ClinPsyD Handbook: Your guide to the ClinPsyD Programme
Welcome to the 2021-2022 ClinPsyD Handbook!
This online resource is an indispensable guide to the Manchester Clinical Psychology Doctorate and our various rules, processes and procedures. Please click on the links to the left to find out more about different aspects of the programme.
Guidance on Covid
Last updated: 24th September 2021
The University has a dedicated webpage pertaining to Covid, which includes advice about keeping safe on campus, what to do if you have symptoms of Covid or have tested positive for the virus and so on. This is your primary source of information about Covid and should be checked on a regular basis.
PLEASE NOTE: If you have tested positive for Covid 19 or have had to self-isolate then you MUST report this immediately by completing the Online Reporting Form, you must also email Tracey Hepburn so that she can inform GMMH.
GMMH emails and guidance
Please ensure that you are checking your Trust email account on at least a weekly basis. Aside from being one of the general expectations of you as a Trust employee, it is particularly important at the current time so that you have access to the most up to date guidance in relation to Covid. The Trust also has a dedicated section of their website that provides guidance for staff in relation to coronavirus.
Attending teaching
For the time being, we expect most teaching sessions to be delivered face to face, although there may be occasions where lectures are delivered remotely via Zoom. We will inform you about these via the timetable or email as needed. Guidance about accessing and using Zoom is available in the ClinPsyD General Information folder on Canvas.
The university has agreed that the default position this academic year is that social distancing is not required in lecture rooms. However, there is a contingency plan to reintroduce social distancing if required. You should be mindful of maintaining social distancing in other areas of campus where possible.
In order to reduce the risk of Covid transmission we expect students to wear face coverings during teaching and when moving around indoors. Students are encouraged to use hand sanitiser and wipes will be made available in all lecture rooms for wiping down equipment/surfaces where applicable.
The university also recommends taking twice weekly lateral flow tests. Testing kits will be available for collection from catering outlets across campus. Vaccination remains the most effective way of protecting yourself and other people; if you have not received your Covid vaccine yet then we strongly recommend that you consider this.
Placements
Please speak to your supervisor about local expectations regarding face-to-face and remote working, social distancing and mask wearing.
All aspects of placement related activity and any concerns you have about this can also be discussed with your clinical tutor or one of the clinical tutor team.
Assessments
For the time being, students should work on the assumption that all of the normal assessment processes and procedures will be followed this academic year, including live observations, case reports, exams, audits of clinical activity, placement assessment and the LSRP. Given the situation with Covid, however, the precise timing and format of assessments may be subject to change. For example, live observations may need to be conducted remotely via Zoom and the format of the exams may need to be adjusted so that they are delivered remotely as open book assessments. Wherever we make changes, we will ensure that the objectives, focus and content of assessments map as closely as possible to the originals. We will also confirm the details of any changes no less than three months before each assessment period.
Research
The Doctoral Academy are providing detailed advice about postgraduate research during the pandemic. This includes information about including Covid impact statements in theses (so that examiners are made aware of any disruption caused by Covid and can accommodate this in their assessment) guidance on rescoping projects affected by Covid, and what to do if your research necessitates face to face contact with people during the pandemic (which may require additional governance approvals).
If you are experiencing on-going delays with your project then please discuss this with your research supervisor ASAP and consider raising your concerns with Dan Pratt.
Staff availability
Most of the team will be returning to campus during semester 1 but many members of staff will be working from home at least some of the time. This may mean that they are difficult to contact on their usual University telephone numbers. If you want to speak to someone, please email them and they can set up a meeting as necessary.
Information about which other areas of campus are open should be available on the University Covid page.
Trainees with carer responsibilities
We are sympathetic to the fact that trainees with childcare or other carer responsibilities may face additional challenges due to the coronavirus pandemic. If this is an issue for you then please discuss it with your clinical tutor in the first instance.
Well-being
This is a very difficult time for us all and it is important that we look after ourselves and each other. Please see the section on trainee well-being for information about specific sources of support. We are also offering regular drop-in slots for trainees (look out for emails about these) and James Lea has been circulating additional advice about maintaining well-being.
General note
We try to keep the handbook content up to date as far as possible. If there are any substantive changes we will do our best to notify you of these as and when they happen. Please note that the majority of the information presented in the rest of this handbook represents “normal” practice on the ClinPsyD. However, there may be some variations in this as a result of the ongoing coronavirus pandemic. We will communicate with you as soon as possible if there are any changes to assessments or teaching as a result of the pandemic.
If you are in any doubt about current requirements for assessment, placement, research or whatever then please contact the appropriate person.
END OF COVID-SPECIFIC SECTION
Welcome from the Head of School, Professor Kay Marshall
I am writing to welcome you to the University of Manchester and I hope you settle into University life soon, in fact, we will all be settling into our ‘new normal’ as we as staff members of the University physically re-join our community – so it will be an interesting time for us all! Rest assured the University has and is working hard to keep our community safe, however, we all have to exercise personal responsibility regarding our behaviours in attempting to slow the spread of Cv-19.
You are joining the Division of Psychology and Mental Health as you study for your Doctorate in Clinical Psychology; your Division sits in the School of Health Sciences which I have the pleasure to head up. Our School encompasses your own Division plus Human Communication, Development & Hearing; Informatics, Imaging & Data Sciences; Nursing, Midwifery and Social Work; Pharmacy & Optometry; Population Health and Health Services Research & Primary Care. So you can see that our School covers a range of disciplines all dedicated to improving health by performing excellent research of the quality that contributes to this University being recognised as one of the best Universities in the world. In the School of Health Sciences our research feeds into improving healthcare and just as importantly our teaching to ensure that your course is future proofed as you are taught by leading researchers and educational specialists.
In Health Sciences we are well aware of the importance of maintaining good mental health as well as physical health and we ascribe parity of esteem to both. During this crisis our teaching and research across the wide array of areas encapsulated by ‘mental health’ have become recognised by many as increasingly important and it is perhaps an understatement to say that we need excellent practitioners in Clinical Psychology more than ever as the impact of the pandemic will no doubt last longer than the infect itself.
I hope that you make the most of your time at the University as it has much to offer – even in these peculiar times where not only teaching has changed but we have also adapted many other activities to fit an on-line format. So do make the most of Manchester and the fantastic University you are joining.
Professor Kay Marshall B.Pharm., FRPharm.S., PhD., MBA, FHEA, FBPhSHead of the School of Health Sciences, Vice Dean of the Faculty of Biology, Medicine & Health
Clinical Psychology Training at Manchester
Information for International Students
International students should be aware that whilst they are not employed by the NHS, they are subject to the same terms and conditions as funded trainees. All procedures should be followed by all trainees regardless of their funding status, for example, booking annual leave, completing monthly returns etc.
Programme Specification, Core Purpose & Philosophy
This statement of the Programme’s core purpose and philosophy was developed in collaboration with stakeholders, and involved consultation with departments associated with the Programme. The Doctorate in Clinical Psychology is a three-year programme of academic and clinical training offered within the Division of Psychology and Mental Health and is the result of close collaboration between the University of Manchester and clinical psychologists working within the North West. The Programme aims to train practitioners in a range of settings, and to thrive in an environment where multi-professional networks are important. We recognise that the majority of graduates will be employed within the National Health Service; thus the Programme is geared to train clinical psychologists who will be able to meet client needs and the organisational requirements of the NHS and other statutory and voluntary bodies who work in collaboration with the health service. Our staff, trainees and graduates are also expected to adhere to the principles and values of the NHS as set out in the NHS Constitution (see below).
The over-arching learning outcomes of the Programme are for students to:
- acquire appropriate theoretical and academic knowledge
- acquire appropriate clinical and practical skills
- acquire knowledge of the appropriate professional and service structures and standards
- acquire appropriate research and evaluation skills
These objectives are achieved through: (a) lectures, workshops and seminars; (b) private study; (c) supervised clinical placements and a service-related project (SRP); (d) research practice, including the presentation of a doctoral thesis; (e) reports of clinical activity in the form of case reports and an audit of clinical activity (ACA); and (f) live observation of clinical skills. Collectively, these will involve exposure to a wide range of experienced clinical psychologists and other professionals, mainly based in the North West.
Central to the role of the Clinical Psychologist is the capacity to understand varied and complex psychological theories and apply these by formulating clinical situations and planning intervention strategies. The Programme is largely cognitive-behavioural in orientation with the emphasis on the role of the clinician as scientist-practitioner. Three other “core” approaches are also taught on the programme: Psychodynamic Interpersonal Therapy, systemic therapy and clinical neuropsychology, which are integrated within the empirical framework of clinical psychology as an applied science.
Our approach to clinical work emphasises full assessment and case formulation through the generation and testing of clinical hypotheses, and the ability to evaluate clinical effectiveness. The Programme acknowledges the complex and changing health care environment, and endeavours to:
- encourage students to reflect on the challenges associated with psychological treatment as an interpersonal activity;
- build awareness of the importance of direct experience in all areas of learning, such as engaging in role plays (which are a condition of entry to the programme);
- recognise the importance of evidence based health care within the NHS, and of the views of local health care commissioners and Health Education North West; and
- remain sensitive to changes in health care needs and the organisation of service delivery, and how these changes are reflected in the training needs of students.
Overview of Learning Outcomes
The Clinical Psychology Doctorate (ClinPsyD) is a practitioner doctorate that equips graduates to work as a Clinical Psychologist in the NHS. As a postgraduate degree of the University of Manchester, the Programme is designed to be consistent with the learning outcomes of the Faculty of Biology, Medicine and Health, to provide learning opportunities for the attainment of appropriate knowledge, skills and professional attitudes and to foster the student’s development as a self-motivating, self-reflecting practitioner. As a postgraduate degree, the Programme aims to ensure that trainees are able to use doctoral-level skills in accessing up-to-date, specialist knowledge, critically analyse research and demonstrate a doctoral level of research skill that will enable them to contribute to professional knowledge. The Programme aims to foster the development of practitioners who will show excellence and innovation in the use and further development of evidence-based practice. The doctorate is run in the context of a well-established academic environment, and the research strengths and professional expertise of the staff contribute to the curriculum.
The doctorate is both approved by the Health and Care Professions Council (HCPC), which regulates doctoral training in clinical psychology nationally, and accredited as a professional qualification by the British Psychological Society (BPS). All aspects of the delivery and learning outcomes of the programme are designed to be in accordance with the HCPC’s Standards of Education and Training (SETs) and Standards of Proficiency (SOPs) for Practitioner Psychologists, which underlie the programme’s learning outcomes. Successful completion of the programme enables graduates to call themselves a Clinical Psychologist (and/or a Practitioner Psychologist), titles that are protected by law. Additionally, the BPS Standards for the Accreditation of Doctoral Programmes in Clinical Psychology provide a framework for the design and content of the Programme, while the Faculty of Biology, Medicine and Health’s learning outcomes are integral to the way in which the Programme is provided in order to foster generic academic and professional skills. Due to the level and specificity of learning required, accreditation of prior (experiential) learning is not offered.
The BPS standards identify the following over-arching goals, outcomes, ethos and values for all Clinical Psychology Doctorates:
- A value driven commitment to reducing psychological distress and enhancing and promoting psychological well-being through the systematic application of knowledge derived from psychological theory and evidence. Work should be based on the fundamental acknowledgement that all people have the same human value and the right to be treated as unique individuals.
- The skills, knowledge and values to develop working alliances with clients, including individuals, carers and/or services, in order to carry out psychological assessment, develop a formulation based on psychological theories and knowledge, carry out psychological interventions, evaluate their work and communicate effectively with clients, referrers and others, orally, electronically and in writing.
- Knowledge and understanding of psychological (and other relevant) theory and evidence, related to specific client groups, presentations, psychological therapies, psychological testing, assessment, intervention and secondary prevention required to underpin clinical practice.
- The skills, knowledge and values to work effectively with clients from a diverse range of backgrounds, understanding and respecting the impact of difference and diversity upon their lives. Awareness of the clinical, professional and social contexts within which work is undertaken and impact therein.
- Clinical and research skills that demonstrate work with clients and systems based on a reflective scientist-practitioner model that incorporates a cycle of assessment, formulation, intervention and evaluation and that draws from across theory and therapy evidence bases as appropriate.
- The skills, knowledge and values to work effectively with systems relevant to clients, including for example statutory and voluntary services, self-help and advocacy groups, user-led systems and other elements of the wider community.
- The skills, knowledge and values to work in a range of indirect ways to improve psychological aspects of health and healthcare. This includes leadership skills and competencies in consultancy, supervision, teaching and training, working collaboratively and influencing psychological mindedness and practices of teams.
- The skills, knowledge and values to conduct research and reflect upon outcomes in a way that enables the profession to develop its knowledge base and to monitor and improve the effectiveness of its work.
- A professional and ethical value base, including that set out in the BPS Code of Ethics and Conduct (2018), the DCP statement of the Core Purpose and Philosophy of the profession and the BPS Professional Practice Guidelines (2017).
- High level skills in managing a personal learning agenda and self-care, in critical reflection and self-awareness that enable transfer of knowledge and skills to new settings and problems and professional standards of behaviour as might be expected by the public, employers and colleagues.
Specific outcomes
The aims of the Programme are for the trainee to acquire the necessary knowledge, skills and competencies in order to graduate at the doctoral level, gain entry into the profession of clinical psychology and be eligible to practise in the NHS. The learning outcomes have been developed in collaboration with NHS supervisors and teachers, and represent the shared views of both University and NHS staff to address the HCPC SOPs and BPS standards for accreditation. The learning outcomes also reflect the broader aims of scholarship within the Faculty of Medical and Human Sciences in providing both generic, transferable knowledge and skills and a doctoral level of research ability.
On successful completion of the programme, trainees will have:
- a basic grounding in appropriate theoretical and academic knowledge across the core areas in the field of clinical psychology, including a range of models of clinical psychology
- developed a satisfactory level of competence in the appropriate clinical and practical skills to enable the trainee to practise in the NHS; this includes the ability to implement therapeutic interventions based on knowledge and practice in cognitive-behaviour therapy and at least one other evidence-based model of formal psychological interventions;
- in-depth theoretical, academic and practical knowledge of some areas of clinical psychology
- an understanding of varied and complex psychological theories and the ability to apply these when formulating cases and planning intervention strategies
- an understanding of the appropriate professional and service structures and standards as these are applied in the NHS context
- an understanding of the central role of patients/clients and the positions and rights of all stakeholders in their own and related disciplines
- the ability to work at different levels of health care systems
- the ability to adapt skills to different settings and client groups
- an understanding of the relevance of scientific background and research skills to the work of the clinical psychologist
- an understanding of the limits of the models that they are using
- an understanding of the ethical and professional requirements of practice in clinical psychology
- the ability to communicate with patients, colleagues and the general public by oral, written or electronic means
- the ability to recognise the limits of their own competence and seek guidance as necessary
- personal and social qualities which will enable them to fulfil their professional role, including adequate interpersonal skills
- skills in time-management, self-management and team working
- the ability to recognise personal stress and ways of managing this
- the ability to independently plan, conduct and evaluate small and large scale research projects in the NHS and to be an effective consumer of research in the evidence-led culture of the NHS
- an awareness of the implications of working in a multi-cultural and multi-racial society, and awareness of equal opportunities legislation and practice
- a basic understanding of the social, political and organisational context in which they are working
- a demonstrated ability to disseminate psychological skills to other health care groups
- a plan for a career post-qualification and an understanding of the need for planning for future professional development and training, including an understanding of the NHS Knowledge and Skills Framework (KSF)
As a doctoral programme within the Faculty of Biology, Medicine and Health, the Programme aims to equip students to:
- access up-to-date specialist knowledge
- critically analyse research
- write up a piece of doctoral-level research, involving appropriate statistical techniques, as a thesis
- conduct research of publishable quality
- recognise their responsibility to advance and define professional knowledge
Summary of Components of the Programme
In order to deliver a programme which fulfils these requirements, the Programme has three main components: an academic programme, a clinical training component, and a doctoral research component. The table below sets out the aims and objectives of these components of the ClinPsyD, the teaching methods used to meet those objectives and how the objectives are assessed.
| Component of training | Aims | Objectives | Teaching Methods | Assessment of attainment of learning objectives |
|---|---|---|---|---|
| Academic | To attain the relevant knowledge of theory and practice to ensure competence to work in the NHS | Trainees will be aware of, and be able to use, relevant theory and research |
|
|
| Clinical and professional skills | To attain a satisfactory level of clinical and professional skills to ensure competence to practise in the NHS | Trainees will have met a set of specified learning outcomes in clinical work, including the ability to intervene using Cognitive Behaviour Therapy and at least one of the other core approaches to intervention on the Manchester programame (Psychodynamic Interpersonal Therapy/relational therapy; systemic therapy; Clinical Neuropsychology) |
|
|
| Research and evaluation skills | To attain sufficient competence to allow work as both a consumer and practitioner of research in the evidence-led NHS | Trainees will be competent to work as evidence-based practitioners, able to evaluate research critically and carry out small and large scale research of clinical relevance |
|
|
Breakdown of the Programme
The ClinPsyD is a full-time programme, three years in duration, and ends on 30th September of each year. The academic component of the Programme consists of a teaching programme (Wednesdays and Fridays during term time for Years 1 and 2, Mondays for Year 3 between October and January) and various ‘occasional’ workshops. Core placements are also preceded by blocks of teaching that serve as an induction to those placements, and are on every week day not otherwise dedicated to teaching or academic study. The clinical component consists of a series of placements, covering core clinical specialities, plus (where possible) a speciality of the trainee’s own choosing. Details of the allocation of time to the various components of the Programme are given below.
Overview of training by year
| Year 1 | Year 2 | Year 3 | ||||
|---|---|---|---|---|---|---|
| Block 1 | Block 2 | Block 3 | Block 4 | |||
| *Teaching | Core Adult | Core Child | Core Older Adults and Core Learning Disabilities; Health; Forensic Issues | Advanced Workshops | ||
| Placement | Adult | Child | OA or LD (or Health**) | LD or OA (or Health**) | Third Year Placement (Jan – Sept) including Service Related Project | |
| Research teaching and activity | Research teaching and planning commences | Submit research proposal; proposal agreed by Research Sub-Committee | Ethical approvals; literature reviewing | Data collection; literature reviewing | Data collection; literature reviewing | Write up and thesis ubmission, |
*Full details of the teaching programme are contained in the Programme Specification and in the Academic Curriculum section of the Programme’s intranet. In addition to the above-mentioned modules, throughout the programme there are modules in Personal and Professional Development (including Team Working and Leadership); Power, Position, Privilege and Intersectionality (formerly Diversity and Engaging the Community); Research Methods; Statistics; Clinical Neuropsychology; Systemic and Family Therapy. Trainees also engage in reflective practice groups in Years 1 and 2 and peer supervision groups in Years 2 and 3 of the Programme.
** In a limited number of cases, and where appropriate, trainees may be allocated a placement in a physical health setting during this period
1st and 2nd year term time
- Academic instruction (equivalent to 1.5 days per week)
- Clinical practice (3 days per week, which includes half a day of placement-related study)
- Academic study and research (equivalent to half a day per week)
1st year out of term time
- Academic instruction (0 days per week)
- Clinical practice (3.5 days per week, which includes half a day of placement-related study)
- Academic study and research (1.5 days per week)
2nd year out of term time
- Academic instruction (0 days per week)
- Clinical practice (3 days per week, which includes half a day of placement-related study)
- Academic study and research (2 days per week)
3rd year 1st term time
- Academic instruction (average of 1 day per week**)
- Clinical practice (0 days per week)
- Academic study and research (4 days per week)
3rd year 2nd & 3rd term time
- Academic instruction (0 days per week)
- Clinical practice (4 days per week)
- Academic study and research, including work on Service Related Project (1 day per week)
** includes a 1 week induction block at the end of October
Programme Management and Committees
Programme Team Structure and Roles
Professor Gillian Haddock is Division Lead and is the budget holder. Professor Haddock has responsibility for ensuring that appropriate strategies are developed and followed in providing a high-quality training Programme. Dr Richard J. Brown, as Programme Director, has overall responsibility for the day-to-day co-ordination and running of the Programme, and ensuring that agreed strategies and approaches are put into operation. The Programme team consists of Clinical Academics, most of whom are employed to conduct research as well as perform teaching and administrative duties on the ClinPsyD, and Clinical Tutors, whose time is dedicated to the programme. The academic and tutorial staff members each carry particular administrative duties in relation to the organisation of specific aspects of the Programme. Dr Adam Danquah, Academic Director, has responsibility for the curriculum; Dr Lara Bennett and Dr Claire Fothergill, as Clinical Co-Directors, have responsibility for placements and trainees’ clinical activity; and Dr Daniel Pratt, as Research Director, has responsibility for overseeing trainee research.
The diagram below details the programme management structure.

Programme Committees
A Programme committee structure exists to ensure that each aspect of training is well managed.
Executive Training Programme Committee
The Executive Training Programme Committee (typically referred to as “The Exec”) oversees all aspects of training, and is the overall management and quality committee for the Programme. The Exec also convenes the Examination Board. The Exec is chaired by the Programme Director, and the membership consists of all Academic and Clinical members of the Programme Team, the Trainee Advocate, trainee representatives for each year and representatives from Greater Manchester Mental Health NHS Foundation Trust and the Community Liaison Group (CLG). The Exec meets monthly, usually on the first Monday of the month. The trainee representatives are full members of the Committee and, except for personal matters affecting individual trainees, are involved in all discussions and may be asked to contribute to Sub-committee work. Trainees can also be represented by the Trainee Advocate. Exec meetings are suitable occasions for raising any matters relating to the Programme.
There are four sub-committees of the Exec (Curriculum Sub-Committee; Placement Forum; Research Sub-Committee; Equality, Diversity and Inclusion Sub-Committee), which review the four broad components of formal academic instruction, clinical training, research and equality/diversity/inclusion issues respectively.
Curriculum Sub-Committee
The Curriculum Sub-Committee is chaired by the Academic Director, who is a member of the Academic staff, and includes the Programme Director, each of the Module Organisers, representatives of all three years of trainees, and representatives from the CLG. This sub-committee is responsible for quality assurance, co-ordination and development of the academic programme. Module organisers are responsible for co-ordinating and developing their particular area, collaborating with the Academic Director and other Module organisers and responding to feedback. The Chair of the committee is responsible for collating feedback from students and staff on teaching sessions.
Placement Forum
The Placement Forum meets twice a year. It provides an opportunity for trainee representatives to discuss issues that are relevant to placements and supervision with the Clinical Tutor team. The Forum is able to take issues to the Exec for further discussion and action. Clinical Tutors are also in regular contact with the many clinical psychologists who act as supervisors for trainees from the training programme and the tutors can raise issues at the Placement Forum on behalf of supervisors. Every effort is made to make supervision as effective as possible and to maximise the learning opportunities within clinical placements. Clinical tutors maintain close relationships with supervisors through regular placement visits, supervisor training, and attendance at meetings such as the Division of Clinical Psychology Faculties (Special Interest Groups).
Research Sub-Committee
The Research Sub-Committee is chaired by the Research Director. The Research Sub-Committee is made up of ClinPsyD Programme team members, other academic supervisors who provide input into the programme, IT Support, Community Liaison Group and representatives of all three years of trainees. The sub-committee, in the form of two concurrent panels, meets on two occasions (with the second meeting being for re-submissions only) to review the research proposals submitted by trainees. Other meetings may be held outside of the scheduled meetings at the request of the RSC and/or the discretion of the Chair of the RSC; there are typically one or two such “business” meetings per year.
Equality, Diversity and Inclusion Sub-Committee
The Equality, Diversity and Inclusion (EDI) Sub-Committee was formed in early 2020 in response to growing concerns about diversity and discrimination within the profession and society more generally. This Sub-Committee was set up to articulate the programme’s vision for equality, diversity and inclusion, make recommendations around any aspect of the programme relating to EDI and monitor objectives in these areas. Our overarching goals are to eliminate discrimination and marginalisation, foster an inclusive and cohesive environment, ensure everyone feels valued and included, and ensure that diversity is valued and embodied in our staff, students, and applicants.
Quality Management and Enhancement
Internal Quality Assurance Mechanisms
Doctoral Academy and Postgraduate Teaching Consortium
As a Postgraduate Research programme, quality management and enhancement of the ClinPsyD is overseen by the University Doctoral Academy. We are also part of a Division-level Postgraduate Teaching (PGT) Consortium, which feeds into relevant School and Faculty committees and is attended by representatives from a number of cognate postgraduate teaching programmes. The Programme Director attends regular consortium meetings, where quality management issues are discussed. We are also subject to a system of peer review of teaching operated by the School of Health Sciences.
University Annual Review
The Programme conducts an annual review process every December, where we complete a self-evaluation procedure and consider our progress in relation to the previous year’s action plan. We also set a new action plan for the coming year. The self-evaluation document and action plan are scrutinised by the Doctoral Academy. The Programme is also subject to a major University review every 5 years (“Periodic Review”), which is timed to coincide with our BPS accreditation visit.
Student Feedback on Programme Quality
Students fill in web-based ratings for every teaching session. We take student feedback very seriously, and have made many changes to the Programme as a result of trainee views. Indeed, students have seen us completely re-structure the timetable in line with their comments. Our last BPS accreditation report commended the Programme on its feedback systems, noting that they “ensure that trainee concerns are given serious consideration”.
Trainees’ names are not attached to their feedback (so it is effectively anonymous) but, if offensive or otherwise unprofessional comments are made, our electronic system allows us to track the author and take appropriate action if necessary. Staff-Student Liaison Committee meetings, which take place at the end of every term and are attended by the Programme Director and Academic Director and trainees from each year group, also provide an opportunity for trainees to comment on teaching sessions and the Programme as a whole. Minutes of the meetings are made and circulated to programme staff, Module Organisers and students. The Module Organisers also receive a list of the ratings for lectures and student comments. Module organisers write individually to lecturers to pass on the feedback, and make modifications to the Programme as necessary. Where a particular lecturer has been the subject of poor feedback, the chair of the Curriculum Sub-committee will make personal contact with the Module Organiser and decide what action should be taken to help the lecturer improve the quality of the teaching.
