representatives if they require any further information about External Examiners’ reports or the process for considering them.”
External Examiner Details
The External Examiner for this programme is Professor Sudarshan Ramachandran, Professor of Metabolic Medicine, who is based at University Hospitals Birmingham NHS Foundation Trust.
Please note that this is for information only and it is inappropriate for students to make direct contact with External Examiners under any circumstances, in particular with regards to a student’s individual performance in assessments.
Other appropriate mechanisms are available for students, including the University’s appeals or complaints procedures and the UMSU Advice Centre. In cases where a student does contact an External Examiner directly, External Examiners have been requested not to respond to direct queries. Instead, External Examiners should report the matter to their School contact who will then contact the student to remind them of the other methods available for students. If students have any queries concerning this, they should contact their Programme Administrator in the first instance.
Confidentiality, Professionalism and Information Sharing Agreement
Information in relation to a student’s academic progression will be shared amongst relevant parties in compliance with the Data Protection Act 1998 and in conjunction with contractual obligations between the parties. Relevant parties could include, but not limited to, education providers as part of the programme, funding bodies and accreditation bodies.
Examiner Meetings
For operational and administrative purposes the MSc is divided into three parts.
Part 1: Year 1 Core taught units + first examiners meeting
Part 2: Year 2 Taught units + interim examiners meeting
Part 3: Year 3 Taught units and Research Project + final examiners meeting
Students who wish to leave the Programme may do so at the end of year 1 (i.e. after core taught units) with a Postgraduate Certificate in Clinical Science, or after completion of year 2 with a Postgraduate Diploma in Clinical Science (i.e. after core taught units, 30 credits of subject specific teaching and completion of a reduced 30 credit research project*). The award of a Certificate or Diploma is dependent on the student obtaining an average of at least 50% for the units taken (see below).
*The 30 credit research project would need to be submitted in early September of the year that the student would have been due to enter their final year of study.
First Examiners Meeting (June, Year 1)
The major purpose of the First Examiners’ Meeting is to ratify the provisional marks from the core taught modules and to decide which students should be allowed to progress to Part 2 of the MSc Programme (see below for details). To progress onto Part 2 and therefore stay within the MSc programme, the student must achieve a mark of at least 50% (including any units passed by referral, within the referral allowance defined by the Postgraduate taught degree regulations) for each of the year 1 Taught Units.
This meeting also provides the examiners with an opportunity to find out how students perceive the course.
Interim Examiners Meeting (June, Year 2)
A second Examiners meeting is held to ratify the provisional marks from the Year 2 taught units and to determine which students should progress onto the research project. Students must have passed all taught units at Masters level, i.e. achieved a mark of at least 50% (including any units passed by referral, within the referral allowance defined by the Postgraduate taught degree regulations) to be able to progress to the research project. Students who do not meet the criteria to remain on the Masters pathway will be considered for an alternative award (PG Certificate).
Final Examiners Meeting (June, Year 3)
During this meeting the progress of each student will be discussed. The marks from the research project dissertation will be combined with the taught unit marks to provide a final weighted average percentage score. The panel will then recommend the student be awarded.
Please note the MSc Programme Director, MSc Programme Committee or the Graduate Office are not permitted to disclose the recommendations made at the Final Examiners’ meetings.
8. Learning Resources
Learning Resources
Libraries
All registered students may become members of the University of Manchester Library on the main campus.
Up-to-date news about the library is available here.
IT Services and eLearning
IT Services Support Centre online
Details of what IT support is available and how to access it can be found on the FBMH eLearning Support page.
Login to the Support Centre online to log a request, book an appointment for an IT visit, or search the Knowledge Base.
Telephone: +44 (0)161 306 5544 (or extension 65544). Telephone support is available 24 hours a day, seven days a week.
In person: Walk-up help and support is available at the Joule Library, Main Library or Alan Gilbert Learning Commons:
Use Support Centre online for support with eLearning, from where you may make a request, report a fault, or search the Knowledge Base. The email address is: elearning@manchester.ac.uk
Blackboard
Blackboard, the University's 'virtual learning environment', will be used for online teaching.
What is Blackboard?
Blackboard is a web-based system that complements and builds upon traditional learning methods used at The University of Manchester. By using Blackboard you can
- view course materials and learning resources,
- communicate with lectures and other students,
- collaborate in groups,
- get feedback
- submit assignments
- monitoring your own progress at a time and place of your own convenience.
Training in the use of software
The Faculty eLearning team have produced a short introduction to Blackboard for new students. The recording is hosted in two places: the VLS and on YouTube:
The recording is just over seven minutes long and covers most of the commonly used tools in Blackboard.
9. Useful Links
Academic and Student Support Policies
Academic Support Policies
A full list of University Policies and documents
Academic Appeals (Regulation XIX)
Academic Malpractice: Procedure for the Handling of Cases
Basic Guide to Student Complaints
Conduct and Discipline of Students (Regulations XVII)
General University information on the Conduct and Discipline of Students
Faculty policies for students on Communication and Dress Code, Social Networking and Drugs & Alcohol can be found at:
Information on Academic Malpractice and how to avoid it
Guidance for the Presentation of Taught Masters Dissertations
Guidance to Students on Plagiarism and Other Forms of Academic Malpractice
Policy on Submission of Work for Summative Assessment on Taught Programmes
Policy on Mitigating Circumstances
Mitigating Circumstances Guidance for Students
Policy on Feedback to Undergraduate and Postgraduate Taught Students
Work and Attendance of Students (Regulation XX)
Blackboard
Students should access Blackboard via My Manchester
Disability Advisory and Support Service
University Language Centre – Study English - Tel: 0161 306 3397
Equality, Diversity and Inclusion for Staff and Students
Occupational Health Services for Students