Students fill in rating forms on all placements. If there is a difficulty with a specific placement, feedback will be given. If there is no improvement, the Programme will give further feedback and decide whether or not to continue to use that placement.
At the end of Year 3, there is a final review where trainees are asked to review the training experience as a whole. The overall experience of balancing teaching, exams, placement-based work and assessments and research is discussed. As a result, numerous changes have been made in recent years. For example, Reflective Practice Groups were introduced to the programme with the aim of providing more opportunity to explore and enhance reflective skills through a range of learning experiences. These include internally facilitated problem-focused discussion groups in the first and second year of training and peer-facilitated groups in years two and three.
Lecturer Feedback
Lecturers are provided with a feedback sheet to provide information on their experience of teaching the trainees. This information is fed back to the trainee group in reviews, and is useful if there is a difficulty over some aspect of teaching.
Graduate and Employer Feedback
The Programme undertakes yearly reviews of past graduates and their first post-qualification employers to ensure that the programme of study is sufficient to meet the needs of the workplace. This feedback is shared with stakeholders and informs the development of all aspects of the Programme.
External Quality Assurance Mechanisms
Professional regulation by the Health and Care Professions Council (HCPC)
It is a requirement that all Clinical Psychology Doctorate programmes meet the Standards for Education and Training laid out by the HCPC, who are our professional regulator, and that all our graduates meet their Standards of Proficiency for Practitioner Psychologists. HCPC approval is essential to ensure that our graduates are eligible for professional registration as Practitioner (Clinical) Psychologists on completion of the programme. We are subject to Annual Monitoring by the HCPC, and have to complete a detailed return every two years demonstrating how we continue to meet their training standards.
Professional accreditation by the British Psychological Society
The ClinPsyD is accredited by the British Psychological Society, who carry out an accreditation visit every five years to ensure that we continue to meet their rigorous accreditation standards, which set out the requirements for excellence within clinical psychology training.
Health Education England
We meet regularly with local representatives from Health Education England, who commission the training and conduct an Annual Review of quality, in order to ensure that our Programme continues to meet their quality assurance criteria.
External Examiners’ reports
External examiners’ reports are discussed at the Exec, the Examination Board and staff away days, as appropriate, in order that relevant action can be taken. They are also examined by the Doctoral Academy and Faculty PGT Committees and by the HCPC and BPS. External Examiners’ reports relating to this programme will be shared with student representatives at the Exec, where details of any actions carried out in response to the External Examiners’ comments will be discussed. Trainee should contact their committee representatives if they require any further information about External Examiners’ reports or the process for considering them.
Other Quality Assurance Mechanisms
The team discusses possible improvements at twice-yearly Programme Away Days. These events generate ideas for substantial improvements to the Programme. A newsletter, Programme News and Views, is sent regularly to NHS staff and trainees. Programme team members also attend School Away Days and University Academy for Education and Professional Development training events, including those pertaining to equal opportunities.
New members of academic staff attend the University’s New Academics Programme. They are also assigned a supervisor and a mentor, a colleague who provides guidance and support over the first three years in post. Administrative and teaching duties are phased in gradually and there is an emphasis on establishing research activities early on.
All staff members are appraised regularly by senior colleagues who have attended relevant training programmes.
Employment Information
Employer
Trainees are employed by Greater Manchester Mental Health NHS Foundation Trust. All administration is carried out by Human Resources (Tel: 0161 358 1156 or Email: resourcing@gmmh.nhs.uk). All employment with GMMH is conditional upon continuous registration on the ClinPsyD Programme at the University of Manchester. Loss of registration on this Programme will incur immediate termination of a student’s contract of employment.
Salary
Starting salary for trainees will be at the agreed level under the Agenda for Change banding.
Superannuation
Trainees have a choice as to whether or not to belong to the NHS pension scheme. A booklet describing this scheme is provided by the employer. Enquiries about Superannuation should be directed to the Payroll department at North Manchester General Hospital on 0161 720 2610.
Holiday Entitlement
- The basic entitlement is 27 working days, in addition to statutory holidays, per year. The ‘holiday year’ starts on 1st April, and trainees are entitled to 13½ days holiday in the first 6 months of the Programme (i.e. up to the end of March). All trainees should keep accurate records of annual leave taken.
- Current NHS Trust conditions of employment allow trainees to ‘carry forward’ up to 5 days unused holiday entitlement into the next financial year. Trainees are not allowed to carry over any more than this, so should plan their leave to make use of their holiday entitlement. Trainees are often surprised by how difficult it is to make use of the full holiday entitlement, and should ensure that they plan to use the time.
- Holiday dates must be agreed in advance with the placement supervisor. The earlier the trainee plans the holiday, the more helpful it is to the supervisor; in particular, it is helpful to warn the supervisor of a future placement of any holiday they wish to take at the beginning of the placement, as well as informing your employer via the procedure below.
- Trainees wishing to book holiday leave must complete an Application for Annual Leave form available from the intranet. This form must then be signed by the supervisor and returned to Indre Miskunaite before the start of the dates requested. The Programme will keep this information for its own records and will also pass the information to the employer’s Contracts Manager.
- If annual leave falls on a study day this must be included as part of the annual leave entitlement; if trainees are planning to do anything other than undertake legitimate work in pursuit of the ClinPsyD, they should submit an annual leave form for that study date. Study days are working days, but the place of work is not specified. As an example, if you are going on holiday Saturday to Saturday, an annual leave form must be submitted that includes the entire week as days cannot be taken as study leave time if you are not available to study.
When Can Trainees book Annual Leave?
Trainees are able to book annual leave within their NHS allowance, on study days and placement days. As part of our commitment to supporting well-being, trainees are also now entitled to take a maximum of four days of annual leave on teaching days per academic year (equating to two weeks off teaching); this is to enable people to maximise their self-care, attend special events and arrange holidays around childcare and other commitments. This is subject to the following rules:
-
- Any leave taken on teaching days has to be agreed in advance with your Academic Advisor so that there is some governance around what is missed
- Leave is not allowed to be taken during any of the induction blocks;
- Trainees must catch up on anything they miss by accessing lecture notes etc.
- Once approved, trainees must complete the usual Application for Annual Leave form and submit it to Indre Miskuniate, noting that it pertains to leave on a teaching day; trainees must also inform the lecturer(s) of their intended absence (there is no need to give a reason other than that you are taking leave);
- Trainees must anticipate any special occasions so that these are covered by their entitlement for leave during teaching time; we will not ordinarily allow people to take more than four days off teaching per year unless there are exceptional circumstances that could not have reasonably been predicted.
Teaching is otherwise compulsory.
The programme endeavours to ensure that trainees are able to book leave during protected weeks around Christmas, Easter and over the summer. Please be mindful of any case report or resubmission deadlines which are not highlighted on the year planner.
Sick Leave
- A trainee who is unable to attend placement through illness should inform their supervisor or his/her secretary at placement base and the University as soon as possible, on the first day of sick leave. Service users may travel long distances and departments will want to do everything they can to cancel appointments and avoid them having wasted journeys.
- All sick leave must also be registered with the Programme administrative staff on the first day of illness, regardless of whether the trainee is absent on a placement or a teaching or study day. Trainees should ring the department on 0161 306 0400 and leave details of their absence. Staff will complete a Sickness Absence Report Form; if staff are not available it is permissible to leave a voicemail message, but staff may telephone students later in the day if further information is required.
- Upon returning to work, students must telephone the department on 0161 306 0400 and notify staff that they have returned. Trainees’ Clinical Tutor or Academic Advisor will then complete a Return to Work Interview either in person or over the phone as soon as possible following the trainee’s return to work.
- Students should familiarise themselves with the GMMH Attendance Management Policy, which can be downloaded from the intranet or the GMMH website and which outlines procedures for monitoring absence due to illness.
- Requests for compassionate leave should be made to one of the Clinical Directors.
Study Leave
The Programme ordinarily allows a number of days’ study leave to help prepare for the examinations and progress the research project. These are:
- Four days before each set of exams, that is at the end of terms 2, 3 and 6. These dates are set by the Programme staff and placement supervisors will be notified of the need for time out of placement.
- Four days in Spring term of Year 1, which should be used to work on the Research Proposal prior to the submission date. These dates are set by the Programme staff and placement supervisors will be notified of the need for time out of placement.
- Four days in Spring term of Year 2, which should be dedicated to research activities at the trainee’s discretion. These dates are set by the Programme staff and placement supervisors will be notified of the need for time out of placement.
The Programme also allows a number of days’ research leave, which can be booked by the trainee subject to the approval of their placement supervisor. These are:
- Four research days can be taken outside teaching time, following research supervisor allocation (January) until the end of Year 1. These are to be taken in consultation with the clinical supervisor.
- Ten additional research days can be taken outside teaching time, from 1stOctober in Year 2 until submission of the thesis in the Year 3. These are to be taken in consultation with the clinical supervisor.
- Two further days in Year 3, following submission of the thesis, until the date of the viva voce examination, for finalising papers for publication and preparation for the viva.
Days not taken within the specified time period may not be carried over.
Research days should be booked with the agreement of a trainee’s placement supervisor and a ‘Research Day Request Form’ completed and submitted to the admin team prior to the leave. This form can be downloaded from the intranet / Canvas: Research Downloads; General.
Study days are working days, but place of work is not specified. Study leave is not taken at the expense of annual leave.
Please remember: Study days are not leave days, and cannot be added to your holiday entitlement!
Travel Expenses (Placement)
- Greater Manchester Mental Health NHS Foundation Trust will pay travel expenses at the Agenda for Change Public Transport rate. Travel expenses are administered at ELFS Payroll Shared Services, Tel: 01254 786007. You will need to quote your assignment number when making enquiries
- Expense claims are submitted via GMMH’s e-expenses system EASY
- In order to claim mileage you will need to show the programme administration team your certificate of motor insurance indicating that you are covered for business use at the start of the programme and subsequent year, and also a copy of your MOT certificate.
- The rate will apply to the “excess” mileage, i.e. the mileage after your normal home to base (Zochonis Building) mileage has been deducted from your daily journey. Full details of your journey should be inputted on the system. These payments are subject to the deduction of income tax as directed by the Inland Revenue
- No travel expenses are paid for attendance at academic occasions
- Travel expenses within placement (e.g., visiting Health Centres, or doing domiciliary visits) will be paid so long as the travel is above and beyond your ordinary commute (i.e Home- Zochonis)
- Trainees should ensure that personal motor insurance covers use of your car for work purposes; you will usually need business insurance
- Claims for travel expenses should be submitted via the e-expenses system monthly and before the first day of the month if you wish to receive reimbursement with the next salary payment. You need to submit your car details via the system before you can claim.
- Lease Cars can be obtained through North Manchester General Hospital providing the cost for this is not greater than the trainee’s actual or anticipated travel expenses. You should contact the Programme Administrator if you would like more information; however, it should be noted that cars are leased for three years in full, and the duration of trainees’ contracts of employment means that significant ‘early return’ fees will be applicable, payable by the trainee. Due to this, trainees interested in this scheme should enquire within the first three months of training. Requests made after this time are not likely to be granted except in exceptional circumstances. The employer will have the final decision as to whether or not a lease car can be made available
Research Expenses
Costs incurred as part of trainee large-scale research projects may be claimed back from the University up to a maximum of £400 (or more if additional funding has been approved – see research section).
It is not permissible to claim for binding or printing of the thesis. Mileage may be claimed back at a rate of 45 pence per mile for return journeys of 150 miles or less (25 pence per mile for each additional mile over 150 in a single journey).
Claims must be submitted on the University claim forms (NOT the NHS forms which claim placement mileage) by a set date in Year 3 following submission of the thesis, although trainees are encouraged to make claims throughout the research process. Queries regarding research expenses should be addressed to Tracey Hepburn.
General Information for Students
Programme Funding
The University has a Contract with Health Education England to provide Clinical Psychology training. Most of the Programme team and secretarial staff are employed through this contract. Trainee salaries are administered through Greater Manchester Mental Health NHS Foundation Trust.
In addition to being NHS employees, all trainees on the Programme are enrolled as students at The University of Manchester, and are governed by the University’s student policies and procedures.
University Registration
Every ClinPsyD student must register at the beginning of the programme, and again at the beginning of the second and third year. Students will register in September of each year following the Examination Board at which assessment results are ratified. The Programme Administrator will forward information regarding registration to all students.
Student Policies and Procedures
Policies relating to students can be found through the Student Portal at http://www.studentnet.manchester.ac.uk/policies. These include:
- Crucial Guide for Postgraduate Students
- Presentation of Dissertations Policy
- Policy on Submission of Work for Summative Assessment on Taught Programmes
- Policy on Mitigating Circumstances
- Academic Appeals (Regulation XIX)
- Guidance to Students on Plagiarism and Other Forms of Academic Malpractice
- Policy on Feedback to Undergraduate and Postgraduate Taught Students
- Conduct and Discipline of Students (Regulations XVII)
- Student Charter
The Code of Practice for Postgraduate Research Degrees can be found at; http://www.staffnet.manchester.ac.uk/services/rbess/graduate/code/
Please note: Due to the programme exit award being a professionally accredited degree, where passing a compulsory course unit is required, the programme will operate a necessary pass across all pathways – i.e. teaching, clinical and research units through to award of ClinPsyD. The programme will not apply compensation rules to any course units, and also will not allow referral of taught credits. In agreement with the NHS, students can only fail, and refer, 3 individual pieces of assessed work across the whole programme. If a 4th piece of work is failed, the student is deemed to have failed the programme. The professional based nature of the programme and accreditation agreements with the Health and Care Professions Council and British Psychological Society dictate these exclusions.
People
Who’s who
A large number of people, including both University staff members and practising clinical psychologists, are involved in formal teaching and clinical supervision. All programme staff have offices in the Zochonis Building, 2nd Floor, but are normally best contacted by email in the first instance given the prevalence of home working.
University staff
The staff members contributing to the management and delivery of the programme are as follows:
- Professor Gillian Haddock, Professor of Clinical Psychology and Head of Division of Psychology and Mental Health
- Professor Richard J. Brown, Professor of Clinical Psychology and Programme Director
- Dr Lara Bennett, Senior Clinical Tutor and Clinical Co-Director
- Dr Claire Fothergill, Clinical Tutor and Clinical Co-Director
- Dr Adam Danquah, Senior Clinical Lecturer and Academic Director
- Dr Daniel Pratt, Senior Clinical Lecturer and Research Director
- Dr James Lea, Clinical Tutor and Admissions Director
- Professor Adrian Wells, Professor of Clinical and Experimental Psychopathology
- Dr Sara Tai, Senior Lecturer in Clinical Psychology
- Professor Katherine Berry, Professor in Clinical Psychology
- Dr Anja Wittkowski, Senior Lecturer in Clinical Psychology
- Jude Moss, Senior Clinical Tutor
- Dr Peter Taylor, Senior Clinical Lecturer and Deputy Research Director
- Dr Katie Reid, Clinical Tutor
- Tobyn Bell, Lecturer in Clinical Psychology
- Dr Lizzie Tyler, Clinical Tutor
- Dr Lydia Morris, Lecturer in Clinical Psychology
A number of NHS Clinical Psychologists also hold honorary University contracts and they are involved with teaching and the supervision of research projects.
There are also Clinical Psychologists and Psychologists within the University who, while not on the Programme Team, provide teaching and research supervision. These include:
- Professor Tony Morrison, Professor of Clinical Psychology
- Dr Warren Mansell, Reader in Psychology
- Dr Fiona Ulph, Senior Lecturer in Qualitative Methods
- Dr Filippo Varese, Senior Lecturer in Clinical and Health Psycholog
Clinical tutor biographies
Dr Lara Bennett
I am one of the joint Clinical Directors (along with Dr Claire Fothergill) on the Doctorate in Clinical Psychology Programme. I completed my clinical training in Manchester in 1998 and worked clinically in a local CMHT until 2008. I am a Cognitive Analytic Therapy (CAT) practitioner. My clinical interests are in personality and relational difficulties and using CAT in a range of settings.
On the Doctorate programme I am clinical tutor for up to 16 trainees, completing placement visits to discuss competency and progress and offering support and guidance where needed. I am responsible for organising year 3 placements, maternity leave and flexible working. I regularly teach across several areas, including breaks and endings in therapy, reflective practice and placement related activity, as well as contributing to the supervisor training programme. I sit on the Faculty Fitness to Practise Committee and contribute to the School of Health Science practice placement forum regarding placement issues. I currently offer supervision for a placement in a local branch of the mental health charity, Mind and I am interested in public health and public mental health and how this can be incorporated into Clinical Psychology training. I am registered with the HCPC registration number PYL33025 and also a member of the Group of Trainers in Clinical Psychology.
Dr Claire Fothergill
Having completed my first degree at the University of York in 2000 I was keen to develop further my research skills and was appointed as a research assistant to Professor Willem Kuyken at the University of Exeter. I undertook a part-time two year Masters degree in Psychological Research Methods at Exeter (between 2000-2002) alongside my work and became interested in cognitive therapy and case formulation, and was keen to pursue training in Clinical Psychology.
In 2002 I started my Clinical Psychology Doctorate (ClinPsyD) training at Manchester and upon qualification in 2005 worked in NHS Primary Care with clients who presented with complex presentations. I offered trainee placements and supervised qualified Clinical Psychologists and CBT therapists, and led on the introduction and development of group therapy within my service. In 2010 I completed a post graduate diploma in Cognitive Therapy and was awarded a distinction.
In 2008 I joined the programme team as a Clinical Tutor and worked at the University part time, initially alongside my NHS role until 2014 when I decided to leave my NHS job. As a clinical tutor I assist the Clinical Directors and act as a training co-ordinator for a number of trainees across year groups and monitor and facilitate their clinical development and progress throughout training. I have lectured on the ClinPsyD on case formulation, interviewing skills, CBT for Depression, and a range of tutor related topics. I have been involved in delivering supervisor training and have taken a lead in assisting trainees who have disabilities or additional needs.
Ms Jude Moss
I am a Senior Clinical Tutor on the ClinPsyD programme and am module organiser for the Learning Disabilities module.
Administrative Staff
- Megan Brown, Professional Doctorates Officer, 0161 306 0404; megan.brown@manchester.ac.uk
- Tracey Hepburn, Programme Administrator; 0161 306 0400; tracey.hepburn@manchester.ac.uk
- Indre Miskunaite, Programme Administrator, 0161 306 0401; indre.miskunaite@manchester.ac.uk
NHS staff
Teaching on the academic programme
The majority of the teaching over the three years is provided by NHS staff with particular expertise in their given fields. Approximately 100 NHS staff provide teaching. The majority of these are Clinical Psychologists, many of whom also act as supervisors for clinical placements, and some also undertake research supervision. There are also contributions from other professions, for example, Psychiatry and Social Work. The Programme is therefore able to draw upon a considerable pool of expert knowledge in providing the teaching programme.
Clinical Placements
Half of the trainee’s time is spent on placement. Learning on placement is under the guidance of a clinical supervisor whose experience and skills meet the criteria set down by the BPS Committee on Training in Clinical Psychology (CTCP). At present we have a pool of approximately 150 supervisors across the region. Supervisors work in collaboration with the Programme to provide support for the development of clinical skills. The Programme liaises closely with them and provides training to ensure high quality and consistency. Students also provide detailed feedback both during and after the placements, an important source of information on quality.
Trainee Advocate
The trainees elect a Trainee Advocate who is a qualified Clinical Psychologist independent of the Programme management. He or she will act on behalf of trainees with respect to all aspects of the Programme, and attends the monthly Executive Training Committee meetings. The Advocate has access to reserve business at meetings that trainees are not allowed to attend.
The role of the trainee advocate is always occupied by people who are very familiar with the Manchester ClinPsyD programme and have some knowledge of the course, the staff and the processes in relation to the clinical, research and academic parts of the doctorate.
Advocates are there for confidential support, advice and advocacy. For example, if you wish the advocate can contact any of the course team on your behalf or if you need to raise an issue anonymously we can assist (although bear in mind that this may limit what the course can do about any concerns). The advocate has in the past been involved in issues relating to examinations, marking, leave, extra support where necessary, negotiation between the course and trainees, issues relating to research and clinical, placements, feedback, relationships between the course and trainees and many other situations too numerous to mention. The advocate also been involved in policy discussions regarding maternity and paternity arrangements and support following a serious incident. The advocate provides a confidential ear if you want to discuss concerns or worries you have and/or if you want advice. The advocate attends the Executive Committee meeting on the course and we have taken many issues to this forum. The advocate also has discussions with individual members of the course team and the course Director where appropriate and always with the explicit consent of the trainee. The advocate is there for both the large and small problems. The advocate has an annual slot in the teaching timetable for each year but are very pleased to hear from any trainee at any time.
The advocate has a good working relationships with the course team and Director and share a common goal of trying to give trainees an excellent experience over the 3 years of the course. The advocate is there to support you if there are any difficulties.
Community Liaison Group (CLG)
The Community Liaison Group brings together people who have used mental health services, carers and community members to contribute to all aspects of clinical psychology training. The Group’s key role is to ensure a better fit between the training provided by the University and the needs of clients Members meet monthly and the group feeds into all Programme committees. Trainees attend the monthly CLG meetings to develop relationships, communication and mutual involvement.
What we do
We aim to establish good relations between the community, professionals providing services to them, and staff within the University.
The Community Liaison Group is associated with the Faculty Centre for Engagement and Involvement.
Our Involvement
We aim to have involvement in a number of key areas of the ClinPsyD training programme:
- Selection of trainees.
- Co-production of teaching and providing teaching in the form of lectures and workshops.
- Ensuring that community and service-user perspectives are considered in research, e.g. LSRP research consultation.
- Ensuring that community and service-user perspectives are considered in placements, e.g. the creation of service user and carer feedback forms on placement.
- Ensuring that community and service-user perspectives are considered in assessment, e.g. providing feedback on video interviewing skills and the live clinical observation.
- Training the programme team, placement supervisors and lecturers to understand the needs of the local community.
- Involvement in Executive and Curriculum meetings.
- Participating in the programme away days and annual review days.
Over the years, the CLG has received a number of university social responsibility awards in recognition of CLG contributions. The group has presented at regional best practice conferences, developed an annual newsletter, shared practice with other University departments. The group has been commended during accreditation visits from them British Psychological Society (BPS) and Health and Care Professions Council (HCPC).
Contact us
The Community Liaison Group is based within the Clinical Psychology department of the School of Health Sciences. The main contact for the group is Dr James Lea, Clinical Tutor. Email: james.lea@manchester.ac.uk
Who Should I Ask?
Answers to most of the queries that people have can be found in the online handbook. We would therefore be grateful if you could check the handbook first, before you approach a member of staff for information. The handbook has a search function is you can’t find a relevant section heading.
If you can’t find the information you’re looking for in the handbook, the following people should be approached for information on particular subjects:
- Compassionate Leave – Lara Bennett or Claire Fothergill
- Holiday entitlement, Sick Leave – Indre Miskunaite
- NHS Expenses, Salaries – Megan Brown, Tracey Hepburn
- Research Expenses – Tracey Hepburn
- Curriculum – Indre Miskunaite/Adam Danquah
- Exams – Megan Brown/Adam Danquah
- Research –Megan Brown/Daniel Pratt
- Audits of Clinical Activity – Peter Taylor/Brendan Dunlop
- Service Related Projects – Katherine Berry & James Lea
- Placements, Supervision – Tracey Hepburn/Lara Bennett or Claire Fothergill
- Anything you are unsure about – Megan Brown/Tracey Hepburn
- Mitigating Circumstances – Megan Brown
- Complaints and Academic Appeals – Richard Brown
- Independent support/advocacy – Trainee Advocate
- Confidential Counselling http://www.staffnet.manchester.ac.uk/personalsupport/counselling/
- Flexible working and maternity leave – Lara Bennett/Tracey Hepburn
- Year 3 Placements – Lara Bennett
- Community Liaison Group – James Lea/Brendan Dunlop
Further information on trainee support systems is in the section below on Support and Guidance.
We all want to help trainees to get the most out of training, and try to help with any difficulties. Trainees’ Clinical Tutor and Academic Advisor will be able to help with a range of problems and are the first port of call in most instances.
Board of Examiners
All assessments on the Programme are ratified by the Board of Examiners, which is made up of clinical and academic members of the Programme team and the lead External Examiner. It is chaired by Prof Gill Haddock as Head of the Division of Psychology and Mental Health.
External Examiners
The Programme’s assessments are all undertaken with oversight and feedback from external examiners from other institutions. External Examiners are individuals from another institution or organisation who monitor the assessment processes of the University to ensure fairness and academic standards. They ensure that assessment and examination procedures have been fairly and properly implemented and that decisions have been made after appropriate deliberation. They also ensure that standards of awards and levels of student performance are at least comparable with those in equivalent higher education institutions. External examiners are selected to ensure that they are appropriately experienced and qualified. At least one, and usually most, examiners are Registered Clinical Psychologists.
The Programme has a lead External Examiner, who scrutinises the marking of all coursework and exams. They also examine theses and conduct individual oral examinations where necessary with students who have failed assessments during the programme. The lead External Examiner is currently Dr Georgina Rowse, who is Programme Director for the Clinical Psychology Doctorate at The University of Sheffield. In addition, further External Examiners are appointed to conduct viva examinations in Year 3 depending on their areas of expertise. All examiners meet at the Examination Board to moderate decisions following the vivas.
Please note that it is inappropriate for students to make direct contact with External Examiners under any circumstances, in particular with regards to a student’s individual performance in assessments. Other appropriate mechanisms are available for students, including the University’s appeals or complaints procedures and the UMSU Advice Centre. In cases where a student does contact an External Examiner directly, External Examiners have been requested not to respond to direct queries. Instead, External Examiners should report the matter to their Programme contact who will then contact the student to remind them of the other methods available for students. If students have any queries concerning this, they should contact the ClinPsyD admin team or the Graduate Office.
Teaching and Learning
Teaching, learning and assessment strategy
All students must learn academic, clinical and research skills. Our overall strategy for teaching is to use a range of approaches to address the different educational functions to be fulfilled by each. Academic and research teaching form part of the preparation for professional practice, and trainees should appreciate that the pursuit of academic excellence will enhance their effectiveness as practitioners, and the contribution that they will make to the NHS.
An important aspect of the Programme organisation is the design and administration of the teaching modules, which are organised by course staff or NHS psychologists with specialist interests and expertise. Representatives of community and service user groups are also formally involved in planning the Programme.
Academic Programme
The academic programme aims to give students comprehensive exposure to the wide range of areas of work of Clinical Psychologists, so that they are aware of, and prepared for, different routes post-qualification. On a broader level, the interactive teaching encourages self-directed, reflective learning.
The academic programme consists of lectures, workshops and problem-based learning. Through didactic teaching, small and large group discussion and feedback, students learn the theoretical and research basis for the approaches that they will use in clinical practice. Lecturers use case examples and/or small group teaching techniques to enable students to discuss links between theory and clinical practice. In this way, students develop and reflect on their ideas, and use their own experiences of clinical work in interpreting the literature. Trainees are encouraged to critically evaluate ideas, and to integrate their understanding of general psychological principles into the clinical context. There is an emphasis on learning based on real clinical problems.
Some teaching is clearly skills-based (e.g., interviewing and formulation), and students practise developing professional skills with feedback on performance by other trainees and lecturers. Role play is commonly used and all trainees are expected to participate fully in this aspect of training. As a condition of entry to the programme applicants are required to provide formal written consent to participate as service users in practical and clinical teaching. The consent protocol is designed and implemented by the Programme.
Participation in peer supervision and reflective practice groups gives trainees the opportunity to receive and provide further guidance and supervision on clinical work, and to hone their reflective skills.
Most lecturers make their slides available to trainees and identify key references so that trainees can undertake guided reading around the topic. Study time is provided each week. Wide reading and revision is encouraged throughout the course and in preparation for the examinations at the end of each block, for which study time is provided.
Placement experience
During the programme, trainees spend 50% of the time on clinical placements where they carry out supervised clinical practice. Each placement is approximately six months in duration. The Clinical Tutors inform trainees of the starting dates. Year 3 placements are of nine months duration between January and September. In normal circumstances the first two years consists of four six-month clinical placements in the core areas of Adult, Child, Older Adult and Learning Disability. A wide range of placements is available and trainees are able to exercise considerable choice in their Year 3 placements, as long as the placement is able to meet any outstanding training needs; a placement register is kept to help trainees choose.
Learning on placement is primarily through guided practice and reflection in the context of the supervisory relationship. Students are exposed to a wide range of cases, and are guided to read around clinical work to attain integration of theoretical knowledge and practical skill. In supervision, trainees are given detailed feedback on a range of aspects of their clinical skills, including interpersonal and professional performance. They are guided in report writing and communication with other professionals. Time is provided for supervisor-guided reading on placement.
Trainees observe their supervisors at work and undertake case work under supervision. Supervisors ensure trainees have exposure to more complex cases as training proceeds, through joint working where appropriate. There is a developmental progression, so that in the third year, more complex cases will be taken on by the trainee, again with supervision. It is also expected that third year trainees will take on a caseload that is more in keeping with that of a qualified Clinical Psychologist, to help manage the transition to post-qualification life. Year 3 trainees all complete a Service-based Research Project (SRP) on placement after submission of their thesis.
Research
Learning research skills is a major part of the Programme, and requires a number of different levels of learning.
- In lectures, students learn to design studies using a range of different approaches, and to critically evaluate these in group discussion.
- Within one of the first four placements, trainees must produce an Audit of Clinical Activity (ACA) based on work conducted within that placement. In conducting the ACA, students learn about the practicalities of NHS-based research applied to real problems.
- The Large Scale Research Project (LSRP) is a substantial piece of independent, doctoral-level research that involves all stages of the research process, from developing an original idea through to final submission of a typed and bound thesis that is presented for oral examination. Lecture/seminars are given in the first year to help with the choice of topics and research supervisors. The trainee is helped in planning research and, in due course, writing the thesis. Trainees learn to select feasible ideas to evaluate, and submit a formal proposal on their planned study. Through the Research Sub-Committee process, the student is able to further develop and refine their ideas. Submitting an Ethical Committee application provides further practical learning. Statistical and/or qualitative analysis consolidates the formal teaching, and students may learn new analytic approaches at this stage. Formal academic writing skills are developed through discussion of drafts of the work. Each Trainee has two academic and usually one field research supervisor for their project. Research will normally take place within the University or any NHS provider unit within the North West.
Detailed information about the ACA and LSRP can be found in the research section of the handbook.
Overview and Organisation of Teaching
The content of the taught component of training reflects both the HCPC Standards of Proficiency and the BPS Accreditation Criteria. The Programme capitalises on local skills in order to provide particular expertise in cognitive behavioural, psychodynamic interpersonal, clinical neuropsychology, and systemic approaches, which are recognised strengths of the University and local NHS departments. Detailed information about the academic knowledge that will be acquired is summarised in the Academic Curriculum, which is available on the programme intranet.
The Programme provides training on all stages of the life span; trainees spend their first 12 months studying clinical problems associated with adulthood and childhood. In Year 2 trainees learn about old age, learning disabilities and physical health. Each of these topics is taught with clinical and academic material integrated, so students immerse themselves in academic and practical aspects of the training simultaneously. Academic material is taught to the group as a whole by lecture, workshop, seminar and clinical problem-based tutorials. Experienced Clinical Psychologists teach clinical skills on placement through one-to-one supervision.
At the end of each block, students are assessed in order to ensure that they have met the desired learning outcomes for academic knowledge and clinical and professional skills. The final year of the programme is designed to cover more specialist, advanced areas of work and to re-visit core skills in greater depth. Students begin to plan their research in January of Year 1, and individual doctoral-level research experience is a focus of Years 2 and 3.
Organisation of the Curriculum
The curriculum teaches basic, generic skills in years 1 and 2, and places emphasis on the development of specialist and advanced skills, including doctoral-level research, in the third year. In Induction Blocks, students learn basic skills necessary to cope with starting clinical placement. An induction precedes each core block. Teaching on Personal and Professional Development spans all three years of training.
In Year 3, trainees have advanced workshops on a range of specialist areas. These include Personal and Professional Development (including Team Working and Leadership), working with complexity and sessions designed to prepare for the workplace.
Year 1 Induction Block
This is intended to provide new trainees with basic knowledge and skills to enable them to start the first placement with a reasonable degree of confidence. Elementary interviewing skills, assessment, formulation and treatment methods are covered, as are theoretical underpinning of cognitive behavioural therapy, using various formats including formal lectures, workshops and role-play.
Main Academic Programme
Fundamental clinical skills
The themes introduced in the Induction Block will continue throughout the first year. As well as skills training, the theoretical bases of treatment and assessment methods will be covered.
Core clinical experience – knowledge and skills
During Years 1 and 2 teaching corresponds to placement activity. Programmes of lectures and workshops focus on working with adults in terms 1 and 2, children and families in terms 2-3, and older adults, people with learning disabilities and health in terms 4, 5 and 6. Modules covering cognitive behaviour therapy, family therapy, substance misuse, psychosis, personality disorder and forensics take place across the three years of training. At present, students typically complete at least two problem-based tutorials per year.
Psychodynamic Interpersonal Therapy (PIT)
Students are introduced to PIT in term 1 of the first year. They are taught to formulate from a PIT perspective and acquire skills in using adjunctive PIT techniques that will enhance their ability to develop the therapeutic relationship and to work with emotional material whatever clinical approach they are using. They also learn about PIT as a standalone model of therapy.
Clinical neuropsychology
Teaching on clinical neuropsychology, which is one of the core clinical frameworks on the Manchester ClinPsyD, begins in term 1 of year 1 and spans all three years.
Research methodology
Commencing in Year 1 and continuing through Year 2, there are lectures on research methods, various designs and statistics, including practical computing sessions with statistical software packages. The research methods teaching is divided into process and content sessions.
Personal and Professional Development (including Team Working and Leadership)
Teaching extends across the 3 years, with Advanced Workshops in Year 3. There is a reflective practice curriculum which provides the opportunity to practice reflective skills through a range of learning experiences, including internally facilitated problem-focussed discussion groups in the first and second year of training and peer-facilitated groups in years two and three. Detailed introductory teaching relating to the reflective curriculum is delivered in advance of the sessions, which commence during term one of year one.
Power, Position, Privilege and Intersectionality (formerly Diversity and Engaging the Community)
Teaching for this Module extends across the 3 years.
Placements
PLEASE NOTE THAT THERE MAY BE TEMPORARY CHANGES TO PLACEMENT PROCESSES AND PROCEDURES ON THE CLINPSYD AS A RESULT OF THE CORONAVIRUS PANDEMIC. STUDENTS SHOULD THEREFORE REGARD THE INFORMATION IN THIS SECTION AS “NORMAL PRACTICE” ON THE PROGRAMME BUT CONSULT THE SECTION ON CORONAVIRUS FOR THE MOST UP TO DATE INFORMATION ABOUT ANY CHANGES TO PLACEMENTS.
Overview
Approximately 50% of the ClinPsyD programme consists of supervised clinical practice. This typically takes place within an NHS establishment that has been approved by the Programme organisers as a training placement and will involve the direct and indirect (i.e., working at a consultatory level through other staff) assessment and/or treatment of NHS patients. In a small number of cases, placements may be provided within Private Independent or Voluntary Orgnanisations (so-called PIVO placements), which are subjected to the same rigorous quality management processes as NHS placements.
Clinical training is supervised during clinical placements by experienced clinical psychologists who will have received induction in supervision. On all placements, the supervisor is clinically responsible for the trainee, so that it is essential that all work is carried out under close supervision and to the satisfaction of the supervisor. Learning on placement is primarily through guided practice and reflection in the context of the supervisory relationship. The job of the supervisor is to provide training and experience in particular methods and to ensure that the trainee sees as varied and comprehensive a range of cases as possible, with graded exposure to cases of differing levels of complexity over time. Through discussion at the start of placement, the supervisor will also help to select the most appropriate cases for the trainee’s needs and acquisition of competencies. In supervision, trainees are given detailed feedback on a range of aspects of their clinical skills, including interpersonal and professional performance. They are guided in report writing and communication with other professionals. Time is provided for supervisor-guided reading on placement in order to help them attain integration of theoretical knowledge and practical skill.
Supervision styles obviously vary between supervisors, but trainees should expect to have a formal session of up to one and a half hours with the supervisor once a week. Supervisors should also be available for advice/consultation at other times as well. Both supervisor and trainee should have the opportunity to observe each other working. Written work (clinical letters and reports) will be scrutinised by the supervisor before being sent out. At the start of each placement the trainee and supervisor will agree on a plan for the placement with specified learning outcomes.
In normal circumstances the first two years consists of four “core” six-month clinical placements in the core areas of Adult, Child, Older Adult and Learning Disability, each lasting approximately six months in duration. The Clinical Tutors inform trainees of the starting dates. Year 3 placements are 9 months in duration. For the 2016 intake onwards, the placement that a trainee undertakes in year 3 will be informed by the level of competence that has been gained during the first 2 years in CBT and a second intervention model (see Competence Frameworks section for further information). For example, if a trainee has successfully completed Level 2 competence in CBT plus one other model, then they will be able to have some degree of choice for their 3rd year placement experience, which might focus on Level 3 skills in one of the core models or gaining competencies in another models. If they have not been able to achieve Level 2 competence in two of the core models (including CBT) then some of the 3rd year placement will focus on the acquisition of the competencies necessary to practice at that level. A placement register is available on the intranet to help inform all placements.
The Clinical Tutors advise on the range of placements available.
Trainee are given access to an electronic Clinical Portfolio in which to record the experiences obtained (e.g., types of cases seen, tests used, treatment methods employed). Mid-way through each placement the trainee will be visited by their Clinical Tutor (a member of staff who will monitor all placements and act as an individual co-ordinator of training through the Programme) to review progress and discuss any problems that the trainee or supervisor may have encountered; the Clinical Tutor may make specific recommendations about further experience or supervision in certain areas.
At the end of the placement, the supervisor is asked to provide a report on the trainee’s performance; the trainee should see this report and have a chance to discuss it with the supervisor before he/she submits it. The trainee is also asked to provide a brief report on his or her experience of the placement. The trainee also meets the Clinical Tutor at the end of each placement to review progress in general.
It is important that trainees keep their Clinical Portfolio up to date and show it to their supervisor and to each new supervisor as they move to a new placement. In this way, any gaps in experience can be identified and remedied. Clinical tutors will also monitor the content of the Portfolio.
Placement Related Study
As part of your time on placement you are allowed to have ½ day placement related study. This is to read around the area that you are working in and have more directed reading about your individual client work, prepare for your sessions and complete any other placement related study, for example, on your Audit of Clinical Activity if you are completing it on that placement. When and where you take the study time must be discussed with your supervisor. Sometimes trainees combine the half day per week into one day per fortnight and have the option of taking this at home, but again this needs to be discussed with your supervisor and permission obtained.
What Experiences Should be Gained on Placement?
The HCPC’s Standards of Proficiency are the threshold standards for safe and effective practice. They are the minimum standards the HCPC consider necessary to protect members of the public. These standards play a key role in ensuring that registrants practise safely and effectively and inform the kinds of experiences that trainees should have on placement. The HCPC’s Standards of Proficiency describes the standards expected of Clinical Psychologists; full versions are given to all trainees at the commencement of training and can be downloaded by clicking on the link above.
In addition to the HCPC’s Standards of Proficiency, the BPS’s accreditation standards gives details of the minimum standard that Programmes must achieve in all areas of training. There are specific requirements for supervised practice and clinical experience. The need for an overall plan of placements and development of experience is stressed. Both depth and breadth of experience should be achieved. A key part of these standards is that graduates must have demonstrated their ability to implement at least two evidence-based forms of psychological intervention, of which one must be cognitive-behaviour therapy (CBT).
Competence in the implementation of psychological interventions has to be benchmarked against agreed competence frameworks. On the Manchester ClinPsyD, we have adopted four main evidence-based models of psychological intervention (CBT, Psychodynamic Interpersonal Therapy/CAT/Brief Psychodynamic Therapy, Systemic Therapy, Clinical Neuropsychology), each of which has been benchmarked against a different external competence framework. Every trainee will acquire basic knowledge in all four of these approaches and be taught to formulate using the associated conceptual model. We call this Level 1 competence. All trainees also have to demonstrate a set of generic clinical competencies that apply regardless of the model being used. Details of the various competence frameworks are provided below.
In addition, all trainees will have to be competent intervening (at either Level 2 or 3) using at least two of these models, of which one must be CBT. The basic standards for intervention are the same for both Level 2 and Level 3 competence; however, we distinguish between these levels to recognise variations in the extent or level of experience gained in each therapeutic modality. Thus, someone who has achieved Level 2 competence in a particular model will have shown that they are able to intervene competently using that approach, but to a lesser extent or level than someone who has achieved Level 3 competence.
The taught programme is designed to provide Level 1 competence in each of the four models, which will be evaluated in the corresponding written examinations. The generic competencies are evaluated via written examinations and in general clinical practice whilst on placement, via the Supervisor Assessment of Trainee form.
At Level 2, competence is demonstrated through the delivery of interventions with a minimum number of cases on placement. Level 2 competence can be demonstrated during any of the clinical placements, as long as the supervisor declares themselves competent to provide supervision and evaluation in that approach for the cases in question; this should be discussed when the placement contract is agreed. In order to achieve Level 3 competence, the trainee must undertake a specialist placement in the relevant modality and demonstrate competence in a larger number of cases.
Trainees are also likely to acquire knowledge of, and experience using, other clinical approaches whilst studying for the ClinPsyD. However, all trainees will still need to demonstrate at least Level 2 competence in CBT plus one of the other main therapeutic models taught on the Programme. Where possible, trainees should aim to have achieved this by the end of Year 2. If a trainee has not demonstrated this competence by the end of Year 2 it must be achieved within Year 3, which may have implications for the choice of third year placement. For example, a trainee may not be allowed to undertake a third year placement using an approach that is not one of the four “core” intervention models, unless they have the opportunity to demonstrate the missing core competences on that placement as well.
Service User and Carer Feedback on Clinical Placements
End of Clinical Involvement Feedback Form (ECIFF)
Since October 2019, trainee Clinical Psychologists on the Manchester programme have been required to seek direct feedback on their clinical involvement with people* in the NHS services they undertake their placements in.
It is recognised that gaining feedback is important and valuable for trainees’ clinical placements. The end of involvement feedback form will be used primarily for the direct learning of the trainee to reflect on and develop their clinical practice. It is hoped that this will provide trainees with an invaluable learning opportunity to develop their clinical and professional competencies, directly from those they have had some form of clinical involvement with.
This feedback also provides another valuable dimension to supervisor evaluation of clinical competencies on placement and is welcomed by trainees.
The form is referred to as an End of Clinical Involvement Feedback Form (ECIFF) as it is intended to be used across the various clinical activities a trainee will undertake. For example: single screening sessions, single consultation sessions, psychological assessments, neuropsychological assessment, brief intervention, longer term intervention, therapy, psychotherapy, family work and group work.
Two versions of the end of clinical involvement feedback form have been developed. One is an accessible version for use with people who may have cognitive, language and/or developmental needs to aid understanding and ease of completion.
The clinical involvement feedback form is to be used in conjunction with the relevant session rating scales and/or outcome rating scales used in their relevant service contexts.
Trainee: How to use ECIFF on placement
The aim is for the trainee to seek feedback from the people they have worked with clinically. People are able to agree to or decline providing feedback.
- The trainee explains that they would be grateful if the person could give them some feedback about how they have found the clinical work completed together. The trainee explains that feedback can help them to develop their skills and provide them with the opportunity to become a better psychologist.
- The trainee explains that any feedback provided will be stored securely and will not change the care that person receives.
- Feedback will go directly to the trainee’s supervisor.
- The trainee explains that feedback can:
- Be shared directly with the trainee if the person is happy for their feedback to be shared (person indicates this on the form).
- Be shared indirectly with the trainee if the person is not happy for their feedback to be shared (person indicates this on the form). A general summary that does not identify the person giving feedback will be shared with the trainee by their supervisor.
- If the person agrees to provide feedback, they are asked to complete the relevant form (ECIFF 1 or ECIFF 2). Once completed they are asked to place it in an envelope provided, seal the envelope and give it back to the trainee.
- The trainee explains that they will pass the sealed envelope onto their supervisor, who will read the feedback. The feedback will be shared directly or indirectly with the trainee, depending on what the person providing feedback has indicated.
Supervisors: How to use ECIFF on placement
The aim is for supervisors to have meaningful conversations with trainees in supervision regarding the feedback they receive and to develop a trainee’s clinical and professional competencies.
Supervisors will be asked to include an anonymised general summary of the feedback on the SAT form (please discuss the relevant section with your clinical tutor).
If supervisors are significantly concerned by any feedback provided to the trainee, they should discuss this with their clinical line manager and inform the relevant clinical tutor on the programme.
*Term people will be used to refer to those who identify as patients, clients, service users or carers.
How are placements organised?
The HCPC and BPS no longer require trainees to go through core placements in particular areas: instead, the emphasis is on gaining core experiences and competences, whatever the setting. In common with the majority of training programmes, however, we tend to operationalise those experience within core placement types, which allows us to use supervisor resources in the most efficient and effective way. As such, the Manchester ClinPsyD continues to retain some organisation of experience based on discrete client groups (adults; children and adolescents; older adults; people with learning disabilities) and trainees on the Programme are required to complete placements in each of these four core areas. The timing of these placements is illustrated in the table below.
| October – March | April – September | |
|---|---|---|
| Year 1 (Mon, Tues, Thurs) | Adult | Child |
| Year 2 (Mon, Tues, Thurs) | Older Adult / Learning Disability | Learning Disability / Older Adult |
| October – December | January – September | |
|---|---|---|
| Year 3 Only | Teaching Block | Clinical Placement (Four days per week) |
It is recognised that experience in some placements will overlap with the experience that is normally associated with other placements (e.g. work in learning disabilities that involves experience with children).
Requirements for Year 3 clinical experience are less definite, enabling the trainee to consider placements reflecting individual needs and interests, depending on their acquisition of core clinical competencies in Years 1 and 2. Given the range of different experiences, no specific guidelines for Year 3 placements are given beyond the experiences required for a trainee to reach Level 3 competence in one of the core models (should they wish to pursue training at that level); however, it is highly likely that Year 3 placements will need to be used to ensure a trainee has achieved all the required learning outcomes and demonstrated competence in all areas prior to the completion of training (including reaching Level 2 competence in CBT and at least one other core model). This will be discussed in conjunction with the trainee’s clinical tutor.
Placement Arrangement Procedures
The Guidelines on Clinical Supervision produced by the British Psychological Society (2010) state the following with regard to allocation to clinical placements:
There should be an explicit procedure for allocating trainees to clinical placements. All trainees and supervisors involved should understand the procedures and know how to influence decisions about clinical placements. The person responsible for arranging placements should give primacy to general training requirements and competency development needs but should also take account of the needs of individual trainees. Information should be provided about the experience obtainable in the various placements to help trainees and programme staff to make placement decisions
The following guidelines have been produced in order to operationalise these recommendations for the Manchester ClinPsyD:
Core Placement Arrangement Procedures
The arrangement of all placements involves three processes:
- Establishing the pool of potential supervisors (this process is linked both with HCPC requirements and the Supervisor Training Programme and is carried out in conjunction with the other North West Clinical Psychology Training Programmes at Lancaster University and The University of Liverpool)
- Determining trainee needs
- Ascertaining trainee preferences (although please note that learning needs take priority over trainee preferences)
Determining the Needs of Trainees
This is an ongoing process that involves the following factors:
- HCPC Standards of Proficiency
- BPS Guidance for Clinical Psychology Programmes
- Needs from previous placements
- Stage of training and trainee prior experience
- Trainee prior knowledge and the clinical competence of the trainee
- Trainee confidence
- Health needs
- Personal factors (e.g. due to disability or needs of dependent relatives; geographical factors are also considered)
Assessment and monitoring of the training needs of trainees is an ongoing process across the three years of the programme. Responsibility for monitoring is undertaken by the clinical tutors in conjunction with trainees and supervisors.
Ascertaining Trainee Needs and Preferences
Trainee needs and preferences are ascertained via the placement visits for the preceding placement and the completion of the Clinical Developmental Needs Form (in ‘Download’ section of the intranet) by trainees, together with further meetings between trainees and clinical tutors as appropriate. Trainees are encouraged to gain information about placements through talking with Clinical Tutors and consulting the Placement Register, which is available on the intranet. In the case of the first placement (adult) the allocation of placements to trainees is based in part on information from their clinical application forms and also on information gleaned from a pre-placement needs form which is sent out prior to the commencement of training.
Core Placement Allocation
This process is:
- Needs-led
- Individual
- Flexible
It is envisaged that this will be a transparent process, subject to the need to maintain the confidentiality of information regarding trainees’ circumstances and needs as appropriate.
It is integrated with:
- Teaching
- Placement visiting
- Placement assessment
- Self-appraisal by trainees
- Research (small and large scale)
Other factors that are involved in this process include regional factors and co-operative planning with other Clinical Psychology Training Courses in the North West. The process also involves assessment of the quality of placements used:
- HCPC requirements for placement quality
- BPS minimum guidelines on placement quality (supervision, accommodation, etc.)
- Trainee feedback on placement quality
- Available resources in departments offering placements
Placements are allocated in the month preceding the start of the placement by the clinical tutors. Following allocation, trainees are expected to contact their new supervisor(s) to arrange a pre-placement visit.
Ultimately, the decision of placement allocation is made by the Clinical Tutors on the basis of a comprehensive assessment of each individual’s training needs. Not having a driving license or access to a car (unless there are disability issues) will not be reason enough to have a placement that is close to the trainee’s home. The programme uses two questionnaires to approve and monitor placement quality, one prospective and one retrospective. Both questionnaires are completed by the Clinical Director(s), the prospective every six months in advance of allocating students to placements and the retrospective annually at the end of each academic year. Only placements that conform to all of the criteria are used.
Year 3 Placement Arrangement Procedures
Year 3 starts with a research and teaching block between October and December. Trainees then start their final placement for four days each week for the remaining nine months of the training programme (January – September).
The Manchester ClinPsyD Programme is fortunate in having a wide range of high quality placements available, many of which are described in the Programme’s Placement Register available via the trainee intranet. Trainees are advised both to consult the Placement Register and to discuss possible placements with their Clinical Tutor or Academic Advisor. A ‘Placement Fair’ is organised in October of the second year so that trainees can meet a sample of supervisors who offer Year 3 placements, and start to think about areas that would be able to meet gaps in their learning. Details of the fair will be emailed to trainees in advance.
The three North West Clinical Psychology Programmes (Manchester, Lancaster and Liverpool) organise Year 3 placements together, adhering to the same procedures and deadlines. The procedure for choosing Year 3 placements is outlined by the Clinical Tutors in a teaching slot in the autumn term of Year 2. Briefly, trainees are advised to begin thinking about possible placements early in Year 2. During this time, trainees may contact potential supervisors to discuss or arrange a visit to the placement, having first discussed this with the Clinical Tutor responsible for organising Year 3 placements. At this stage, however, neither the supervisor nor the trainee should make a definite commitment to the placement.
Trainees are required to submit a ‘Year 3 Placement Request Form’ (from the intranet) by the beginning of February (see Programme Calendar for exact date). The tutors responsible for organising Year 3 placements will liaise with trainees’ individual Tutors regarding the level of competence they have obtained to date, and whether their placement preference for Year 3 will enable them to acquire all of the relevant competencies (including at least Level 2 competence in CBT plus one other model) before the end of training. At this stage, the Clinical Tutors review the requests together with those of trainees from Lancaster and Liverpool and write to the potential supervisors asking them to officially confirm their availability. The deadline for receiving this confirmation is in May (see Programme Calendar for exact date) and trainees are told of the outcome after this.
The reason for setting strict deadlines for the submission of choices is to enable these placement arrangements to be made in conjunction with the planning of placements for Year 1 and Year 2 trainees and with those of the neighbouring Clinical Psychology Programmes.
It should be noted that, in general, core placements take priority over Year 3 placements. Whilst supervisors are often willing to provide both a core and a Year 3 placement concurrently, if trainees are considering choosing a placement in a traditionally core clinical area they should discuss this with the Clinical Tutors, and may need to be prepared to reconsider either the choice or timing of the placement.
In exceptional circumstances, for example if there are no opportunities for a particular type of placement within the North West, trainees may wish to have a Year 3 placement outside the North West. If this is the case, there is a procedure for applying for such a placement and a formal application must be submitted to the Executive Training Programme Committee.
Procedures for Rearranging Placements
Although a very rare occurrence, it is recognised that a placement may need to be re-arranged (either before or after the start date of the placement) due to the following reasons:
- Unavailability of main supervisor due to:
- long-term illness (over one month)
- leaving current position
- internal re-organisation
- Irreconcilable differences between supervisor and trainee when the placement has started, leading to the cessation of training.
- Unprofessional conduct by the supervisor
- Other major factors that may affect the continuance of the placement, such as significant changes in a trainee’s circumstances.
In the case of 2 and 3, all efforts are made by the Programme Team to avoid such circumstances from occurring. In all circumstances, the Programme Team would carry out an assessment of the situation which would consider:
- The minimisation of disruption to both the training process and to the delivery of clinical services
- The stage of training of the trainee concerned (e.g. the needs of a trainee on their first placement would be considered different compared to their fourth placement)
- The type of placement involved (i.e. core or Year 3)
If it proves necessary to re-arrange an on-going placement, the following steps would be taken in conjunction with the assessment by the Programme Team:
- Where possible, an internal re-arrangement of supervision within the same service would be the preferred option
- Allocating trainee to a ‘spare’ placement if available and if feasible within remaining time on placement
- Allocating trainee to a supervisor on another ongoing placement
It should be recognised that ‘spare’ placements may not always be available in a given specialism.
How the North West Doctorate Programmes Manage Serious Concerns with Supervision on Placement
A document has been developed by the three North West Doctorate in Clinical Psychology programmes to deal with serious concerns about the clinical supervision of trainees on placement. The majority of placements offered are of extremely high quality and the three programmes are enormously grateful for the input to training provided by supervisors and for the high quality of their work. However, on rare occasions, concerns about supervision and the competence of supervisors are raised. The policy aims to deal with such situations in a way that is transparent to, and supportive of, supervisors as well as those raising the concerns. This should mean that where real difficulties do exist these can be identified, and appropriate action taken in order to remedy the situation. Please refer to the policy on the intranet for full details.
Trainees are encouraged to contact their Clinical Tutor as soon as possible if they have any concerns about their placement or the supervision they are receiving.
Where are the Placements?
Most clinical placements are in public service settings: NHS, Social Services or Education. Placements are in the North West of England and predominantly within the Greater Manchester area. We do have placement opportunities in other settings, for example, the voluntary sector and a school. These placement experiences would normally form part of a year 3 placement and further information will be given in the teaching about year 3 placements.
Ultimately, the decision of placement allocation is made by the clinical tutors on the basis of a comprehensive assessment of each individual’s training needs. Trainees need to be aware that in applying for the programme they have accepted that they will have to travel required distances from their homes to the locations specified above. Travel within placements will also be expected. It is necessary that all applicants must possess a valid driving licence and have regular access to their own transport to enable them to fulfil the requirements of placements (subject to reasonable adjustments for disability). If offered an interview, they will be required to bring their photocard licence on the day, which will also be used as documented photographic proof of identity. Candidates without a photocard licence must bring their paper driving licence (issued before 1998) and current passport.
The programme uses two questionnaires to approve and monitor placement quality, one prospective and one retrospective. Both questionnaires are completed by the clinical directors, the prospective every six months in advance of allocating students to placements and the retrospective annually at the end of each academic year. Only placements that conform to all of the criteria are used.
Clinical Supervision
What is Supervision?
Supervision is the process by which a trained senior professional helps another person to learn and develop professionally through engaging in a process of review of and reflection on their work. A useful definition is as follows: ‘The formal supervision, by approved supervisors of a relationship-based education and training that is work-focused and which manages, supports and evaluates the work of colleagues’ (Milne, 2007).
Who Can Be a Supervisor?
The BPS Standards for the Accreditation of Doctoral Programmes in clinical psychology (2017) state who can supervise clinical psychology trainees:
Trainees will have clinical or practice supervisors. These supervisors must be appropriately qualified, but may be registered in a different domain of psychology, or be a member of another profession:
• Psychologists providing supervision to trainees on accredited programmes must be registered with the Health and Care Professions Council.
• Members of other professions who are providing supervision to trainees on accredited programmes should normally be registered with an appropriate professional or statutory body.
The nature of supervision provided will depend on the organisational context in which the placement takes place and may range from supervision of specific case work to supervision of the whole placement experience. It is for programmes to ensure that all supervisors, based on their training, experience and CPD, have the appropriate competencies to be offering the particular services in which they are supervising the trainee.
All supervisors are expected to have completed training in supervision as recognised by the Society or provided by the education provider.
For full guidelines, please see BPS Standards for the Accreditation of Doctoral Programmes in clinical psychology (2017), page 29 onwards:
What Can be Expected from Supervision?
Placement information pack
Supervisors should provide trainees with a placement information pack at the start of placement. This may contain the following types of information, which can often be helpful when starting placement:
- Who’s who within the department – names and service structure
- Who are the client group and how do they access a service?
- Map of the locality and any useful information about demographics/social context
- Suggestions for professionals/organisations to speak with/visit/shadow (and/or a timetable for doing so)
- Administrative procedures – note keeping, letters, secretarial support etc.
- Coffee arrangements, library use, departmental ‘traditions’
- Professional issues – departmental protocols, dress, time-keeping etc.
- Health and safety arrangements
Structure in supervision
Supervisors should follow the BPS guidelines https://www.bps.org.uk/sites/beta.bps.org.uk/files/Accreditation/Guidelines%20on%20clinical%20supervision.pdf on amount of time allocated to supervision, i.e. at least one hour of formal supervision, and up to three hours of informal and formal supervision per week. The Manchester programme recommends 1.5 hours of formal supervision per week. Supervision should be booked in advance, be within working hours, and is the responsibility of the supervisor. Ideally, trainees will have their supervisor’s undivided attention during their supervision session. Many trainees mention that they find it disruptive if their supervisor takes phone calls during supervision time.
Cover when the supervisor is not around is important. If the supervisor knows that they will not be available at certain times when their trainee is on placement, it is appropriate for them to arrange for someone else to be available for the trainee to consult in case they have any unexpected difficulties with their work.
Keeping a record of supervision
Trainees are encouraged to gain the most from supervision by preparing effectively and reflecting on their own learning between sessions. Many services have their own guidelines for how supervision should be recorded and it is important that trainees and supervisors adhere to these guidelines in the first instance. Trainees may also wish to keep their own record of the learning arising from supervision sessions (see intranet for an example of a Supervision Log that may help to structure this process).
Reflecting on the experience of supervision
The Supervisory Relationship Measures (see intranet) were developed and published by trainees on the Oxford Clinical Psychology programme under the supervision of Dr Helen Beinart. One measure is the trainee’s view of the supervisory relationship, giving ratings for different subscales, and the other measure is from the supervisor’s perspective.
These measures can provide a useful tool for reflecting on supervision and enhancing the supervisory relationship. Trainees and supervisors may find it helpful to consider these measures when drawing up the psychological contract and to complete these at one or more points during placement in order to support further discussion, although this is not a programme requirement.
Choosing cases and deciding on caseload
The size of the caseload should be decided through a process of negotiation, bearing in mind the formal guidelines. It is clearly difficult to prescribe an ideal caseload, or mixture of cases, which will vary according to abilities, interests and referrals. The Programme has introduced guidelines for the types of experience that trainees should expect to gain on each of their core placements (see intranet), based on the placement guidelines issued by the associated Division of Clinical Psychology Faculties and Special Interest Groups (SIGs). Caseloads and contracts should, however, be carefully tailored to the trainee’s current level of training, and individual training needs (including the attainment of competencies described in the Clinical Portfolio). Trainees need both relatively straightforward cases, to build up confidence, and less easy ones, so that they are prepared for work post-qualification. Trainees are able to take on more difficult cases when they are very closely supervised, and this can be a valuable learning experience. Overall, the quality of clinical work should take priority over quantity, and the standards of a single case study, with careful assessment, formulation and planning of intervention and evaluation of change should be followed.
Observation of Clinical Work
Trainees should have the opportunity to watch their supervisor working, and the chance to discuss this. Similarly, trainees should be seen at work, so that the supervisor can help the trainee to develop appropriate skills. Video and audiotaping can be helpful in this process, with a focus on the trainee’s strengths and positively framed feedback on areas for improvement. Trainees are encouraged to video record clinical sessions as often as possible and watch these back independently or with their supervisor(s) for feedback (see below). The temptation to collude in avoiding this aspect of supervision should be acknowledged.
Observation of the trainee
It is a requirement that trainees’ clinical work is observed by the supervisor on AT LEAST SIX different occasions for each placement. This can be direct observation or using audio/video recordings. Ideally, this should include:
– 2 x Assessment Sessions
– 2 x Intervention Sessions
– 2 x Other forms of work (e.g. teaching, staff meetings, consultation)
Observation of the supervisor
It is a programme expectation that trainees observe supervisors early on in the placement on AT LEAST TWO occasions.
Talking about clients
Trainees have said that they also like it when their supervisors discuss their own clients with them, and this may again help to introduce trainees to cases that are beyond the current level of difficulty that they feel able to deal with. Sharing cases which have not worked out so well can also be helpful, and can help trainees to feel safe about talking about their own problems in clinical work. Trainees have also said that it is helpful if supervisors are able to recognise when clinical material is causing difficulties because of the trainee’s own personal issues and help the trainee to find ways of dealing with this. This is, of course, a shared responsibility and relies on trainees being responsive to supervisors’ efforts to reflect on these issues as they arise.
Feedback
Trainees should be given positive feedback on those areas of their work which are good or developing well, and should also be given clear feedback on those areas which require further improvement. Supervisors should also be prepared to address problematic aspects of the trainee’s style as sensitively as possible, and in a way that does not damage the trainee’s self-esteem.
Advice and Guidance on Formulation and Intervention
Trainees should be guided towards a clear formulation of a clinical problem, with clear advice on the direction which should be taken in clinical work. Trainees may find it helpful to refer to the DCP Good Practice Guidelines on the use of Psychological Formulation (BPS 2011).
Study and Reflection
Placements should incorporate time for study and reflection of clinical matters. It is helpful if trainees can be directed to up-to-date written or taped material which is relevant to their current clinical work and training; time should be allowed for trainees to process this information. Half a day study time is allocated for this purpose and should be discussed with the supervisor.
Video and Audio Recording on Placement
Trainees in year 1 will be provided with a video camera for use throughout that academic year. This is to be used for recording clinical work on placements and trainees are encouraged to record and watch as much of their own work as possible, as a means of reflecting on and learning from their work. Trainees are strongly encouraged to use some time in supervision to look at this video material with their supervisor, for their comments and guidance. Trainees in year 2 will be given an audio recorder and encrypted memory stick for the same purpose.
It is essential that informed consent is gained before recording any clinical work on placement. A consent form for this is available on the intranet and must be used. Trainees must also discuss local policies and procedures around video recording with their supervisor(s) at the start of the placement. Trainees must find out if the placement provider (e.g. NHS Trust) has a consent form for video recording clinical sessions. If so, this may also need to be completed in addition to the university form.
Any video recording of clinical work must be treated as sensitive personal data. Under the Data Protection Act (2018), personal data (i.e. data relating to a living individual that enables him/her to be identified) must be processed lawfully and for a specific purpose, should not be kept for longer than necessary and should be protected against unauthorised or unlawful processing and accidental loss, destruction or damage. The video recordings should only be made using the equipment provided by the university for this purpose. Once the camera/ memory stick contains any recording of clients, it should be kept under lock and key at the placement premises. It should not be left in unattended cars or easily accessible areas and must not be taken home. The video files must not be transferred to personal computers or laptops, sent by email or placed on the internet. Any recording that is made away from the placement base (e.g. during a home visit) must be transferred to the encrypted memory stick as soon as is reasonably possible. The SD card in the video camera will store approximately three hours of recordings. In addition, a further three hours can be transferred to the encrypted memory stick, using the procedure outlined in the document “video recording equipment information” which is available on the intranet. At the end of the first year, all video recordings must be removed before the camera is returned to the university.
The Supervisee’s Role
Although the onus rests with the supervisor to develop and maintain effective supervision we expect the trainee (as supervisee) to also contribute to this through active preparation for and participation in supervision. Teaching will be provided on this role and trainees will be encouraged to reflect on their contribution to the supervisory process – both as part of their own professional development and in preparation for their own supervisory practice in future.
Supervisors and trainees work to develop a relationship where feedback on both sides is an on-going process. The use of placement contracts, psychological contracts, learning objectives and the two evaluation forms ([i] Supervisor of trainee and [ii] Trainee of placement) should be seen as assisting, not replacing this. Explicit reference to the forms and contracts at the beginning, middle and end of placement will help with overall reviewing of the work. Supervisors are encouraged to help trainees identify and work on areas which need development, as well as giving positive feedback on strengths; equally, they need to be open to the trainees’ views on the helpfulness of supervision and placement experience.
From placement two onwards trainees are required to share the ‘Supervisor’s Assessment of Trainee Form’ (or ‘SAT’ form) from the previous placement with their new supervisor to help build and refine skills, and prioritise any areas that may need attention.
Trainees should be mindful of all of the professional guidance published by the HCPC and The British Psychological Society. Amongst others, the following is a list of key relevant documents that are all available for free download from the HCPC and BPS websites (www.hcpc-uk.org & www.bps.org.uk).
HCPC
- Guidance on Conduct and Ethics for Students (2016)
- Continuing professional development and your registration (2017)
BPS
- Code of Ethics and Conduct (2018)
- Division of Clinical Psychology – Guidelines for Clinical Psychology Services (2011)
- Electronic Records Guidance (2019)
- Division of Clinical Psychology – Guidelines for CPD (2010)
- Practice Guidelines (2017)
- Sexual Harassment at Work and the Ethics of Dual Relationships (1993)
- Prevention and Management of Violence at Work (1992)
- Working in Teams (2001)
- In addition, there are a number of information leaflets available for free download.
- Clinical Governance in the NHS: A briefing
- Defining Quality
- Branches and subsystems have many downloadable documents relating to specific client groups and areas of clinical practice.
Ensuring High Quality Supervision
The Programme follows the BPS Guidelines on Clinical Supervision (2010), which set out the following procedures for ensuring high quality supervision:
1. Qualifications of supervisors
1.1 Trainees must be supervised either by:
- A clinical psychologist who is registered with the Health and Care Professions Council, and/or who holds Chartered Membership of the Society and full membership of the Division of Clinical Psychology, who has at least two years’ post-qualification experience, and who has clinical responsibilities in the unit in which the work is carried out; or
- Any other appropriately qualified and experienced psychologist who is registered with the Health Professions Council, and/or who holds Chartered Membership of the Society; or
- An appropriately qualified and experienced member of another profession who is registered with a professional or statutory body which has a code of ethics, and accreditation and disciplinary/complaints procedures.
In case of (ii) or (iii) above, the quality and quantity of supervision that is received by the trainee must be monitored carefully by the Programme Director or Clinical Tutor.
1.2 Supervision should normally be provided by a supervisor who has clinical responsibilities in the unit or service in which the work is carried out.
2. Supervisors Workshops and Meetings
2.1 Programmes must organise regular supervision workshops to train supervisors in methods of supervision; these should be designed with the needs of new as well as experienced supervisors in mind. Supervisors are expected to attend workshops on supervision. There should also be regular meetings at which supervisors have an opportunity to share information and discuss problems. Where programmes make use of team supervision, viz. where the ratio of trainee to supervisor is other than 1:1, the programme must ensure that appropriate guidance is given to supervisors and trainees on the procedures that are necessary for good team supervision. It will probably be necessary to establish supervisor workshops related specifically to team supervision.
2.2 Suggested learning objectives for introductory supervisor training are provided at www.bps.org.uk/accreditation/downloads. Programmes that have developed supervisor training that reflects these objectives are able to seek approval for their training from the Society’s Learning Centre (www.bps.org.uk/learningcentre), enabling supervisors who successfully complete the training to apply for entry to the Society’s Register of Applied Psychology Practice Supervisors.
2.3 It is important that supervisors keep abreast of theoretical, research and professional developments in their fields of work and participate in continuing professional development.
3. Allocation to Clinical Placements
3.1 There should be an explicit procedure for allocating trainees to clinical placements. All trainees and supervisors involved should understand the procedure and know how to influence decisions about clinical placements. The person responsible for arranging placements should give primacy to general training requirements and competency development needs but should also take account of the needs of individual trainees. Information should be provided about the experience obtainable in the various placements to help trainees and programme staff to make placement decisions.
3.2 The Programme should try to ensure effective co-working for trainees who are sharing the same placement. This is especially important where there is team supervision, with two trainees allocated to one supervisor, or when two or more trainees receive supervision from a team of supervisors, within the same placement.
4. Setting up the Placement
4.1 Both trainee(s) and supervisor(s) must have an opportunity to meet either before, or at the very beginning of the placement to discuss the range of experience, which is to be provided, and the expectations (hours, days of work, etc) of the trainee(s). The general aims of the placement should normally be agreed within the first two weeks of the placement and a clinical contract should be written. Attention must be paid in the clinical contract to the range of opportunities available in the placement, and to the needs, interests and previous experience of the trainee. Particular efforts should be made to fill major gaps in the trainee’s experience, and records of the trainee’s previous experience should be available for this purpose. The Programme Director or Clinical Tutor will have played a major role in the assessment of the trainee’s strengths and needs and in the sequence of placements.
4.2 In cases where there is more than one supervisor involved in a trainee’s placement (team supervision) a primary supervisor must be identified for each trainee who will take responsibility for the planning and co-ordination of that trainee’s placement, supervision and assessment, and for liaison with Programme staff.
4.3 The supervisor must plan an induction for the trainee, arrange for cover in the event of annual or other leave and should plan casework well in advance.
4.4 Care should be taken to ensure that the trainee has access to (at least) shared office space, telephone and a desk. There must be adequate arrangements for secretarial and IT support for placement work and trainees must be given guidance on the facilities available.
4.5 Supervisors must remember that they have clinical and legal responsibilities for their trainees throughout the training period. It is good practice for supervisors to be insured, for trainees to be aware of relevant legal boundaries (e.g. re. the Data Protection Act, the Children Act). It is essential that trainees have appropriate (substantive or honorary) contracts that allow them to work in their placement.
5. Placement Content
5.1 Programmes must develop, in consultation with the Division of Clinical Psychology’s Faculties and Special Interest Groups and local supervisors, guidelines on the required experience in clinical placements, recommending an appropriate amount of clinical work.
5.2 The local guidelines on placement content should be taken into account in the provision of placement experience for the trainee. The level of his/her experience and expertise and the stage of training will determine the particular balance of work for each individual trainee.
5.3 Supervisors should ensure that trainees undertake an appropriate quantity of clinical work. There are dangers in both extremes: too little work reduces the opportunity for learning and too much may reduce trainees’ capacity for planning or reflecting upon the work. Supervisors should monitor the balance of time spent by the trainee on work at different levels (direct client work, indirect and organisational work). This balance will vary according to the stage of training and the type of placement. Supervisors should be alert to the dangers of time being lost at the start of the placement through suitable work not being available and should take this into account in preparing for the arrival of the trainee.
5.4 A log must be kept of the work a trainee has done in a clinical placement. The programme must ensure that the Clinical Tutor appropriately uses these records in planning future placements and by future clinical supervisors in discussing what experience they should provide.
5.5 With team supervision, the programme should give clear guidelines about the experience to be acquired so that the placement may be planned to make optimal use of others involved in providing supervision.
6. Clinical Supervision
6.1 There must be a formal, scheduled supervision meeting each week that must be of at least an hour’s duration. Longer supervision will sometimes be needed, especially where team or group supervision is used. In addition, supervisors should try to make themselves available for informal discussion of matters that arise between formal supervision sessions. The total contact between the trainee(s) and supervisor(s) must be at least three hours a week, and will need to be considerably longer than this time at the beginning of training.
6.2 In cases of team or group supervision, trainees must always receive, in addition, an appropriate amount of individual supervision. Individual supervision must provide opportunities to discuss personal issues, professional development, overall workload and organisational difficulties as well as on-going casework.
6.3 Adequate time for clinically relevant reading must be made available to the trainee on placement. In addition, supervisors have a crucial role in contributing to the integration of the academic and practical aspects of the Programme. They should discuss literature relevant to the clinical work in hand and suggest suitable reading to the trainee. In general they should help trainees to develop a scholarly and critical approach to their clinical work.
6.4 In addition to discussing clinical work, it is essential that the trainees and supervisors have opportunities to observe each other at work: the trainee can learn much more from this and it is essential in order for the supervisor to give the trainee accurate and constructive feedback. Placements differ in the most appropriate opportunities for such direct contact: some may use joint clinical work of some kind; others may prefer audiotape, videotape or a one-way screen. Some form of mutual observation of clinical work is regarded as essential.
7. Quality of Clinical Supervision
7.1 The quality of the supervision that is provided for the trainee will depend upon many factors. The care taken in the early stages to build up a good relationship will enhance the quality of the clinical supervision.
7.2 Supervisors should be prepared to adapt their style of supervision to the stage of the programme a trainee has reached. It is necessary to be prepared to describe basic clinical procedures in detail and to ensure that trainees have an adequate grasp of techniques they are asked to use. Detailed training in techniques should also be available to more experienced trainees if required.
7.3 Trainees and supervisors may find that they have a different orientation and interests. Where this happens tolerance should be shown on both sides. Trainees should be helped to see that they might learn much that is valuable from a supervisor whose approach they may not ultimately wish to adopt. On the other hand, supervisors should see it as one of their functions to help trainees develop their own interests in an appropriate way. Where supervisors decide they must overrule the way the trainee wishes to work, they should explain their reasons with care, rather than simply asserting that this is how things should be done.
7.4 Supervisors should be prepared to discuss seriously and sympathetically any general issues of relationships with patients or staff that arise in the programme of clinical work. They should be sensitive to any personal issues that arise for the trainees in relation to clients and be prepared to discuss these in a supportive way when they are considered to affect the trainee’s work. The range of personal issues that can be raised by clinical work is wide and includes, for example, over-involvement, dealing with anger and despair, workload and time management problems.
8. Clinical Reports and Communication
8.1 Communication with other members of clinical teams and networks involves both written and verbal reports. Verbal reporting and discussion are often more important than formal written reports in terms of their effects on clinical decisions and action. Since the relative importance of written and oral communication is likely to vary between settings, supervisors will need to identify the most important channels of communication in their placement and teach the trainee to use these channels effectively and efficiently. Training in effective communication will involve both observation of the supervisor’s behaviour, and practice by the trainee with ample opportunity for feedback.
8.2 There is a wide variation within the profession in how clinical reports are written and presented, particularly with respect to the amount of detailed information provided. Trainees need to be acquainted with a variety of report and letter writing styles. If there is agreement about minimal requirements of clarity and relevance in reports, exposure to individual differences between supervisors is more likely to be constructive than confusing. Trainees should be encouraged to write reports that are appropriate to the recipient (whether this is a professional colleague or a client), avoid jargon, distinguish clearly between fact and opinion, and provide consistent clarity of expression. Both supervisor and trainee should be aware of the potential conflict between communicating fully to professional colleagues and maintaining confidentiality.
9. Review Meetings and Feedback
9.1 There must be a formal process during each placement whereby the Programme team monitors the clinical experience of trainees and the supervision provided, and helps to resolve any problems that may have arisen. The aims of this are:
- to review the progress of the clinical contract
- to give feedback to the trainee on his/her clinical performance
- to allow the trainee to comment on the adequacy of the placement
- to set targets based upon the above for the remainder of the placement
- to give feedback to the supervisor on his/her performance.
9.2 When a trainee is involved with some form of team supervision, the programme must ensure that each trainee’s experience is monitored on an individual basis. Other review or feedback of meetings that may be held at the beginning and end of a placement should also allow for individual time allocation for each trainee. If possible, all team supervisors involved with any single trainee should be involved in the monitoring process (and beginning and end of placement meetings). Where it is not possible for all a trainee’s supervisors to be present at a key review meeting, one designated supervisor should seek views from other team supervisors prior to the meeting, and provide feedback after the meeting.
9.3 Matters such as the physical resources available to the trainee (room space, secretarial backup, etc) and theory-practice links may also be usefully discussed at this time. Supervisors and trainees may find it helpful in the review to go through the rating forms that will be used at the end of the placement.
9.4 In general, it is expected that the programme staff member conducting the monitoring will hold discussions with the trainee and supervisor separately and then hold a joint discussion. In this way more accurate feedback about the trainee’s performance and about the quality of the supervision provided may be obtained. The timing of the monitoring is important if sufficient time is to be left for improvements to be made. A plan and timetable for the review should be agreed at the start of the placement.
9.5 Mid placement qualitative feedback is essential both for the supervisor and the trainee. Supervisors should try to set aside positive or negative personal feelings about trainees when making evaluations. Feedback should be detailed and constructive and designed to help trainees develop a range of effective and appropriate skills; thus, feedback should be critical but not wholly negative.
9.6 If seriously dissatisfied about aspects of a trainee’s performance, supervisors should regard themselves as under an obligation to the profession to indicate this to the programme staff.
9.7 The trainee also has a responsibility to the programme and to the profession to give feedback to the programme staff about the quality of the placement and the supervision.
9.8 At the end of the placement the supervisor must give the trainee full feedback on his/her clinical performance. The trainee must see the supervisor’s written assessment. Any major points that the supervisor is concerned about should normally have been raised well beforehand, at least during the formal monitoring process, to allow the trainee time to improve. The trainee must also have ample opportunity to comment on the placement, for example, on the experience and the supervision received. The trainee’s views should be recorded formally as part of the general evaluation of the placement. Feedback forms and forms for rating clinical competence should always be completed at the time of the end of placement review and returned promptly.
9.9 The points made in section 9.5 concerning the provision of balanced, constructive and detailed feedback to the trainee also apply to the end of placement review. The supervisor should, in addition, help the trainee to identify gaps in his/her experience to facilitate planning for subsequent placements. It is important for the supervisor and trainee to forward this information to the person responsible for co-ordinating placements.
10. Assessment of Clinical Competence
10.1 It is important that supervisors are familiar with the examination and continuous assessment requirements for trainees and the guidelines and regulations for these.
10.2 In cases of team supervision, all supervisors who have been involved with the trainee(s) must be familiar with the programme’s assessment procedure and must give feedback on the trainee(s) clinical competence.
10.3 Supervisors must be familiar with the specific criteria for passing and failing in the assessment of clinical competence set by the programme. In addition, supervisors should be aware of appeals procedures. In cases where trainees have displayed unsatisfactory behaviour, such as regular and serious lateness for clinical appointments, professional misconduct, or failure to acquire an adequate level of clinical competence, trainees must be left in no doubt about the problem. The supervisors should discuss with the Clinical Tutor what action should be taken and it may be helpful to have a member of the programme staff present at the time of the end of placement review.
Supervisor Training
In its Guidance for Clinical Psychology Programmes (2010), the British Psychological Society requires training programmes to provide training for supervisors, and in Manchester this is well established. The Health and Care Professions Council also has some minimal standards concerning supervisors. The Clinical Directors arrange the training events with input from other members of the Programme Team. All supervisors are informed of these and encouraged to attend.
Feedback is routinely sought from supervisors and developments made to the workshops incorporating this and evidence from the research/literature base. The Manchester Programme has been in the forefront of the Clinical Supervision Advisory group (CSAG) which has helped develop the BPS accreditation procedure for supervisors.
The ClinPsyD Programme provides an annual cycle of training which spans 10 months. The training is four days long and consists of 2 days in February followed by a day in May and a fourth day in November. The course has a developmental structure with supervisors needing to attend in chronological order. The Programme is keen to evaluate the impact of the training on supervisors’ performance and participants are required to complete some work in the form of a portfolio within 12 months of the start of training. The portfolio needs to be submitted in the February following the start of training and written formative feedback with be given on this in April . On completion of the training, supervisors will be eligible for recommendation to join the BPS Register for Applied Psychology Practice Supervisors (RAPPS).
Each year the proposed schedule is as follows (all dates to be confirmed):
| Day 1 and 2 | February | An introduction to supervision. Why supervise? What does supervising involve? Identifying the tasks and skills that are needed in supervision. How does learning take place in supervision? |
|---|---|---|
| Day 3 | May | The Supervisory relationship. Supervision and diversity. Developing your skills as a Supervisor. |
| Day 4 | November | How should we evaluate supervision? Maintaining good practice in supervision. Current developments in supervision. |
Training takes place at the Programme base in the Zochonis Building, The University of Manchester, between 9.30 and 4.30.
Advanced Supervisor Training
In addition to the Introductory Supervisor Training Programme, the three North West ClinPsyD Programmes also jointly provide a minimum of two Advanced Supervisor Workshops per year, which are open to all supervisors who have two or more years’ experience of providing supervision. These usually run in May and November and cover a range of topics, all focussed on encouraging the sharing of ideas and best practice. Recent topics include:
- Providing accurate feedback to trainees
- Managing strong feelings in supervision
- Group supervision
- Attachment and Supervision
These workshops are periodically advertised to all current and previous supervisors but supervisors are also encouraged to contact the Clinical Tutors to find out more or to suggest potential topics.
Reading List
The following is a selected list of useful books and papers. There is a vast literature available on the subject in general, but less about Clinical Psychology and the NHS context
- Campbell, D. & Mason B. (2002). Becoming an effective Supervisor. Ann Arbor MI: Sheridan Books.
- Dennis, M. (1998). Is There a Place for Diversity Within Supervision? An Exploration of Ethnic and Cultural Issues. Clinical Psychology Forum, 118, 24-33
- Falendar, C.A. & Shafranske, E. P. (2004). Clinical Supervision: A Competency–based approach. Washington DC: APA.
- Fleming, I. & Steen, L. (2001). Supervisor Training on the Manchester Clin.Psy.D. Course. Clinical Psychology, 8, 30-35
- Fleming, I. & Steen, L. (Eds.) (2012). Supervision and Clinical Psychology: Theory, Practice and Perspectives 2nd Edition. Hove: Brunner-Routledge
- Green, D. & Youngson, S. (2005). Discussion paper regarding DCP Policy on Continued Supervision. Leicester: British Psychological Society
- Hawkins, P & Shohet, R. (2012). Supervision in the Helping Professions (4thd Edition). Milton Keynes: Open University Press
- Milne, D. (2009). Evidence-based Clinical Supervision: Principles and Practice. Chichester: John Wiley & Sons
- Milne, D. & James, I. (2002). The observed impact of training on competence in clinical supervision. British Journal of Clinical Psychology, 41, 55-72
- Scaife, J. (2009). Supervision in clinical practice: a practitioner’s guide (2nd edition). Hove: Brunner Routledge
- Watkins, C. E. & Milne, D. L. (Eds.) (2014). Wiley International Handbook of Clinical Supervision. New York: Wiley – Blackwell
Guidelines for Completion of the Supervisor’s Assessment of Trainee Form
At the end of the placement, the supervisor is asked to provide a report on the trainee’s performance; the trainee should see this report and have a chance to discuss it with the supervisor before he/she submits it.
The guidelines below have been prepared to assist Supervisors in completing the ‘Supervisor’s Assessment of Trainee Form’ (SAT – see form on the intranet). If a supervisor is uncertain of their interpretation or feels an issue has arisen to which they do not readily apply, she/he should not hesitate to contact the Clinical Tutors for further clarification. This form should be discussed with the trainee at the middle and the end of the placement and completed at the end of the placement.
Supervisors are able to access the SAT form on the intranet and will also be able to view SATs from previous placements.
The ‘Supervisor’s Assessment of Trainee Form’ (SAT) comprises two main sections, namely Transferable Competencies and Specific Competencies. Items for the Transferable Competencies section derive from a job analysis of the role of a trainee clinical psychologist. The Specific Competencies section incorporates the broad areas of competence set out in the British Psychological Society’s (BPS) Accreditation Through Partnership: Guidance for Clinical Psychology Programmes (2012) and Standards for the Accreditation of Doctoral programmes in clinical psychology (2016) and the Health and Care Professions (HCPC) Standards of Proficiency for Practitioner Psychologists (2015).
Required Objectives that Demonstrate Competence
(full descriptions for all the competencies listed below can be found on the SAT form)
1. Transferable Competencies
A commitment to inclusivity: Demonstrating a clear understanding of the issues around inequality and a commitment to inclusive practice.
Verbal and non-verbal communication skills: Using clear concise language and conveying complex ideas coherently. Communication is adapted to the needs and understanding of the listener or audience. Non-verbal communication is inclusive and congruent with the verbal message.
Self awareness and openness to learning: Having insight into own behaviour, emotions and motivations and how they interact with the work undertaken. Demonstrating moving towards resolution of any unresolved issues. Actively seeking and learning from feedback.
Personal maturity: Taking responsibility for own actions and anticipating consequences of own actions. Showing realistic confidence in their own ability and has the courage to deal with difficult issues. Demonstrating an appropriate level of autonomy.
Warmth and empathy: Relating respectfully to others, acknowledging the unique perspective of others and not making negative assumptions about their actions.
Resilience: Coping well with pressure, tolerating anxiety and uncertainty but seeking support where needed. Responds robustly and sensitively in the face of conflict and regulates and manages own emotions, enjoying a challenge and showing flexibility when required. Engages in appropriate self-care.
Professional skills: Using time effectively and working systematically, anticipating difficulties and taking action in good time. Is punctual, reliable and meets deadlines.
Motivation and application: Working hard and with enthusiasm. Committed to completing tasks as well as possible.
Contextual awareness: Understanding psychological health problems in social, economic, political and cultural context. Engaging critically with accepted practice. Showing an understanding of the organisations and agencies involved in health and social care.
Problem-solving and decision-making: Exercising good judgment in making decisions and has a creative approach. Enjoying an intellectual challenge.
Ethical practice and decision making: Practising in an ethical manner (e.g. respecting boundaries and confidentiality); Has awareness of the complexity surrounding ethical issues and dilemmas, and approaches these in a systematic and balanced manner.
Interpersonal skills: Demonstrating an awareness of interpersonal dynamics, social cues and social skills, responding appropriately and sensitively.
2. Specific Competencies
Assessment: Clinical assessment and/or assessment in a broader sense e.g. a group, a family or a staff team.
Formulation: developing formulations is a central competence of the profession; formulations:
· are built collaboratively,
· inform the understanding of clients, carers and other professionals,
· draw upon psychological theory and evidence,
· have explanatory power,
· take intrapsychic and social contexts into account,
· guide the best next steps
· can be revised and reformulated in the light of ongoing work and
· can be formulation in a broader sense e.g. a systematic understanding of an organisational issue.
Intervention: Clinical intervention and/or intervention in a broader sense e.g. in terms of changing a team dynamic, providing training etc
Evaluation: Clinical evaluation and/or evaluation of a non-clinical intervention. Selecting the appropriate methods and evaluating in a way which gives a clear picture of outcome in the most respectful and ethical way possible. The ability to critique evaluations.
Teaching: Teaching or training others effectively, including establishing a clear rationale and learning outcomes, appropriate planning, selection of materials and mode of teaching or training and evaluation.
Consultation: Facilitating the learning and reflections of others in clinical and non-clinical work, offering advice and support as appropriate. This may be on one occasion or more frequently.
Supervision of others: Developing a close ongoing relationship with one or more others to facilitate reflection and learning in a specific clinical or non-clinical context. This would normally take place over a number of sessions or throughout the piece of work undertaken.
Service development: Making a contribution to the processes involved in improving existing services or developing new services. Using the relevant evidence base, consultation skills, networking, persuasion and facilitation skills appropriately. This may also include written work (e.g. contributing to proposals, bids, briefs and reports).
Risk assessment: Assessing risk in accordance with the relevant policies and procedures. Demonstrating both a sensitivity to risk issues and a sound knowledge of relevant evidence.
Keeping records and information governance: Keeping records in accordance with the requirements of relevant policies and procedures. Demonstrating competence in handling sensitive and personal information and understanding why this is important.
Knowledge and creative application of specific psychological theory or approach: Demonstrating a sound working knowledge of a specific psychological theory or model. This is applied creatively to match the context where appropriate.
Community engagement skills: Considering contextual factors including culture, social structure, and empowerment to identify community needs, strengths and resources. Identifying key stakeholders and creating and sustaining partnerships with them.
Facilitating meetings or collaborative projects: Facilitating meetings, group decision-making, and consensus building. Assisting with conflict resolution where appropriate.
Written communication: Ensuring letters, reports, notes, proposals, bids, policy briefs and other documents are well expressed and match the needs of the intended audience.
Working alongside service users: Co-creating facilitative and effective partnerships with service users to support meaningful participation in service development and delivery.
Multi-professional liaison: Developing constructive work partnerships across professional boundaries to ensure the best outcome for service users.
Service audit: Understanding the professional, practical and ethical issues involved in undertaking audit and research in a service setting, and in the analysis and dissemination of findings as appropriate.
Managing a reasonable workload: Sustaining a full and diverse workload appropriate for the amount of available time on placement and sufficient to facilitate the achievement of the range of required competencies on the placement.
How to Complete the ‘Supervisor Assessment of Trainee’ Form
Written Feedback
The ‘Supervisor’s Assessment of Trainee Form’ is designed to provide feedback to the trainee in order to help her/him develop core skills. At the end of each placement supervisors are asked to rate trainees and provide feedback on their performance on each area of competence. Supervisors are encouraged to give detailed written feedback where possible and appropriate, including examples to support feedback as these will be used by the trainee and clinical tutor to form the basis for setting learning objectives for future placements.
Rating Scales
In addition to providing written feedback on each of the key competence areas, supervisors are asked to give a rating as a recommendation to the Examiners on whether the various aspects of the trainee’s performance on placement have been satisfactory, and whether performance on the placement as a whole has been satisfactory.
There are two levels of rating:
- Each of the individual competence areas (Satisfactory/Requires Attention*/Unsatisfactory/No Opportunity) * for the final placement, ‘CPD recommendation’ is used in place of ‘requires attention’
- Supervisor’s Overall Rating (Satisfactory/Unsatisfactory)
In arriving at a rating, the following points should be considered:
- The rating should reflect the expected level of competence for the trainee’s stage in training– for example, what is considered a satisfactory level of performance for a first year trainee at the end of his/her first placement may not be viewed as appropriate for a trainee on the final placement of the third year
- A rating of ‘requires attention’ should be given to reflect some limited degree of concern over aspects of the trainee’s performance. It is still a pass grade and is to be used as formative feedback
- No opportunity: This rating should be given if the trainee did not have the opportunity to develop the competency or to work on achieving the learning outcome for this particular competency area
- In the case of a rating indicating ‘requires attention’ or ‘unsatisfactory’, the Clinical Tutor, in collaboration with the Supervisor, will specify work to be undertaken on subsequent placements; if this is on a final placement, provided the trainee is given an overall rating of ‘Satisfactory’, recommendations for CPD will be made
Supervisor’s Overall Evaluation
This rating signifies the “gate keeping” aspect of evaluation. The main criterion being used is whether the trainee is ready to move on to the next stage of training. As such, the standard should be adjusted to take account of the length of time a trainee has been on the programme. The definitions of the ratings are given below:
- Satisfactory:The supervisor considers that the trainee is ready to move on to the next stage of training.
- Unsatisfactory:The supervisor considers that the trainee is not yet ready either to move on to the next stage in training or to carry out further less closely supervised work in this area without definite assistance in addressing specified issues.
In arriving at a rating, the following points should be considered:
- One would expect a relationship between the Overall Rating and those given for the competence areas described earlier.
- If an unsatisfactory rating is given for more than one of the competence areas or if conduct is unethical or seriously unprofessional then an ‘unsatisfactory’ rating should be given as an overall rating. The reasons for the ratings should be obvious from the written comments in the section
- If a Supervisor is considering giving an Overall Rating of ‘unsatisfactory’, she/he should always discuss this with the clinical tutor in advance. This is discussed in detail in the next part (6).
All decisions are subject to ratification by the Examination Board.
General Comments
This can be used either to expand on comments previously made or to introduce points not covered in other sections of the form.
Recommendations
This refers to any needs that should be addressed on future placements. The more detailed the recommendations, the more helpful this is likely to be for both the trainee and future supervisors.
Trainee’s Comments
This is an opportunity for the trainee to comment on the ratings and feedback given by the supervisor.
On Completion
The form should be given to the trainee so that she/he has time to read it in advance of discussing it with the supervisor. Having discussed it, the form should be signed by the supervisor, initialled by the trainee and trainee’s comments added. By initialling it, the trainee is not indicating that she/he necessarily agrees with all of the ratings or comments, simply that she/he has had the opportunity to discuss them. Two copies of the form should then be made, one to be retained by the trainee, another by the supervisor, with the original being sent to Alison Cox, Clinical Programme Administrator by the last day of the placement. This is the responsibility of the trainee.
Placement Contracts, Visits and Feedback
Placement Contract
The development and agreement of a clear contract between the trainee and supervisor at the commencement of each placement helps to guide the training experience and to prevent later difficulties if supervisor and trainee feel that expectations are not being met. The contract is a signed agreement on the content of the placement experience, the Intended Learning Outcomes and the form that the supervisory relationship will take, as referred to in the BPS Guidelines on Clinical Supervision.
The trainee may feel less able to play such a part in the development of the contract for the first placement at the beginning of the programme, but should still be able to contribute information about his/her perceived strengths. For second and subsequent placements it is expected that the trainee will play an active role in developing the placement contract. The trainee’s particular expectations should be considered within the scope of the placement. The individual’s Clinical Portfolio, the ‘Supervisor’s Assessment of Trainee Form’ from the preceding placement and the Clinical Tutor’s placement visit reports must be used in this process. It is hoped that, with guidance from their Clinical Tutor, trainees developing their Year 3 contracts will consider not only any outstanding learning needs but also preparation for the transition to qualification.
The placement contract should be developed using the standard pro forma (see ‘Download’ section on intranet). Trainees or supervisors are welcome to speak with the trainee’s Clinical Tutor if they are unsure about what to include. It may also be helpful to refer to the Placement Guidelines (on the intranet) for examples of the core experiences expected from specific placements.
NHS constitution
It is essential that trainees and supervisors think about how the NHS constitutional core values are embedded in the placement and this can be described in the placement contract. Further information about this can be found in the NHS constitution section of the handbook.
Psychological Contract
In addition to a Placement Contract, which sets out expectations about clinical work and the practicalities of supervision, trainees and supervisors are required to draw up a Psychological contract (available on the intranet). The Psychological Contract makes explicit both the trainee’s and supervisor’s expectations of each other and helps to develop a positive supervisory relationship
- How are supervisor and trainee going to relate to each other?
- What expectations do each have of the other?
- What is the role of each?
The supervision literature (e.g. Hawkins and Shohet, 2012; see Supervisor Reading List) suggests that if these issues can be made explicit and agreed upon then the process of learning will be enhanced. It is hoped that this contract will help form an open and trusting Supervisory relationship by making the expectations clear on all sides.
We would like you and your supervisor to consider the following key points that make up the psychological contract; please feel free to add any additional information that you feel is relevant. It may be useful to reflect on previous experiences to develop this contract:
- What I value most in supervision (from both trainee and supervisor perspectives)
- What I value least in supervision (from both trainee and supervisor perspectives)
- Practicalities and boundaries of supervision
- When, where, how frequently will we meet?
- What are the boundaries of the relationship and how can these be protected?
- Who has ultimate responsibility for the work?
- Style of supervision
- How would we like our work to be discussed or presented?
- How we will provide feedback to each other? / How will we act on this and react to this?
- Supervisory Relationship
- What do I feel I need from my supervisor / trainee? What would I not want from my supervisor / trainee?
- Conditions that will help the relationship to work well
- What if difficulties arise within our Supervisory relationship, how will we manage/resolve them?
Once the contract has been drawn up, it is important to remember that this should be reviewed periodically and modified in the light of experiences; any lapses in fulfilling the contract should be viewed as opportunities for reflection and learning.
Please return the contract to Alison Cox within the first two weeks of starting the placement. If you have any difficulties in completing the psychological contract please discuss further with your clinical tutor.
Placement Meetings with the Clinical Tutor
For the purposes of the Examination Board, training is divided into 4 six-month placement periods and 1 nine-month placement period over three years. The Programme formally monitors progress in each placement period through the mid-placement visit and the end of placement visit. Each trainee is allocated a Clinical Tutor at the start of training. This is a member of the Programme Team who monitors the trainee’s clinical experience throughout the three years of the Programme (unless there are changes to the staff team or exceptional circumstances).
This section describes the placement meetings that take place between the trainee and his/her clinical tutor. Before looking at these, the initial meeting between the clinical tutor and trainee is described. This section should be read alongside the section regarding academic guidance and tutorial support in the handbook.
Commencement of Training
At the beginning of training, there will be a meeting between the trainee and clinical tutor. This meeting serves several functions. The trainee and Clinical Tutor have a chance to get to know each other a little, and discuss what the Clinical Tutor’s role is in relation to training. Particular training needs can be identified, which can be carried through as objectives for training on placement. Anxieties that the trainee may have about the Programme can be identified and addressed. Further, the trainee should be given the opportunity to raise any personal concerns which may be affecting them at the time; worries over moving into a new setting, housing problems and separations are all common at this time.
The Mid-placement Visit
The Clinical Tutor visits each placement at about the mid-point. The purpose of the visit is to:
- Monitor the clinical work and performance of the trainee through (a) a report from the trainee of work undertaken to date and (b) a report from the supervisor of his/her view of the trainee’s functioning.
- Monitor the extent to which the Intended Learning Outcomes (as recorded in the Portfolio) of the placement are being met and to suggest corrective action if necessary.
- Monitor the opportunities provided by the setting in terms of suitability for future trainees.
- Monitor the performance of the supervisor, particularly adherence to the BPS Guidelines on Clinical Supervision.
- Identify gaps in the experience of the trainee which may be rectified during the remainder of the placement.
- Negotiate any difficulties which may have arisen at a personal or professional level between supervisor and trainee.
- Facilitate feedback between supervisor and trainee in relation to the trainee’s progress and performance and the supervision and training opportunities.
- Identify any other areas, be they academic or personal, that may be affecting the trainee.
Visits are arranged some weeks in advance; the Clinical Tutor will contact the trainee to arrange the meeting in the first week or two of the placement via email or telephone.
- For October – April placements, the visit takes place in December-January
- For April – October placements, the visit takes place in June-July
- For Year 3 placements, the visits will take place in early May and September, and the clinical tutor will organise an informal meeting with the trainee prior to the start of placement.
It is recommended that the ‘Supervisor’s Assessment of Trainee’ form and ‘Trainee Evaluation of Placement’ form are used as a framework for a mid-placement review. The forms need not, however, be completed at this time.
An example of a timetable for a visit is shown below. Timings are approximate, as different visits may require more or less discussion of particular issues, and should act only as a guide to the amount of time that should be made available for the visit.
| 45 minutes – 1 hour | Trainee meets with clinical tutor |
| 30 minutes | Supervisor meets with clinical tutor |
| 15 minutes | Joint Meeting |
Trainee meets with Clinical Tutor
During the first session, the trainee gives an account of his/her work and view of the placement and Supervisor. The Clinical Portfolio, ‘Trainee Evaluation of Placement’ form and Placement Contract may be used as a guide in this session. The contract and objectives will be reviewed. The Clinical Tutor should discuss (1) placement related issues, (2) academic progress and possible anxieties and (3) give the trainee the opportunity to discuss any personal issues that may be of relevance or which they may wish to raise.
If the trainee is clearly troubled about issues of any kind, it may be necessary to arrange a separate opportunity to meet and discuss these outside the placement setting. In this case, the tutor should consider whether the trainee should be guided towards other parts of the network, be it one of the Clinical Tutors, Academic Advisor, Academic Staff or other personal support systems and networks.
Supervisor meets with Clinical Tutor
In the session with the supervisor, they are encouraged to reflect on the training opportunities offered as well as give a report on the trainee’s progress and any issues which may need addressing. The ‘Supervisor’s Assessment of Trainee’ form should be used as a guide to areas to be covered. The tutor may meet with the supervisor individually or may have a joint meeting with the supervisor and trainee so that feedback from the supervisor can be given directly to the trainee. This will be discussed beforehand.
Joint meeting
The joint session is an opportunity for the Clinical Tutor to focus on the placement contract and learning objectives which can be reviewed and, if necessary, amended. The ‘Trainee Evaluation of Placement’ form and the ‘Supervisor’s Assessment of Trainee’ form can be used to encourage mutual feedback between supervisor and trainee. Concerns over other issues that the trainee has raised, be they academic or personal, should only be raised with the supervisor with the trainee’s permission.
Following the visit, the Clinical Tutor will provide the trainee and supervisor(s) with a written summary of the visit with any recommendations for the remainder of the placement. A copy of this report is retained by the programme and is held in the portfolio.
The End of placement review
The trainee may have completed the ‘Trainee Evaluation of Placement’ form and have the Clinical Portfolio as up to date as possible and the supervisor will have completed the ‘Supervisor’s Assessment of Trainee’ form. In this review, objectives for the forthcoming placement should be identified and any omissions in the range of experience noted, so that these can be made up in future placements. in the case of a final year placement, recommendations for CPD will be made.
The Clinical Tutor will provide a written summary of the visit with recommendations for further placement experience.
Feedback About and Evaluation of Placements
Trainees are required to complete a Trainee Evaluation of Placement form (see ‘Download’ section of intranet) at the end of each placement. This evaluation broadly encompasses an assessment of:
- Induction and practicalities of the placement
- Experience of supervision
- Wider service issues
- Placement related support
- Opportunity to develop core competencies
There is also the opportunity for the Trainee to provide an overall evaluation of their experience of the placement.
Trainees are required to share the Trainee Evaluation of Placement form at the end of placement and discuss this with their supervisor. They submit the form electronically along with the Clinical Portfolio and supervisors are required to sign the form off and add their own comments at this point.
Supervisors are of course welcome to retain a copy of the Trainee Evaluation of Placement form for their own records. The Programme will also publish an annual report which provides an anonymous summary of Trainees’ experiences of placements and highlights any common themes that have arisen.
Supervisors and trainees work to develop a relationship where feedback on both sides is an on-going process. The use of placement contracts, psychological contracts, learning objectives and the two evaluation forms (Supervisor of trainee and Trainee of placement) should be seen as assisting, not replacing this. Explicit reference to the forms and contracts at the beginning, middle and end of placement will help with overall reviewing of the work. Supervisors are encouraged to help trainees identify and work on areas which need development, as well as giving positive feedback on strengths; equally, they need to be open to the trainees’ views on the helpfulness of supervision and placement experience.
From October 2019, trainees will be expected to seek direct feedback from people they work with clinically on placement. Please click the link for the relevant information and forms.
Getting the Most out of Placement
Placement arrangements
Making timely and appropriate arrangements will help you get the most of placement. The table below summarises the key arrangements in this regard.
| At least 1 month before start of placement | Pre-Placement Planning | |
|---|---|---|
Supervisor
|
Trainee
|
|
| Approx 2-4 weeks prior to placement | Pre-Placement Visit | |
|
||
| At start of placement | Induction programme | |
| Within first 2 weeks | Placement objectives and contract | |
|
||
| One copy of placement and psychological contract to be sent to placement administrator within two weeks of the start of placement | ||
| At mid point | Mid-Placement Visit | |
| In preparation for visit, supervisor and trainee to:Review contractsLook through end of placement forms | ||
| Just prior to end of placement | End of Placement Visit | |
| In preparation for visit:Supervisor to have completed Supervisor’s Assessment of Trainee formTrainee to have completed Trainee Evaluation of Placement (TEP) form and Clinical Portfolio | ||
| One copy of all documents to be sent to placement administrator (deadline set at beginning of placement) | ||
| Placement Changeover Week | ||
| Supervisor to read trainee’s case report and sign validation formTrainee to ensure that all training documentation and placement administrative procedures are completed | ||
The following comments are based on a collaborative effort between past trainees and the ‘Placement Forum’, formerly ‘Supervisors Sub-Committee’, who wanted to provide some guidelines that would help to improve the quality of the supervisory experience for both trainee and supervisor. They are presented as an informal set of guidelines for good supervisory practice.
Preparation for Placement
In advance of Trainees starting on placement, Supervisors are asked to consider:
- How formal and informal contact time will be facilitated and what the arrangements will be for trainees to seek advice when supervisors are unavailable
- What arrangements need to be made in terms of accommodation and secretarial support
- Making colleagues aware of the trainee’s arrival, likely responsibilities etc
Trainees are required to make contact with supervisors prior to the start of placement and, where possible, arrange a visit. The aim of this meeting is for supervisor and trainee to begin to get to know each other and discuss:
- Broadly what the service provides and what the placement will entail
- The trainee’s past experience
- Any hopes and fears about the placement from either party
Booking in clients
Both trainees and supervisors frequently describe a sense of frustration when the clinical work on placement is slow to take off, for example where there have been high rates of cancellations and DNAs. If supervisors feel that it is appropriate within the placement being offered then they are encouraged to book in 3-4 clients in advance for the second or third week of placement in order to allow for this. The amount and type of work is something that can be discussed at the pre placement visit.
Induction
Both supervisors and trainees describe finding it most helpful if plans are in place for the first few weeks of placement before the trainee arrives. These plans might include provision of a placement information pack (see below). It can be particularly important to discuss aspects of the work that can be taken for granted within departments, for example:
Written communications
Supervisors should give trainees clear guidance on the particular procedures and expectations within the department concerning written communication, and should read through draft reports and provide constructive feedback. Departments and supervisors differ across the region in terms of the requirements for written work, and supervisors should anticipate this and help to ease the trainee into the placement with an explanation of what is required.
Professional conduct
Similarly, departments differ in their expectations concerning dress, timekeeping and so on. Please ensure that your trainee is not left in a state of confusion over this, which could lead to difficulty later.
What might a placement information pack include?
The following types of information can often be helpful for trainees starting placement:
- Who’s who within the department – names and service structure
- Who are the client group and how do they access a service?
- Map of the locality and any useful information about demographics / social context
- Suggestions for professionals / organisations to speak with / visit / shadow (and/ or a timetable for doing so)
- Administrative procedures – note keeping, letters, secretarial support etc
- Coffee arrangements, library use, departmental ‘traditions’
- Professional issues – departmental protocols, dress, time-keeping etc
- Health and safety arrangements
Placement ‘Handover’ Period
At the end of each placement there are days that have become known as the `change-over` period. Each of these periods are indicated on the annual calendar for the programme.
There are a number of tasks to be achieved during this period and it is not to be considered annual leave although annual leave can be taken by arrangement on those days that are not already designated and once the tasks set out below have been accomplished.
The main aim of the handover period is to enable the various documents that accompany the training placement (for example Clinical Portfolio, Supervisor’s Assessment of Trainee Form and Trainee Evaluation of Placement Form) to be completed and to ensure that case notes and correspondence are complete. This might involve completing administrative and discharge procedures, for example. If all of these tasks have been completed then the remaining time may be taken as annual leave by prior arrangement with supervisors.
What happens if a Trainee’s Performance on Placement is Unsatisfactory?
Overview
This section sets out the procedure to be followed when a supervisor considers that their trainee may merit an overall rating of ‘unsatisfactory’ on placement. Central to this procedure is that the Clinical Director must be involved in assigning the overall placement grade in such circumstances. The main reason for this procedure is to try to ensure that an appropriate grade is given when there is doubt about a trainee’s clinical competence. In particular it is hoped that trainees will feel protected from the possibility of an idiosyncratic judgement being made about their clinical abilities. Of equal importance, it is hoped that supervisors will feel supported in the event of having to make a difficult decision. As soon as a supervisor becomes aware that their trainee may obtain an ‘unsatisfactory’ overall rating on the placement, they should inform the Clinical Tutor.
It would obviously be desirable if some indication of the supervisor’s degree of concern could be given at the mid-placement visit. However, if this is not possible, the supervisor should inform their trainee and the Clinical Tutor as soon as he or she becomes aware of doubts about the trainee’s competence. At that stage, the trainee should be clearly and specifically informed of what the supervisor’s concerns are and what he or she needs to do in order to make sufficient improvement to pass the placement. This information should then be written down and a copy given to the Clinical Tutor. If this occurs at the mid-placement visit, it can be recorded on the placement visit form by the Clinical Tutor.
The next stage occurs during the final week of the placement. Firstly, the supervisor and trainee should fill out the ‘Supervisor’s Assessment of Trainee Form’ without assigning an overall grade, and the ‘Trainee Evaluation of Placement form’ respectively. They should then meet to discuss these. This must happen prior to the Clinical Director’s involvement. The Clinical Director will then see the trainee and supervisor individually to discuss the assessments and will, together with the supervisor, decide what overall grade to assign to the trainee. This decision must be ratified by the examination board. The following step by step plan of action has been drawn up to clarify the procedure and to act as a quick reference guide.
- Supervisor contacts Clinical Tutor to discuss concerns.
- Supervisor informs trainee and together they make a plan of what the trainee needs to do to make sufficient improvement to be able to obtain a rating of ‘satisfactory’.
- Supervisor sends a copy of this plan to the Clinical Tutor.
- Both (2) and (3) can be done as part of the mid-placement visit.
- The Clinical Tutor arranges appointments for the supervisor and trainee to meet with the clinical director and clinical tutor at the end of the placement.
- During the final week of the placement, the supervisor completes the ‘Supervisor’s Assessment of Trainee Form’ without assigning an overall grade and the ‘Trainee Evaluation of Placement Form’.
- The supervisor and trainee meet to discuss these.
- The Clinical Director and Clinical Tutor meet the trainee, who should bring three completed copies of the ‘Trainee Evaluation of Placement form’ to that meeting.
- The Clinical Director and Clinical Tutor meet the supervisor, who should bring three completed copies of the ‘Supervisor’s Assessment of Trainee Form’ to the meeting.
- The Clinical Director, Clinical Tutor and supervisor decide on an appropriate grade to assign to the trainee.
- The Clinical Tutor, Clinical Director and supervisor then see the trainee to inform him/her of the assigned grade and the implications of this.
- The examination board will be involved in all cases of overall ‘unsatisfactory’ ratings.
Action to be Taken Following a Rating of Unsatisfactory Performance on Final Placement
If an overall rating of ‘unsatisfactory’ is awarded to a trainee at the end of their final placement, the clinical tutor in collaboration with the supervisor will specify skills to be demonstrated in order for the trainee to achieve a ‘satisfactory’ rating and specified further work will be determined by the examination board.
Dress Code
Please be aware there is a Faculty Advisory dress code for students whilst on placement. This can be found under the downloads section of the intranet and on the University website at http://documents.manchester.ac.uk/display.aspx?DocID=29038. Please ensure local Trust policies and guidance are also adhered to.
Assessment
PLEASE NOTE THAT THERE MAY BE TEMPORARY CHANGES TO ASSESSMENT PROCESSES AND PROCEDURES ON THE CLINPSYD AS A RESULT OF THE CORONAVIRUS PANDEMIC. STUDENTS SHOULD THEREFORE REGARD THE INFORMATION IN THIS SECTION AS “NORMAL PRACTICE” ON THE PROGRAMME BUT CONSULT THE SECTION ON CORONAVIRUS FOR THE MOST UP TO DATE INFORMATION ABOUT CHANGES TO ANY ASSESSMENT PROCEDURES.
Overall requirements of students
Summary of forms of assessment
Our assessment strategy is designed to ensure that graduates of the Manchester ClinPsyD meet the HCPC Standards of Proficiency and have demonstrated the competencies set out in the BPS Standards for the Accreditation of Doctoral Programmes in Clinical Psychology. In this way, we ensure that graduates are eligible for entry onto the HCPC register as Practitioner Psychologists and to be registered with the BPS as Chartered Clinical Psychologists.
The degree of ClinPsyD is awarded on the basis of the formal evaluation of: (a) academic work; (b) clinical practice; and (c) research practice. Trainees must pass all three aspects of the evaluation procedure in order to be awarded the degree. Programme work and examinations are marked and moderated anonymously as far as possible, with moderation over discrepant marks and formal evaluation by the lead External Examiner throughout the Programme. Trainees may be asked to defend any aspect of their work during oral examination.
The diagram below illustrates the relationship between core competencies, learning opportunities and approaches to assessment on the Manchester ClinPsyD.

At the end of the first and second years trainees must satisfy the Examination Board that they have achieved a satisfactory standard to continue to the next year of study. Candidates who fail to satisfy the Board that they have achieved satisfactory progress in any aspect of their training or conduct after the first or second year may, after consultation with the lead External Examiner, be disqualified from continuing the Programme.
Because the Doctorate in Clinical Psychology is an approved and accredited professional qualification as well as an academic degree, the University must be satisfied that graduates are fit for purpose and fit for award. In order to graduate, it is essential that students demonstrate safe, competent clinical practice. For this reason, irrespective of performance on academic assessments, students must reach the required standard of clinical work and will not be able to graduate from the programme if they have not done so.
While a student may fail one placement, in which case remedial action will be set out, students who fail two clinical placements will be deemed to have failed the programme. Details of this aspect of assessment are set out elsewhere in this handbook.
With respect to deadlines, for the sake of clarity we have a zero tolerance policy on late hand-ins for the submission of all academic assessments, including exams, case reports and placement assessment forms. The official hand-in time is 9am on the specified date; any pieces of coursework that are handed in late will automatically receive a fail mark. If you hand something in late and you believe there are mitigating circumstances in relation to this, you can apply for this to be taken into account.
The format of assessment is as follows:
- At the end of Year One, trainees must have passed two written examinations (Adult; Child), a Live Observation focusing on their ability to assess and manage clinical risk, which is completed alongside their adult placement in year 1. Their clinical competencies will also have been assessed on Placements 1 and 2. Trainees will ordinarily be asked to leave the Programme if they have not fulfilled the requirements at this stage.
- By the end of Year 2, trainees must have passed a further two written Case Reports (from Placements 2 and 3) and three additional written examinations (Clinical Neuropsychology; Older Adults; Learning Disability). Their clinical competencies will also have been assessed on Placements 3 and 4. Trainees will ordinarily be asked to leave the Programme if they have not fulfilled these requirements at this stage.
- In year 3, a further written Case Report from Placement 4 must be passed, and the Large Scale Research Project thesis is handed in.Their clinical competencies will also have been assessed on Placement 5.
- An Audit of Clinical Activity (ACA) must be passed during Year 1 or Year 2 of training, and a Service Related Project (SRP) in the final year of training, which is evaluated as part of Placement 5. There is a viva in July of Year 3 which primarily examines the thesis, but may cover any aspect of training, if required.
The section on academic dates provides information about what assessments will take place when.
How many fails are permitted?
Trainees are permitted to fail up to three academic assessments (i.e., case report, ACA or written examination) at the first attempt. Where an assessment has been failed at the first attempt, and assuming that the trainee has not already failed three other assessments, the trainee will be required to re-sit, re-submit or repeat that assessment. Resits of written examinations take place in August of the same year; the University charges a £75.00 fee for all resit examinations. If the trainee fails the piece of work at the second attempt then they will be deemed to have failed the Programme and will be disqualified from continuing further. In exceptional circumstances, and at the discretion of the Examination Board, a trainee who has failed a second attempt may be given an extraordinary oral examination. Only one such oral examination is permitted over the 3 years of study. A trainee who fails a fourth academic assessment on first attempt will be deemed to have failed the Programme.
On the first occasion of an overall rating of unsatisfactory on placement, this is equivalent to the fail of one academic assessment, and specific advice on progression will be given in these circumstances. Trainees who receive two overall unsatisfactory ratings on placements during the duration of their Programme will be deemed to have failed the Programme and will be disqualified from continuing further.
A diagram describing the actions to be taken in the event of failures of examinations or other assessed work can be found here.
It should be noted that mitigating circumstances must ordinarily be notified in advance using the forms and procedures set down by the University. The Programme’s policy is set out in the mitigating circumstances section of the handbook. Please read the guidance carefully, noting the kinds of circumstances for which mitigation can, and cannot, be given.
General Management of Professional Performance
Many aspects of trainee performance are evaluated using formal clinical and academic assessments (i.e., Supervisor assessments of clinical activity on placement, written examinations, case reports, Audit of Clinical Activity, Live Observation, Large Scale Research Project). More general aspects of performance management are informed by Greater Manchester West Mental Health NHS Foundation Trust’s Improving Performance Policy (IPP), which all trainees are subject to as employees of Greater Manchester Mental Health NHS Foundation Trust (GMMH). The IPP is available from the Trust intranet and should be read in conjunction with the ClinPsyD handbook.
The Improving Performance Policy is particularly relevant to the management of professional behaviour. Our standards and expectations in this regard are outlined in the ClinPsyD handbook (particularly the Professional Conduct, Ethics and Other Responsibilities of Trainees section), the Code of Professional Conduct and Fitness to Practise for Clinical Psychology Students that all trainee sign at the start of the programme, and more generally in the HCPC Standards of Conduct, Performance and Ethics and the BPS Code of Ethics and Conduct.
Trainee behaviours that might be considered examples of inadequate professional performance include (but are not limited to):
- unintentional but avoidable lateness for lectures or placement
- falling asleep in lectures
- an unacceptable attitude to patients and/or work colleagues
- writing unprofessional comments in lecture feedback
- minor, unintentional breaches of anonymity in case reports
- occasional failures to adhere to the departmental dress code in lectures or on placement
- other minor instances of unprofessional behaviour
- a lack of professional insight
- failure to recognise and/or acknowledge when personal circumstances (e.g., health problems, life events, social difficulties) are having a significant adverse impact on one’s performance
- failure to demonstrate the attitudes and behaviours described in the NHS Constitution or otherwise valued by the University and/or the employing Trust
- demonstrating attitudes or behaviours that go against the NHS Constitution or the values of the University and/or GMMH (but which are not obviously wilful)
- failure to check email communications from GMMH on a regular basis, particularly where this results in being locked out of your Trust IT account;
In cases where trainee performance has fallen below the required standard on an assessed piece of work we will follow the procedures and rules outlined in the Assessment section of the ClinPsyD handbook. In all other aspects of performance management our processes are informed by the IPP. The basic principles of this are:
- Very minor and brief/“one-off” transgressions should be dealt with in a common sense manner by a relevant staff member (e.g., lecturer, Clinical Tutor, Academic Advisor) and do not require explicit mention of the IPP or official recording.
- More significant, but still relatively minor and brief transgressions, should be dealt with at the earliest reasonable opportunity by the Clinical Tutor or another member of the Programme Team (e.g., Programme Director) as appropriate. This may be done as part of the staff member’s routine contact with the trainee (e.g., in a placement visit or other meeting), or in a dedicated meeting set up by the Tutor. This is considered equivalent to management supervision as described in the IPP and is an informal stage of performance management. In these cases, the Tutor should follow the process described in section 5.6 of the IPP. In brief, this consists of a discussion where the Tutor (providing clear evidence) makes the trainee aware of where their performance has fallen below the required standard and what should be done to rectify this in future. There should also be discussion about the likely causes of the performance issue and any potential mitigating circumstances, as well as whether the trainee has any additional support or training needs. Following the discussion, the Tutor should draw up a Performance Improvement Plan (see the IPP for further details) specifying the outcome of the discussion and the timescale and process for reviewing their performance.
- If the process outlined in the preceding point is unsuccessful in assisting the trainee to meet the targets set or achieve the required standard, the Tutor should (after seeking advice from Human Resources) follow the procedures outlined in Section 5.7 of the IPP in relation to Formal Stage One of performance management. This involves a formal meeting to consider the trainee’s performance, which would be chaired by the Programme Director and attended by the trainee, the Tutor, a representative from GMMH Human Resources and (if the trainee wishes it) a trades union representative or colleague to support them. After this meeting, a First Written Warning may be issued to the trainee specifying the nature of the problem, the actions needed to rectify the situation, and the frequency of subsequent review meetings, as well as details of any additional support, supervision or training required. In the event of a First Written Warning being issued, trainees will be advised that continued poor performance will ultimately lead to dismissal. Written Warnings remain in place for twelve months, during which time the required standards, once reached, should be maintained. The record or areas discussed at the meeting will normally be retained on the trainee’s file until the warning period had expired.
- If performance remains or falls below the required standard during the lifetime of a First Written Warning (or if a very serious concern or shortcoming becomes apparent for the first time) then the procedures described in section 5.7.3 of the IPP in relation to Formal Stage Two of performance management should be followed. This will involve a second formal meeting and may result in a Final Written Warning (or, in the case of trainees entering the policy at this stage, a First and Final Written Warning) being issued to the trainee.
- If performance remains or falls below the required standard during the lifetime of a Final Written Warning (or First and Final Written Warning) then the procedures outlined in section 5.7.4 of the IPP in relation to Stage 3 of performance management (Dismissal on Grounds of Capability). This may ultimately result in the trainee failing the ClinPsyD programme and their contract with GMMH being discontinued.
This policy does not cover issues of capability as a result of sickness; these should be addressed under the Trust Policy for the Management of Sickness Absence.
In considering whether to initiate a performance management process, the Tutor should consider whether it is better dealt with under the remit of the Trust’s Disciplinary Policy. If there is any uncertainty about this they should seek advice from the Programme Director in the first instance. In cases where there is evidence that poor performance exists as a result of wilful negligence and/or misconduct, the Trust’s Disciplinary Policy should always be used.
Annual Appraisals
At the end of Years 1 and 2, all trainees are required to meet with their Clinical Tutor and/or Academic Advisor for a formal Annual Appraisal meeting. Appraisals are an opportunity for trainees to reflect with their Tutor and Advisor about how their training is progressing, any areas of particular strength or difficulty, and how they can get the most out of their remaining time on the programme. The goal of the meeting is to identify a set of clear training objectives so that trainees know what to prioritise in the next year. During the appraisal meeting, all aspects of training (including their clinical, academic, research and professional development) will be discussed. Although the research supervisor is not present at the appraisal, they will be asked to provide a short report on their trainees’ progress for consideration at the meeting.
The appraisal meets required NHS recruitment and performance management policies and procedures (Knowledge and Skills Framework dimensions, KSF) and the KSF underpins discussions during the meeting. The meeting is an obligatory part of the programme, as well as preparation for the appraisal process that ClinPsyD graduates will follow if they are employed within the NHS after qualification. Trainees will be contacted during the summer about the date of their appraisal and will be expected to complete a preparation form in advance of the meeting.
Assessment of Clinical Competence on Placement and the Clinical Portfolio
Clinical competence is evaluated through (a) monitoring of clinical experience and reports from placement supervisors; and (b) four clinical Case Reports. Three of the Case Reports will be written and the fourth is a live observation designed to assess clinical risk assessment skills with an accompanying oral examination.
At the commencement of placement, the trainee and supervisor write a placement contract. This is drawn up with reference to core competencies set out by the HCPC and the BPS. The contract sets out a series of learning outcomes and is monitored by the Clinical Tutors.
Trainees are reviewed on placement by one of the Clinical Tutors at the mid point and again at the end of the placement. Through individual and joint meetings of the trainee, supervisor and Clinical Tutor, learning objectives are reviewed. Gaps are identified and set as learning objectives for future experience. The placement supervisor will have good, detailed knowledge about the student’s level of ability, and will have monitored their performance carefully throughout the placement. The Supervisors Assessment of Trainee (SAT) Form is completed by the clinical supervisor at the end of placement. This form lists a number of essential clinical skills, and trainees are rated on each. This assessment is an essential component and is regarded as the most effective way to evaluate clinical skills. The trainee should see the SAT form and have a chance to discuss it with the supervisor before he/she submits it. The trainee is also asked to provide a brief report on his or her experience of the placement.
The trainee also completes a Clinical Portfolio of experience, which they add to throughout the training (see below). This will be done via the Programme’s Personal Development Planning (PDP) system, accessible through the Programme intranet and visible to Clinical Tutors and Academic Advisors. Tutors will be asked to review trainee competencies throughout the training programme, including trainees’ progress towards competence in CBT plus at least one other of the core intervention models taught on the programme.
Trainees will be assessed on the extent to which they have achieved the learning outcomes set out for that placement and on their skills at the current stage of training. A rating of ‘unsatisfactory’ on one placement would be followed by advice from the Clinical Tutor and Supervisor about future work to be undertaken. Trainees who receive two overall unsatisfactory ratings on placements during the duration of their Programme will be deemed to have failed the Programme and will be disqualified from continuing further.
Case Reports are reports of clinical work which reflect knowledge of theory-practice links. Case Reports are marked anonymously, except for videos of clinical activity and case presentations where this is clearly not possible. Marking criteria include a rating of the student’s ability to critically appraise their own work. Students are also required to demonstrate their understanding of the importance of being able to maintain confidentiality, and of obtaining informed consent.
The categories of outcome for Case Reports are:
- Pass
- Pass with minor corrections
- Pass following anonymity corrections
- Fail
Where any sections are awarded a Fail, the examiners may award an overall rating of Pass with Minor Corrections or Fail. Pass with Minor Corrections is applied to cases where the examiners can see that only minor amendments are required to reach the pass standard and that these amendments could be completed within a 24-hour period. In this case, the overall mark is a pass, as long as the student completes the corrections in the allotted period. The fail mark is applied to work where substantial rewriting is deemed necessary.
Clinical Portfolios
Trainees are required to complete a clinical portfolio from each of their placements.
The trainee will be given access to an electronic Clinical Portfolio in which to record the experiences obtained (e.g., types of cases seen, tests used, treatment methods employed).
The Portfolio provides evidence of the work that has been completed on the placement and provides a means of demonstrating the experience gained and competencies developed over the course of the training programme. The clinical portfolio is completed by the trainee and submitted at the end of the placement, together with the Trainee Evaluation of Placement (TEP) form. However, it is recommended that trainees do not wait until the end of the placement before starting to complete the portfolio, as it should be easier to gather the evidence needed and add to the portfolio throughout the placement.
The Clinical Portfolio should contain information about all of the work completed on a placement, including assessments, formulations, interventions, supervision, consultation, teaching, meetings attended, contact with other professionals/ agencies, and any other work undertaken by the trainee. The portfolio should contain information about all of the people seen by the trainee for clinical work, including demographic information and information about complexity and risk. For each piece of client related work, trainees are required to state the primary psychological model that informed the work (e.g. PIT/relational, CBT, systemic, neuropsychological). If more than one model was used, trainees can list these as the secondary, tertiary etc. depending on the extent to which each contributed to the formulation. For intervention work, trainees must similarly indicate the primary psychological model that was used and within this, indicate the specific skills that have been used in each case. Over time, this will provide a useful overview of the experience gained through training and also enables trainees to highlight any gaps in their experience.
Once completed, the Clinical Portfolio must be seen and signed off by the supervisor as an accurate record of the work completed at the end of the placement. As well as containing information about individual placements, the portfolio will also summarise the overall training experiences and competencies gained on clinical placements.
It is important that trainees keep their Clinical Portfolio up to date and show it to their supervisor and to each new supervisor as they move to a new placement. In this way, any gaps in experience can be identified and remedied.
Written Examinations and the Assessment of Academic Knowledge
There are written examinations at the end of each block, which allow the Programme to assess key learning outcomes related to the acquisition of, and ability to apply, knowledge about theoretical models, clinical presentations and professional issues. A key part of this is assessing whether students have acquired Level 1 competences for the four main clinical approaches on the Programme .
Having unseen papers also requires students to read and revise widely, meaning that they have pedagogical value over and above their use as assessments. After each examination, trainees are encouraged to meet their Academic Advisor and feedback on their performance is discussed.
A sample of marked exam scripts are moderated anonymously by internal examiners and all marks are approved and ratified by the External Examiner at our Annual Exam Board Meeting in September. A pass, borderline pass or fail mark is awarded.
Trainees unable to attend an examination due to illness will be given a second opportunity as soon as feasible; this will be arranged on an individual basis. A re-sit of all papers is available in August of each year; the University will charge a £75.00 fee for all resit examinations.
The exam structure is as follows:
Year 1
March: Adult exam (Incorporating assessment of CBT and PIT knowledge and skills and professional issues)
June: Child exam (Incorporating assessment of CBT and systemic therapy knowledge and skills and professional issues)
Year 2
June: Older Adults exam; Learning Disabilities exam; Clinical Neuropsychology exam
All exams are based on an extended vignette and candidates are required to answer a number of standardised questions for each paper. Please see Canvas for exam guidelines, example vignettes and the standardised questions for each paper. Marking checklists are also available for the trainees on Canvas.
Case Reports
What are Case Reports and How Many are Required?
What are Case Reports?
Case Reports are reports of clinical activity and enable trainees to describe the breadth and quality of their practice. Four Case Reports need to be submitted, one from each of the first four core placements, and passed successfully to obtain the ClinPsyD.
Three of the case reports (from placements 2, 3 and 4) are fully written, and one is a Assessment of a Live Observation. Please see the relevant section in the handbook.
One of the four case reports should be written using a Cognitive Behavioural formulation and intervention. This CBT case report counts towards the acquisition of the CBT competences as outlined in the Competency Framework section. To be classified as a CBT report, any evidence-based cognitive or behavioural approach to formulation and intervention may be used as long as it can be justified as belonging under the CBT umbrella. This includes approaches within all of the so-called first, second and third “waves” of CBT, and therefore includes most behavioural approaches, “traditional” CBT (e.g., Beck, Ellis) and approaches such as Metacognitive Therapy, Acceptance and Commitment Therapy, Dialectical Behaviour Therapy, Compassion Focused Therapy and Schema Focused Therapy. If a trainee is in doubt about whether a piece of work is appropriate to be classified as a piece of CBT work, the clinical or academic tutor will be able to advise.
For the other two Case Reports, trainees are required to submit at least one assessment report. Case Reports are only completed on core placements and are not required for Year 3 placements.
Case reports should be representative of some fairly substantial piece of work that the trainee has done and demonstrate the trainee’s competence as a clinical psychologist. They are reports of clinical work which reflect knowledge of theory-practice links, and can cover any activity that falls within the broad scope of a clinician’s work. The work will often be that of individual assessment and/or therapy but could be clinical activity with patient or staff groups. A written Case Report must be submitted at the end of placements 2, 3 and 4.
The content of the Year 1 teaching session on Case Reports will include a brief overview of information that ensures that students are clear about both the rights and needs of service users and good practice in gaining informed consent from service users for writing up case reports. A second teaching session on Case Reports is scheduled later on in Year 1. This is an opportunity for trainees to ask more specific questions about their own case report write up and obtain feedback from the Clinical Tutors.
Written Case Reports are marked anonymously. Full details are provided elsewhere of Case Report 1 (Live Observation), which comprises of a role play designed to assess trainees’ ability to assess risk.
Case Reports and client consent
We encourage all trainees to seek consent from clients to write up the work as a Case Report. The main reason for this is that we do not want to place additional limits on what can be submitted as a Case Report, as this may compromise a full and fair academic assessment process; we believe this is acceptable as the documents are not in the public domain and the content is fully anonymised.
How Many Case Reports are Required and When?
Each of the four Case Reports must be submitted by the deadline dates specified in the Programme Calendar. Exact deadline dates are set out at the start of each academic year.
Broadly, the timing for submission of Case Reports 1-4 is as below:
| Submitted | |
|---|---|
| Case Report 1 (Live Observation) | February |
| Case Report 2 ( Written) | October |
| Case Report 3 (Written) | April |
| Case Report 4 (Written) | October |
Submission of Case Reports
A copy of the case report (including the case report cover sheet, which can be downloaded from the intranet) must be emailed to Megan Brown by 9am on the day of the deadline. This should be password protected using the standard format. Information regarding this format will be sent direct to trainees. If submitting multiple documents, trainees should zip these into a folder and password protect the folder. The validation form should be submitted separately via email and not attached to the case report or appendices as this contains the trainee name and will be saved separately.
Usually mitigating circumstances are submitted two weeks in advance of a deadline however, if you hand something in late and you believe there are mitigating circumstances in relation to this, you can apply for this to be taken into account.
There are a number of examples of case reports (with marks and feedback included) from previous years, in the ClinPsyD Administrative Office. Trainees are encouraged to look through a selection of these reports as a guide to content and style.
Content of Written Case Reports
The marking sheet used by examiners is available for trainees to view on the intranet (see intranet) and should be read in conjunction with this material.
Written Case Reports should enable the marker to have a clear idea of the reason for referral and of the way in which it was tackled. Markers will be looking for a systematic approach to the problem, which integrates theory with practice and addresses the issue of outcome. Markers will attach particular importance to the application of psychological knowledge in the formulation of the problem and the candidate’s demonstrated ability to evaluate clinical work critically and to learn from it.
It is common for trainees to complete pieces of clinical work jointly with their supervisor, especially where the work might be considered more complex than in a case that they would otherwise see individually. It is possible to write up this work as a case report, as long as the Trainee has completed a significant proportion of the work him or herself and has been closely involved in the process of developing a formulation and plan for intervention. It is also important to specify the role of the Trainee in the work and to place an emphasis on reporting these aspects of the case.
One of the three written case reports should describe a piece of clinical case work where a Cognitive Behavioural formulation and intervention was used.
All reports should include examples where clinical decision making has been used in your work, for example the decision around suitability for psychological input, the decision about which approach to use, the decision about the number of sessions offered.
Word limits
Written reports should be between 2,500 and 4,000 words, excluding ancillary sections. This means that the title page, list of contents, references and appendices are not counted. The rest of the report including the diagrammatic formulation and any tables or diagrams are included.
All Case Reports should be submitted with the word count indicated on the cover sheet. All word counts should be calculated using Microsoft Word 2010. To check the word count using this please click on the ‘words’ tab at the bottom of the document, next to the page numbering. Trainees need to click on ‘word count’ and a pop up box will appear and the ‘include textboxes, footnotes and endnotes’ check box needs to be ticked. Please note, no JPEG or PDF files are to be included in pieces of work as these are not counted by the word count. However, if tables and diagrams are not being included in the word count they should be counted manually and added to the word count if necessary. It is the trainee’s responsibility to ensure that all text is being counted.
Reports that are over the word count will be returned to the trainee, who will be required to amend them so that they are within the word count limit; the normal submission deadline still applies in these cases, so trainees should ensure that they allow themselves enough time to check their work prior to submission. Any attempt to disguise the actual number of words in the report (e.g., by placing words in ‘invisible’ text boxes, presenting text as images, introducing ‘invisible’ hyphens between words) will be regarded as a form of academic malpractice and will be dealt with accordingly. We do check reports to ensure that trainees are not engaging in such practices!
What Should an Intervention Case Report Include?
Intervention reports should outline a piece of work where assessment, formulation and intervention work has taken place. The report of clinical activity should be structured using the following guidance. Variations to this structure are acceptable but you should present your work in a coherent way which takes into account the content of the sections below.
Assessment
It is appropriate to report here about how and/or why the problem came to the trainee or their supervisor and any initial thoughts/hypotheses that guided the subsequent assessment process. The report should then describe the initial assessment which might include information from interviews, case notes, meetings, telephone calls, psychometric measures, observation or daily diaries. Such assessment should form the basis for subsequent action including assessment of outcome. The reasons for selecting particular instruments/processes should be included. For all clinical reports it is helpful to include a statement about confidentiality and consent, and also where and how often the client was seen.
Formulation
The report should contain an initial formulation which consists of a brief statement and diagrammatic representation about how the problem was understood after the assessment phase. Such an initial formulation could be wrong but should lead coherently to the initial interventions. Note that separate formulations may be required for the aetiology and maintenance of the problem. Account should be taken, either here or elsewhere in the report, of social context including race, class, gender issues. You should include the hypotheses that you planned to test out in therapy. Both diagrammatic and written formulations should be consistent with each other and not contain any new information that has not already been presented in the assessment section.
Action plan and Goals
This plan should follow logically from the assessment, formulation and hypotheses and include measurable goals. This action plan might involve further detailed assessment and/or outline of therapeutic intervention, and/or proposals for service development, and/or outline of teaching programme. Where relevant it should refer to the professional and ethical issues raised. Goals should be from the client and the trainee perspective and be clearly operationalised.
Intervention
The report needs to describe how the action plan was implemented and the treatment process. Although not a verbatim account, this should provide enough detail and/or examples to enable the examiners to have a clear picture of which procedures were adopted. It is important to demonstrate the link between theory and practice in this section and relate procedures to established research findings.
Outcome
This is a description of what was achieved. This might include accounts and/or measures of change in psychological functioning, skills, settings, management practice or effectiveness of training programmes. It is important here to refer back to the goals identified previously. Follow-up details should be described in this section as well as any reformulation that might be required. Tables and graphs may be included if appropriate.
Critical Evaluation
Here you should provide a critical review of the case, discussing the relationship of the original formulation to the subsequent clinical work. Reference to relevant literature should be made. Reflection upon professional issues raised may be appropriate, as may the discussion of the relationship between the therapist and client, what has been learned and how supervision was used.
Social Context
The report should demonstrate the impact that the social environment has on the psychological problem and the therapy. Ideally this should be integrated throughout the report. Examples include:
- any causal factors e.g. social isolation
- any maintaining factors e.g. family, cultural beliefs, lack of support
- impact upon psychological intervention e.g. therapist/client age, gender or financial influences.
See also the notes below on making reference to social and cultural aspects of the case.
Integration of theory and practice
The report should contain references to relevant theoretical work and research to identify its basis in psychological knowledge. This should be integrated into the report as a whole and work should be cited as appropriate.
References and Appendices
A complete list of references should be contained in a separate section at the end of the report and before any appendices. References should follow a standard format (American Psychiatric Association; see APA reference style guide on the intranet). Each report of clinical activity should include, as appendices, copies of anonymised but original referral letters and official reports written by the candidate as well as copies of completed monitoring forms, diaries and rating forms. It should be noted that report writing, a professional communication skill, will also be assessed.
What Should an Assessment Case Report Include?
These guidelines encompass neuropsychological and other forms of formal assessment and it is intended that they inform the planning and writing of assessment case reports in general clinical work. They should not be taken be as constituting a set framework for writing assessment case reports, but are intended to steer you towards good practice both during and after training. They are written primarily, but not exclusively, to compliment the teaching in the areas of learning disability, neuropsychology, older adults and children.
An assessment case report will not usually contain information about an intervention and its outcome. The requirements pertaining to case reports in general, e.g., word limit, references etc. all also apply to this type of report.
Referral details and background to assessment
Questions that should be considered at this stage are:
- Is the referral appropriate?
- Why has it is come to clinical psychology?
- What does the referrer hope to get from a psychological assessment?
- Is the referral feasible?
You should consider the person’s presentation and history, together with other factors that might be relevant so as to develop provisional hypotheses that your assessment will then examine. If the referral is a ‘routine assessment’ (e.g. memory clinic, IQ testing, etc.), then you should think carefully about whether it is an appropriate case to write up for your assessment case report, which should demonstrate your ability to undertake complex idiosyncratic clinical assessment work.
Assessment
You should describe the assessment work as it was carried out and should refer to both formal and informal assessment as appropriate. The assessment reported should relate to what is being assessed. This may sound obvious, but if you state that you will be assessing, for example, sleep disturbance, then appropriate methods should be used and the data should be analysed and reported in the appropriate manner.
Although standardised formal assessments can be a useful short-cut in carrying out the assessment, the following sources of information and clinical data are equally valid and important:
- History
- Self-report
- Objective measures (e.g. actigraphy, GSR, heart rate, etc.)
- Direct observation
- Third party reports
- Idiographic measures (e.g. repertory grids, personal questionnaires, Q-sort, etc.)
Always bear in mind that the formal assessment is only one part of the wider psychological assessment and your account should not lose sight of the individual , their relationships, social context, stage of life factors; in short, the psychology. Such factors should inform your formulation as they will relate to the individual’s response to their cognitive difficulties and will partly determine the choice and feasibility of your recommendations. Remember that the quality of the therapeutic relationship is as important, and can be as informative, as any other aspect of the assessment.
Results
When reporting results, the minimum requirement is that you report the overall results of all of the formal assessment measures utilised. However, this information does not have to be reported in the main body of the text as long as there is sufficient to illustrate the extent or range of the problem or impairment under consideration. A full data set should be in the appendices (including confidence intervals, standard errors, significance levels, etc. if relevant), but if the reader has to refer to the appendix to make sense of the assessment, you have not included enough information in the main body of the report. Therefore, it can be useful to present data in tables, but this should not take the place of a written description of your findings. As per the diagrammatic version of your formulation, tables are a useful adjunct not an alternative to your description. Qualitative information regarding a person’s performance on formal assessment procedures should also be reported. Do not infer what you think the person’s thoughts might be in order to make these fit a particular model or hypothesis.
The data thus presented, in table or text, should be “translated” so that the reader is able to understand the extent of the person’s difficulties in relationship to normal or non-pathological functioning, for example by making use of verbal descriptions of the specific problems: “ this meant that X had difficulty in doing Y and Z”. This might involve age-matched norms and reporting centile scores or by reference to baseline data or clinical cut-offs. The use of non-specific composite scores such as IQ or non-scientific statistical constructs such as ‘mental age’ should be avoided whenever possible. If perforce you have to use the WAIS or any of the other Wechsler test batteries, results should be reported in terms of cognitive strengths and weaknesses, linked to specific neuropsychological processes and real-life situations, rather than using aggregate scores (e.g. FSIQ/VIQ/PIQ/NVIQ, etc) or the WIS “index scores”, which have little if any relationship to neuropsychological processes and actual functioning. The same applies if you have to use a set battery of assessments rather than tailor your assessment to the person’s specific difficulties and needs.
Formulation
A formulation in an assessment case report must be derived from the assessment work carried out and therefore should be specific to the individual case. The formulation should be presented in diagrammatic form as well as being described in the text. A simple Carr-style list of factors pertaining to the case is unlikely to be regarded as an adequate formulation, unless it was the actual focus of the assessment.
Recommendations
The recommendations in an assessment case report essentially take the place of the action plan and goals in an intervention case report. As such they are subject to most of the same considerations, including being:
- derived from the formulation
- practical and capable of being implemented
- operationalised (give examples) and, if possible, part of an on-going care plan
- capable of being assessed and measured and
- unique to the case and reflexive in light of future developments
A useful test is to ask whether the recommendations could have been generated without actually carrying out the assessment and/or whether they could have been derived from general guidelines for a particular clinical population. If the latter is found to apply, then the recommendations should be revised so that they are specific to the case in question and follow from the individual assessment and formulation.
Critical evaluation & reflection
Critical evaluation of the work undertaken is an essential part of any case report. You may reflect on the appropriateness of the assessment, the suitability of your formulation, your hypotheses, the measures you used etc. It is in this section that you critique your decisions and explain any omissions. If, for example, there is something that you would do very differently in retrospect, the work will not be penalised as long as you demonstrate that you have reflected on the decision(s) and given an account of your reasoning at the time.
This is also the section where you may wish to consider personal issues (for example, your experience of the therapeutic relationship, how you made use of supervision), professional issues (for example, informed consent, issues of confidentiality, working with complex systems, issues of risk / safety etc.), and service related issues (for example, impact of waiting lists, staff turnover etc.).
Integration of theory and practice
A common omission in assessment case reports is any reference to research work and research findings. Such reference is as important as in intervention case reports and is an essential part of any formulation. With regard to assessment case reports, the following should be considered:
- Neuropsychological research: it is acknowledged that in areas such as learning disabilities, there is much less research and theory to draw upon and that such areas are largely ignored in many standard neuropsychological texts. However, this should not be a barrier to developing appropriate formulations for people with learning disabilities that draw upon “standard” neuropsychological concepts such as memory, attention, executive functioning, etc.
- Cohort psychology: a report describing the neuropsychology of suspected dementia, for example, should be embedded in old age psychology, issues of aging pertinent to the client, literature on loss, cultural and social factors – remember, older adults might not know who Catherine Tate and Simon Pegg are, but do you know who Rob Wilton and Frank Randall were?
- Syndromes: it is important to be aware of work that has investigated the distinct neuropsychological profiles of specific syndromes, such as Prader-Willi, autism and Korsakoff syndrome.
Social context
You must be aware that issues such as ethnic origin and identity are not ‘bolt on’ factors in an assessment and that even in the presence of major cognitive impairment, a person’s cognition and action have a large social and cultural component. Moreover, psychological assessment is not a neutral process. Therefore the interaction between assessor and assessed should always be considered, as this relationship may involve explicit and implicit elements of inequality and coercion, particularly with minority and/or vulnerable groups of people.
See notes on Social and cultural aspects of case reports below.
References & appendices
Appendices should include copies of anonymous but original reports/letters written as part of the assessment, anonymous but original referral letters, copies of completed monitoring forms, diaries and rating forms (only one of each is required), copies of all completed psychometric assessment forms (in the case of neuropsychological assessments). It should be noted that report writing, a professional communication skill, is being assessed.
How do I Make Reference to Social and Cultural Aspects of the Case?
These brief notes have been written with the aim of helping trainees to fully incorporate the relevant social and cultural factors into the account of their work.
Obviously, it is hoped that social and cultural factors will have been considered throughout the assessment, formulation and intervention stages of the piece of work that is being documented and not solely considered in relation to the case report. The following factors are therefore intended to illustrate the depth, breadth and importance of such issues. It is not the intention that the headings below should appear in case reports, but that such factors should be considered in the main formulation and incorporated throughout where appropriate.
Please also bear in mind the John Burnham mnemonic SOCIAL GRRAACCEESS which has been discussed in teaching and further information can be found in this article;
Learning as a context for differences and differences as a context for learning John Burnham, Diane Alvis Palmab and Lisa Whitehouse; Journal of Family Therapy (2008) 30: 529–542
Causal factors with respect to clients’ difficulties
- Unemployment
- Material deprivation
- Ethnicity
- Gender
- Care of young/elderly relatives
- Social isolation
- Work environment and practices
- Poverty related physicalillness
Maintaining factors with respect to clients’ difficulties
- Family beliefs
- Cultural beliefs
- Secondary gains (e.g. financial benefits, social contact, avoidance)
- Lack of appropriate formal services
- Lack of informal support
- Personal/familial finances
Influences on appropriateness and effectiveness of psychological intervention
- Personal economic and financial factors
- Individual beliefs
- Cultural beliefs
- Structural e.g. benefit systems, local and national policies, service structures
- Physical environment
- Gender of therapist
- Class background of therapist
- Age of therapist
Effects of psychological difficulties on other aspects of clients’ life
Effects related to:
|
Impacting on:
|
Live Observation Assessment
Requirements of Live Observation
Overview
The evaluation will be in two parts, a mock clinical session involving an assessment of risk (lasting 20 minutes), followed by answering a set of standard questions (20 minutes). The former part will allow an in vivo look at trainees’ assessment, interpersonal, risk assessment and management skills. The latter part will provide an opportunity to assess trainees’ thoughts about the case and their plans for further action regarding risk management for this client. A member of the programme team, and a member of the Community Liaison Group (CLG) will sit in during both parts and mark the assignment ‘live’. Both parts will also be recorded by video camera (operated by the staff member) for moderation purposes.
For the 2020 intake, the Live Observation role play and examination will be carried out via Zoom.
The Live Observation scenario content will be linked to the trainees’ core adult placement.
Clinical session: The client will be played by an actor. It will be assumed that this is the first appointment the trainee has with the client and that the usual discussions around consent, confidentiality, and the nature of the sessions have been covered.
Trainees will be instructed to open the session with a standard question “Many thanks for coming along to the session today, could you please start by telling me a little about some of the difficulties you’ve been having”. Trainees will be allowed to adjust the wording.
The actors would then have a standard opening statement which would hint at the presence of risk. The risk assessment would follow from this point.
Trainees will be given the following guidance:
- Identify and assess the key areas of risk present for this client
- In assessing risk, consider the following:
- The form and nature of the risk
- The overall level of risk
- The imminence of the risk
- Factors (personal and contextual) which moderate (enhance/reduce) the level of risk
- Collaboratively generate an initial plan with the client for how this risk(s) will be managed.
- Maintain a warm and empathic therapeutic stance
Trainees are not expected to generate a full risk management plan within the space of the simulated risk-assessment, but will be expected to begin the process of collaboratively planning a way of managing identified risks with the client.
All scenarios will contain at least two distinct forms of risk.
Actors will be provided with the standard starting script, and an additional character sketch of the client they are playing, including the specific details of the areas of risk they are experiencing. The sketch will also cover: presenting problems, interpersonal style (e.g., avoidant, hostile, etc.), and contextual information (e.g. living situation).
Post-session Questions: Upon completion of the clinical scenario trainees will have a short 10 minute break (taking place in a breakout room) to reflect on the session, plan what they might do next, and make notes. The markers will then bring the trainee back into the main room on Zoom and the trainee will be given 20 minutes to answer the following questions, which will be asked by the markers:
- Please briefly summarise the main areas of risk, the nature, form and severity of this risk.
- Detail a brief plan of how you would respond to and manage this risk(s). Within this plan, consider actions you would take, both within the session itself, and following the session. This may include outlining actions you had already started to implement during the simulated session with the actor.
- (asked by the member of the CLG): How well do you think you engaged with this person whilst discussing a potentially difficult area of their life?
Objectives
- To demonstrate competence in clinical risk assessment
- Demonstrate knowledge of potential areas of risk (to others, to self, environmental, safe-guarding, etc.)
- To demonstrate an ability to appropriately assess the presence of risk in these areas
- To demonstrate an ability to gain adequate information to determine an overall level of risk, its imminence, form and character.
- To demonstrate an ability to reflect upon how psychological and contextual factors may contribute to risk and to make plausible hypotheses concerning these relationships.
- To demonstrate an ability to collaboratively problem-solve with a client about ways of managing risk.
- To demonstrate an ability to generate an appropriate plan, both in the short and long-term, for managing identified risks.
- To demonstrate an ability to discuss and assess risk, in an interpersonally sensitive and appropriate manner, which supports the therapeutic relationship
Procedure
The evaluation will run across two days. This means approximately fifteen trainees will complete the assessment on each day. A different scenario will be used for the first and second day to ensure trainees allocated to the second day do not have an unfair advantage.
All trainees will be asked not to discuss the assessment with their peers until the end of the day, to ensure that those trainees who complete the assessment later in the day do not have an unfair advantage. It will be made clear that sharing the details of the scenario to another trainee due to be assessed that day, in a fashion that would potentially aid the latter trainee’s performance, will be seen as a professional issue.
The sessions would take place in two basement break-out rooms in the Zochonis building. Two sessions will be run in parallel, with a total of 15 trainees per day. A different actor would be in place for each of the two parallel streams, doing the full day. As above this will be done via Zoom for the 2020 intake.
At the start of the day an hour has been set aside to set up the rooms and filming equipment and also to ensure standardisation of the actors. The latter process will involve an opportunity for actors to ask staff any questions about the characters in the vignette and to pilot the scenario with one another to ensure consistency across the parallel streams.
Marking Guidelines
One staff member will provide marking and feedback on each trainee’s performance. A member of the CLG will also be present. They will complete a separate CLG marking form, which will be formative only, and also inform the marking by the staff member. The video recordings will be provided to the staff member. Marking will be done in a similar way to the existing case reports, with a marking form used that covers a series of key competencies. The marker will assign a mark based on the skills viewed in the role play and the feedback to camera. The areas being assessed will be:
Effective information gathering
- An ability to elicit information regarding nature and severity of risk.
- An ability to elicit information regarding the context within risk occurs, including triggers, maintaining factors and moderators of risk.
- Appropriate use of prompts and follow-up questions to gain the required information.
- An ability to structure assessment in a coherent and logical manner.
Appropriate summary of risk
-
- An ability to correctly identify the main forms of risk.
- An ability to accurately evaluate the severity of risk, its imminence, form and character
- An ability to identify relevant triggers, maintaining factors and moderators of risk.
- An ability to reflect upon how psychological and contextual factors may contribute to risk, and to make plausible hypotheses concerning these relationships.
Appropriate interpersonal style
- Collaborative approach to assessment is taken
- While maintaining professional boundaries, an ability to show appropriate levels of warmth, concern, confidence and genuineness, matched to client need
- An ability to engender trust.
- An ability to develop rapport.
- An ability to convey an appropriate level of confidence and competence.
- An ability to avoid negative interpersonal behaviour (such as impatience, aloofness or insincerity).
- An ability to listen to the client’s concerns in a manner which is non-judgmental, supportive and sensitive and which conveys a comfortable attitude when the client describes their experience.
Development of plan for management of risk
- An ability to formulate a basic plan for appropriately managing and mitigating risk, that matches the nature of the risk identified
- An ability to consider both immediate and longer term actions within the plan
- An ability to consider appropriate use of information sharing, balancing the needs of the client
- An ability to consider the collaborative involvement of the client in future actions.
Consideration of social, cultural and contextual factors?
- An ability to identify and ask about relevant social, cultural, systemic or contextual factors related to risk
- An ability to reflect upon these factors in summarising the nature of the risk
- An ability to consider these wider factors where relevant, in considering a plan for mitigating risk.
- An ability to adapt the assessment so as to match the client’s needs in terms of factors such as age, education, social and cultural background, etc.
Each of the five competences assessed will be awarded pass, borderline pass or fail, according to the following criteria:
Pass – The trainee has demonstrated skills in this area to the level expected for this stage of training.
Borderline Pass – The trainee largely performs at the expected standard but is falling short on some key areas.
Fail – The trainee does not meet the necessary standard in most areas or there is the presence of serious problematic behaviours or responses in one area.
Written feedback will be provided outlining what the trainees did well and what they could improve upon.
Marks will be based on trainees’ overall performance, encompassing both sessions and further thoughts recorded on camera. However, some sections of the marking form differentially weight the role play or the response to the examiners questions. To get a straight pass an adequate level of performance will be required across both parts of the assessment.
A sample will then be moderated by a member of the programme team and sent to the external examiner for consideration.
An overall mark will be given of pass, pass with minor corrections or fail. If any of the individual sections are awarded a fail, the examiner may award an overall rating of either pass with minor corrections or fail. The former is applied to cases where the marker can see that only minor problems are identified and that amendments can be made within a two-week period, as outlined below. A fail is applied to work where there are significant problems identified. Where a trainee preforms at the expected standard on all but one section, but there are major concerns about this component of the assessment (e.g. very inappropriate interpersonal style) a fail mark may still be given.
Pass with Minor Corrections
If the Live Observation is awarded pass with minor corrections, the trainee will be sent a resubmission requirements form. This will outline the areas of concern and prompt the trainee to reflect on the work submitted. Trainees are required to submit a piece of written work, demonstrating: (1) their reflection on the original Live Observation performance; and (2) a description of what the trainee would do differently in future, in order to address the issues raised by the examiner. This may include, for example, different questions that may have been asked by the trainee in the session, ways in which the session could have been structured differently, knowledge/ theory that the trainee could have drawn on and would do so in future, etc. Trainees will have two weeks from the collection of the resubmission requirements form to complete this work. A maximum of 1000 words are allowed. Following a PWMC mark a trainee will have a maximum of two attempts at resubmission. If the second resubmission is not up to standard the piece of work will be awarded a fail.
Fail
If the video submission is awarded fail, the trainee will be required to pass a second Live Observation during the next placement (placement 3). The new Live Observation may be awarded a pass, pass with minor corrections or fail. If a PWMC is given, the trainee has a maximum of two attempts at further submission using the PWMC guidance above. If a second Fail mark is given, the trainee will be required to exit the programme.
Assessment of Written Case Reports
Written Case Reports are assessed “blind” by one member of the programme team. This means that the assessor does not know who the trainee is. A selection of the marks for submitted case reports are then reviewed by a member of the programme who was not involved in the marking process. This person – known as the moderator – is able to oversee the marking process and reviews all reports that have received a fail or pass with minor corrections award and a selection of passes. They are able to assess whether the range of marks have been fairly awarded and if there are any major discrepancies between marks.
Within this process the moderator may choose to discuss the assessment of a case report with an individual marker in order to seek clarification. The moderator may also recommend that the marker makes changes to the assessment.
In the rare circumstance when agreement about this cannot be reached the Case Report is allocated to a second marker, a member of the programme team who has not been involved in the assessment of this case report. The second marker is unaware of the initial mark awarded and the content of the discussion between the marker and moderator. The assessment of the second marker stands as the final mark awarded.
The sample of case reports and marks overseen by the moderator are then sent to the External Examiner for approval. The moderator also includes written copies of any discussions between the marker and moderator, where discrepancies have occurred. The marks are then communicated to trainees. The External Examiner’s views about the consistency and validity of the marks are sought and ratified at the Exam Board meeting in September.
Case reports are assessed using the criteria outlined in the rating forms that are available on the intranet. Each section of the report is awarded Pass (P), Borderline Pass (BP) or Fail (F) and assigned an overall judgement of Pass, Pass with Minor Corrections or Fail. In the event that the Case Report contains any breaches of anonymity or confidentiality, the report will be awarded, as a maximum, a grade of Pass following Anonymity Corrections and returned to the trainee who will be required to rectify the anonymity breaches. Only once the anonymity breaches have been corrected to the satisfaction of the marker can the mark be formally recorded as a Pass.
If any of the sections are awarded a Fail, the marker may award an overall rating of either Pass with Minor Corrections or Fail. The former is applied to cases where the marker can see that only minor amendments are required to reach the pass standard and that these amendments could be completed within a 24 hour period. A Fail is applied to work where substantial rewriting is deemed to be required. In addition to the ratings, trainees will receive written feedback from the marker for all reports. In the event of Pass with Minor Corrections and Fail, the trainee will receive the marker’s comments and a resubmission requirements form outlining the necessary amendments to ensure that the report reaches the appropriate standard (see here for further information).
Resubmission of Case Reports
Resubmission of Written Case Reports
In the event of a Pass with Minor Corrections
If a case report is awarded Pass with Minor Corrections the trainee will be sent a PwMC Requirements Form. This will outline, along with the assessment feedback provided by the marker, the shortcomings identified and the revisions required to amend the piece of work to meet the appropriate standard. Trainees will have one week from publication of results to return reports that have been awarded a ‘Pass with Minor Corrections’. Up to 200 words are allowed in the corrected report for any additional information that is required. Trainees are allowed two attempts to make the necessary corrections; if these are not completed to the required standard by the second attempt then the piece of work will be deemed to have failed.
In the event of a Fail
If a case report is failed on examination, the trainee will be sent a Resubmission Requirements Form, outlining the shortcomings of the piece of work and noting the requirements for resubmission. The trainee is invited to meet with his or her academic advisor to discuss the feedback. Up to 200 words are allowed in the resubmitted report for any additional information that is required. All other changes need to be accommodated within the original 4000 word limit by revising the existing material.
It is likely that a trainee will resubmit a case report based on the same material as the original and amended in the light of the feedback. It is possible, however, following discussion with the tutor, for a trainee to resubmit entirely new clinical material. If this course of action is followed, the trainee will not be entitled to feedback on the new version as a whole although some general feedback, in line with the weaknesses identified in the failed case report, is permissible. Trainees will have four weeks from publication of results to resubmit a failed piece of work or alternative report.
The resubmitted piece of work (either from a new report or the original report) can be awarded a Fail, a Pass or a Pass with Minor Corrections. If a PWMC is given, as above, trainees are allowed two attempts to make the necessary corrections; if these are not completed to the required standard by the second attempt then the resubmission will be deemed to have failed.
Resubmission for Live Observation
Pass with Minor Corrections
If the Live Observation is awarded Pass with Minor Corrections, the trainee will be sent a Resubmission Requirements Form. This will outline the areas of concern and prompt the trainee to reflect on the work submitted. Trainees are required to submit a piece of written work, demonstrating: (1) their reflection on the original work, explaining what they have learned from the work shown in the Live Observation and from the examiners feedback; and (2) a description of what the trainee would do differently in future, in order to address the issues raised by the examiner. This may include, for example, different questions that may have been asked by the trainee in the session, ways in which the session could have been structured differently, knowledge/ theory that the trainee could have drawn on and would do so in future, etc. Trainees will have two weeks from the publication of results to complete this work. A maximum of 1000 words are allowed. Following a PWMC mark a trainee will have a maximum of two attempts at resubmission. If the second resubmission is not up to standard the piece of work will be awarded a fail.
Fail
If the Live Observation is awarded a Fail, the trainee will be required to undertake an additional Live Observation . The new submission may be awarded a pass, pass with minor corrections or fail. If a PWMC is given, the trainee has a maximum of two attempts at further submission using the PWMC guidance above. If the resubmitted piece of work receives a further Fail then the trainee will be deemed to have failed the Programme.
Retention of Marked Work
Assessed work will be retained until twelve months after your completion of the Programme. An anonymous sample of Case Reports, with feedback, is provided for future trainees to use as a guide.
Case Report Deadlines and Extensions
Deadlines
A copy of the case report (including the case report cover sheet, which can be downloaded from Canvas) must be emailed to Megan Brown by 9am on the day of the deadline. This should be password protected using the standard format. Information regarding this format will be sent direct to trainees. If submitting multiple documents, trainees should zip these into a folder and password protect the folder.
Reports that are found to be too far under (i.e. less than 2500 words), or over the word limit, will be returned and must be represented (within the word limit) within two working days of the original submission date.
Any pieces of coursework that are handed in late will automatically receive a fail mark. Usually mitigating circumstances are submitted two weeks in advance of a deadline however if you hand something in late and you believe there are mitigating circumstances in relation to this, you can apply for this to be taken into account. The report will still be marked as normal and the marker will be unaware of the fail for late submission. If the late piece of work is awarded a Fail mark in relation to its content, trainees will be required to make the required corrections so that it meets the necessary standards.
Requesting an extension
If for reasons beyond your control, you are not able to meet a deadline, you should request an extension by discussing the situation with your Clinical Tutor. After this discussion, if it is agreed that it is appropriate for you to receive an extension you should submit an extension form to the clinical directors (Lara Bennet and Claire Fothergill) via the admin team at least two weeks in advance of the relevant deadline. This request should be made using the extension application form (see Canvas for form). The clinical director, in liaison with your Clinical Tutor, will then decide whether an extension of the deadline is appropriate. Competing deadlines will NOT be considered as suitable grounds for an extension request to be granted.
Case Reports: Some Frequently Asked Questions
Do I need to Adhere to a Set Style?
Whilst the programme does not insist on a predetermined layout, certain features should be present. These are outlined in the “Guide to the Presentation of Case Reports” (see intranet). Trainees are strongly advised to use this guide as a checklist prior to submission. It is derived from simple recurring errors and using it should prove very helpful. At a practical level, it is also helpful to present the report in a format that allows the marker to read it easily, for example using a folder that holds the pages together well, with clearly labelled appendices.
How is my Supervisor Involved?
When you start your placement, you should indicate to your supervisor that you will need to present a report on one of your cases and outline the format for the relevant Case Report. In this way your supervisor may be able to guide your choice of case for the report. You should ensure that you do not leave your placement without getting anonymised copies from the file of all essential information. Your supervisor should read the report and sign the Validation Form before you submit both the report and the form. Copies of the validation forms are contained within this handbook (see intranet).
What Guidance or Help Can I Expect?
For all pieces of assessed programme work, trainees are actively encouraged to seek advice from others, especially supervisors, lecturers and programme staff. Seeking advice is viewed as a way of making use of available resources and is viewed positively by the programme. Advice secured by trainees may not always be consistent. It is the trainees’ responsibility to make decisions when advice is not in agreement.
For both Case Reports, ACA and SRP research projects, advice is likely to be sought at two stages, namely:
- choosing a suitable case/project
- writing up the case/ACA/SRP
It is usually the case that supervisors and programme team members focus on different aspects of the reports when marking. As a rule, supervisors will concentrate primarily on the clinical competence aspect of the report, for example, checking it is an accurate description of the clinical work. The programme team will look at the safety and validity of the work and will also consider the extent to which the report adheres to the guidelines in the programme assessment procedures e.g. are the hypotheses clear? Is the formulation adequate and appropriately linked to theory?
It is important to note that incorporating the advice of either supervisors or programme team members will not guarantee that the assignment will be passed by the assessors. The aim of the advice is to help the trainee to improve the report. As such they are formative comments and not an assessment procedure.
Audits of Clinical Activity
An audit of clinical activity (ACA) needs to be conducted before the end of Year two and it is designed to develop specific audit skills for use within clinical settings and services. Clinical psychologists (in collaboration with audit departments) are often called upon to assist with auditing various activities within their service and it can be regarded as a core skill for clinical psychologists. This type of health service audit is often vital for ensuring efficiency and good outcomes for existing health services.
What is an ACA?
The ACA is a piece of work in which the trainee, in their first or second year of training, needs to complete an audit of clinical work in collaboration with the Trust’s audit department or equivalent. This work will establish protocols for organising an audit, including the use of a priori audit standards drawn from professional, empirical and policy documents as necessary. In order to complete the ACA, the trainee needs to locate a piece of clinical work from placement for which they can audit outcomes. This work would then need to be written up as a report for the service and submitted for examination. The word limit is 2000 words excluding the title page, contents page and appendices, plus trainees need to provide an additional 100 word summary of the work.
ACA aims and objectives
The ACA has the following principle aims:
- To develop students’ ability to understand and apply audit in NHS settings
- To develop students’ ability to audit appropriate aspects of a clinical service, with a view of improving the service and its outcomes.
Having completed an ACA, trainees will have demonstrated that they are able to:
- Critically appraise published research and audit findings and apply these to real-life clinical/ health service problems
- Understand the importance of Governance processes and procedures
- Conduct an audit that fits with the needs of the service which initially commissioned the work.
- Link with colleagues and NHS organisational structures, such as audit departments.
- Disseminate their work to peers and colleagues.
Developing an ACA
The ACA is undertaken in the first two years of training and the first step for a trainee is to identify a potential topic for an ACA. The topic of the audit must be related to a service need. It is difficult to specify the exact means by which ACAs are identified, because this will depend on service needs at any particular time. Thus, trainees should be both proactive and open to suggestions. A formal teaching session is timetabled at the beginning of Year 1 to assist in this process. However, the principal academic and practical support for the ACA should come from the trainee’s clinical supervisor. It should be remembered that the ACA is intended to be a placement-based and placement-relevant activity.
Practical considerations that must be considered are that the ACA should be completed within the resources and time of the placement, that it must not jeopardise other placement requirements and that it can be safely carried out whilst on placement.
Scrutiny of ACA Proposals
Once a potential ACA is identified, the trainee should complete the ACA proposal form and submit this to the deputy research director (Peter Taylor) for scrutiny to ensure that the proposed ACA is of an appropriate scope and focus. This process includes advising trainees if their proposed project is over ambitious as well as inappropriately modest and determining whether the ACA is in line with the ClinPsyD programme requirements and feasible given available time and resources.
The involvement of members of the Programme Team in scrutinising the proposal will also help to ensure that the topic and the plan are appropriate and to check for potential pitfalls. The proposal will be scrutinised within 15 working days. All proposals must be approved by the Deputy Research Director and projects that are submitted without being approved will not be marked.
Trainees are strongly encouraged to submit their proposals as soon as possible to allow time for any revisions to be made. Proposals MUST be submitted at least 6 weeks prior to the end of the placement. No proposals will be approved after this time.
Once an ACA has been formally approved by the Deputy Research Director, the Trainee and their Supervisor should, as far as is possible, conduct the work within the current clinical placement. Trainees are advised to seek appropriate guidance and advice available to them on placement. Such sources might include their current supervisor, other clinicians and NHS-based researchers, Trust R&D committees and local clinical audit offices.
If an ACA that has been approved by the Deputy Research Director is no longer feasible to complete (e.g. due to external placement related factors), the trainee can stop the ACA and attempt to conduct another ACA on a different placement. In these instances the trainee should inform the programme team (by emailing Megan Brown) that they no longer intend to continue with the approved ACA, and give their reasons for this.
Format of ACA Presentations
Each trainee has to complete the work on placement and supply a report to the service detailing the findings from the audit. It is expected that the format of the report will include:
- Summary
- Context of audit, including service need and any engagement with stakeholders
- Audit standards
- Methodology
- Results
- Action plans, including plans for re-audit
- Reference list (APA format)
- Appendices
The ACA mark sheet, which is available for download on the programme VLE (Canvas), provides details about the kinds of information required in each section of the report.
All information which identifies the service or individual stakeholders should be removed from the report.
Deadlines
The ACA must be completed on one of the first four core placements. The deadline for submission is six weeks from the end of the placement that the ACA was completed on. If an extension is required, this must be discussed with the Programme Team in accordance with the usual extension protocol.
Each trainee will need to submit a copy of their ACA report to the Programme Team by the end of September of the second year.
Support for Trainees or Supervisors
Peter Taylor oversees the ACAs and trainees should make contact if they have a question or concern. The team will be running a half day annual supervisor workshop on the ACAs.
Submission of ACAs
A copy of the ACA (including the ACA cover sheet, which can be downloaded from Canvas) must be emailed to Megan Brown by 9am on the day of the deadline. This should be password protected using the standard format. Information regarding this format will be sent direct to trainees. If submitting multiple documents, trainees should zip these into a folder and password protect the folder. The validation form should be submitted separately via email and not attached to the ACA or appendices as this contains the trainee name and will be saved separately.
If you hand something in late and you believe there are mitigating circumstances in relation to this, you can apply for this to be taken into account (see here for the kinds of circumstances that might constitute valid grounds for mitigation to be applied).
Resubmission of ACAs
In the event of a Pass with Minor Corrections
If an ACA report is awarded Pass with Minor Corrections (PWMC) the trainee will be sent a PWMC Form. This will outline, along with the assessment feedback provided by the marker, the shortcomings identified and the revisions required to amend the piece of work to meet the appropriate standard. The trainee is invited to meet with his or her academic advisor to discuss the feedback. Trainees will have one week from publication of results to resubmit reports that have been awarded a PWMC. Up to 100 words are allowed in the resubmitted report for any additional information that is required. Following a PWMC mark, a trainee will have a maximum of two attempts at resubmission. If the 2nd resubmission is not up to standard the piece of work will be awarded a fail and no further resubmissions are allowed.
In the event of a Fail
If an ACA is failed on examination, the trainee will be sent a Resubmission Requirements Form, outlining the shortcomings of the piece of work and noting the requirements for resubmission. The trainee is invited to meet with his or her academic advisor to discuss the feedback. Up to 100 words are allowed in the resubmitted report for any additional information that is required.
It is likely that a trainee will resubmit an ACA based on the same material as the original and amended in the light of the feedback. Trainees will have four weeks from publication of results to resubmit a failed piece of work. It is possible, however, following discussion with the tutor, for a trainee to resubmit an entirely new project on a different placement. The proposal for this project will need to be approved in the same way as the original project. The resubmitted piece of work (either from a new report or the original report) can be awarded a fail, a pass or a pass with minor corrections. If a pass with minor corrections is given, as above, the trainee has one attempt at a further resubmission. If the resubmitted piece of work receives a further fail then the trainee will no longer be allowed to continue to the Programme.
Service Related Projects
The Service Related Project (SRP) is a project that is undertaken in the final year of training and is designed to develop competencies in thinking at a strategic and organisational level. Through the SRP, trainees are encouraged to take on a leadership role and use existing research and examples of best practice in order to bring about positive change within a particular service or setting. Clinical psychologists are increasingly taking on roles where they are expected to have competence in thinking and working organisationally and the SRP component of clinical training is designed to develop the skills necessary for carrying out such work in the NHS and other settings.
What is an SRP?
For an SRP, the trainee must report on a piece of work that has been commissioned by an NHS or another organisation. It is envisaged that most trainees will carry out the SPR on their Year 3 placement, although trainees in some circumstances may identify a different service for the project or a project linked to the ClinPsyD which will be supervised by the service or course team member responsible for commissioning it. Trainees will take responsibility for identifying the idea for the project as this is an important aspect of learning. Although the responsibility for the project idea rests with the trainee, all SPRs must be deemed to be useful activity by the service lead/supervisor/member of the programme team responsible for supervising it. The programme team will also be able to guide the trainee in generating the idea and determining suitability and feasibility, both informally and via a formal process of vetting project proposals.
Examples of these projects could include, but are not limited to: staff training initiatives; ways of implementing, monitoring and evaluating change across the service; and making a business case for a new post or other service development. Trainees with an interest in engaging in research post qualification may also opt to complete a fellowship or grant application for their SRP.
SRP aims and objectives
The SRP has the following principle aims:
- To develop students’ ability to understand and apply scientific knowledge and approaches in NHS and other clinical and social care settings
- To develop students’ ability to appraise real life clinical settings, with a view of improving the service for both staff and service users.
- To help establish students’ competence in taking leadership/ownership of a particular task and see it through to completion.
Having successfully completed a SRP, trainees will have demonstrated that they are able to:
- Critically appraise published research findings and apply these to real-life clinical and health service problems
- Plan service level assessments and organisational interventions in clinical and health service settings
- Understand governance processes and procedures
- Conduct an independent service development piece of work that fits with the needs of the service which initially commissioned the work
- Take leadership on a piece of strategic work within a clinical context
- Disseminate their work to peers and colleagues
Developing an SRP
The SRP is undertaken in the final year of training, normally after thesis hand-in. The first step for a trainee is to identify a potential topic for a SRP, which must be related to service need and have been commissioned by an NHS or other health or social care provider. As with ACAs, it is difficult to specify the exact means by which SRPs are identified, because this will depend on service needs at any particular time. Thus, trainees should be both proactive and open to suggestions. A formal teaching session is timetabled in Year 3 to assist in this process. However, the principal academic and practical support for the SRP should come from the trainee’s clinical supervisor or the person commissioning the project. It should be remembered that the SRP is intended to be a placement-based and placement-relevant activity.
Practical considerations which must be considered are that the SRP should be completed within the time resources and time available, and that it must not jeopardise other placement requirements.
There are no set days allocated for SRPs, but as a rule of thumb trainees should spend one day a week after handing in their thesis on the SRP. However, time within the one day a week also needs to be used for activities such as preparing for viva, addressing reviewer comments on papers and making corrections to the thesis. It is not therefore expected that the whole day will be used for the SRP, if the trainee has competing research demands. Please note that we do not typically permit trainees who are behind with their thesis to move SRP days to give themselves extra time to complete thesis-related activities prior to handin. See Assessment of Research section of the handbook for more detailed information about applying for an extension to the thesis.
Scrutiny of SRP Proposals
Once a potential SRP is identified, a detailed proposal must be developed using the SRP proposal proforma. This will normally be submitted after hand-in of the Large Scale Research Project (please see academic year planners for precise deadlines).
The scrutiny process includes advising trainees if their proposed project is over ambitious as well as inappropriately modest and determining whether the SRP is in line with the programme requirements and is feasible given available time and resources. The involvement of members of the programme team in scrutinising the proposal will also help to ensure that the topic and the plan are appropriate, and to check for potential pitfalls.
If a proposal is not submitted and approved for a given SRP prior to the work being carried out, the trainee will risk failing this aspect of their placement.
It is not necessary for the trainee to collect any data, but where appropriate the project needs to be discussed with the Trust department for audit and quality improvement and if applicable registered as a service development project. Registering the project in this way is unlikely to be a lengthy process as this is not the same as requiring ethical approval for a research project. There are clear national guidelines that Trusts use on what constitutes research, audit and service development. Carrying out surveys/interview does not automatically mean that the activity constitutes research requiring ethical approval.
Supervision of SRPs
It is intended that the SRP be supervised by the clinical supervisor(s) for the final year placement on which it is being carried out. In some circumstances, it may be appropriate for this supervision to be carried out by another supervisor due to shared supervisory responsibilities, specific research interests or the project being based in a different service to the main Year 3 placement.
Assessment of SRPs
The SRP must be completed over the final year placement and will be assessed by supervisors/project commissioners using the standard evaluation of placement forms at the end of the placement. Trainees will also be required to produce a poster presentation at the end of training, which will normally be presented at the programme’s Annual Review day in September. The assessment process will be reviewed for future cohorts.
Support for trainees and supervisors for the SRP
It is envisaged that the SRP will be carried out under the same supervisory arrangements as the other agreed placement goals. In order to facilitate this, there are a number of mechanisms to support placement supervisors in the supervision of SRPs. These include:
Formal Teaching – a teaching session is scheduled in Year 3 for SRPs (for trainees only).
SRP proforma – all potential SRPs have to be initially submitted for scrutiny by the programme team, following which appropriate feedback on the acceptability and feasibility of the proposed work will be provided. If it is thought that a proposed project is unsuitable, this will be conveyed to the trainee. At this stage, a meeting with a member of the programme team may need to be arranged to look at the proposed SRP work.
Mid-placement visit (MPV) – a review of progress of the SRP will be incorporated in the protocol for mid-placement visits by the trainee’s clinical tutor.
Supervisor training programme – workshops on the supervision of SRPs are planned as part of the ongoing supervisor training provided by the programme and will be run on an annual basis. Please contact the programme for more details.
Procedures following failed work
At the end of each of the first and second years, trainees must satisfy the Exam Board that they have achieved a satisfactory standard of progress to continue to the next academic year. Students will be appraised on their examinations, placements, case reports and, where appropriate, ACA.
Trainees who, in the opinion of the Exam Board, fail to achieve the required standard will be deemed to have failed the Programme and will be disqualified from continuing further.
If the trainee fails to hand in their case reports, ACA or SRP by the given deadlines, or fails to satisfy the examiners that a report which has previously been failed has been sufficiently improved, they will be considered to have failed that report.
A trainee may also fail the Programme if attendance is unsatisfactory, or there is some other serious professional misconduct.
In any of these cases, a Progress Board would meet to decide the action to be taken.
Actions to be taken in case of failures of examinations / assessments / placements
Please click on link below for flow charts:
Mitigating Circumstances
Sometimes circumstances or events beyond your control may adversely affect your ability to perform in an assessment to your full potential or to complete an assignment by the set deadline. In such cases, mitigation may be applied i.e. treating marks or results in a way that recognises the adverse impact that may have resulted from those circumstances or events, or waiving penalties that would arise from late submission. Please read the guidance carefully, noting the kinds of circumstances for which mitigation can, and cannot be given. Possible mitigating circumstances can be discussed with your clinical tutor.
Possible grounds for mitigation are outlined in the University’s Policy on Mitigating Circumstances, which can be downloaded here.
Programme Procedure for Mitigation
Trainees requesting consideration of mitigating circumstances should contact their Clinical Tutor.
The Clinical Tutor will discuss the process and give the trainee the Notification of Mitigating Circumstances Form. The Trainee will also be directed to the relevant section of the Programme Handbook, and the University of Manchester Policy on Mitigating Circumstances. The University also provides a basic guide to Mitigating Circumstances, which can be downloaded here.
The Clinical Tutor will be clear that whilst they may give guidance, the Mitigation Panel determines whether or not a request for consideration of mitigating circumstances is approved.
The Notification of Mitigating Circumstances Form should be submitted as early as possible to Megan Brown. It will not be accepted without prior discussion with the Clinical Tutor.
The Notification of Mitigating Circumstances Form should include the date of the onset of the circumstances and, where appropriate, documentary evidence, for example, sick note from their doctor.
The request will be acknowledged in writing and the date given of the Mitigation Panel Meeting at which it will be considered.
As a rule, requests for consideration of mitigating circumstances will apply to particular pieces of work stated on the Notification of Mitigating Circumstances Form. Where the need for consideration continues, additional forms should be submitted for subsequent pieces of work.
Where an extension has been agreed, trainees should be informed that mitigation does not automatically apply and a request for consideration of mitigating circumstances must be sought separately. Extensions, where granted, will generally be considered to have met the trainees’ needs to submit an acceptable piece of work without the need for further mitigation.
The Administrators will ensure that requests for mitigation are brought to a Mitigation Panel Meeting prior to the assessment being marked.
Consideration of mitigation will be discussed anonymously.
The Mitigation Panel can make a range of recommendations, including (but not limited to): considering the mark as a Pass, asking the student to resit the assessment but without the resit penalty, or abolishing the original mark and asking the student to submit a new piece of work. Mitigation will be applied on a case-by-case basis in the most appropriate way. All recommendations of the Mitigation Panel need to be ratified by the Exam Board, which may include Chair’s action.
Trainees will be instructed to discuss the original mark with either their Academic Advisor or Clinical Tutor.
Procedure ratified at the Executive Training Programme Committee, September 2007.
Last updated: December 2016
Competence Frameworks
Introduction to Competence Frameworks
Overview
The British Psychological Society requires all Clinical Psychology doctorates to provide training in at least two evidence-based forms of psychological intervention, of which one must be cognitive-behaviour therapy (CBT). On the Manchester ClinPsyD, we have adopted four main evidence-based models of psychological intervention: CBT, Psychodynamic Interpersonal Therapy (PIT)/brief psychodynamic therapy/Cognitive Analytic Therapy, systemic therapy and Clinical Neuropsychology. Each of these has been benchmarked against a different external competence framework. We also set out a number of generic clinical competences that have to be demonstrated on the programme regardless of the specific models used.
Choice of frameworks
The Programme team spent a long time deciding how to approach the competence benchmarking process. In an ideal world, trainees would be able to pick any evidence-based approach as their “second model” (i.e., in addition to CBT) and demonstrate competence in that. In practice, however, there is a limit on how many models we can teach to a reasonable level on the Programme, as well as on the availability of supervisors who are qualified in different approaches. In addition, the process of identifying suitable competence frameworks, benchmarking training against them and then evaluating trainees’ performance against the associated standards involves a considerable amount of work. This has meant focusing on a core set of approaches that we consider ourselves to have some expertise in, and which collectively provide a rounded set of training experiences and therapeutic competences. In order to graduate from the Manchester ClinPsyD, trainees must have demonstrated knowledge of, and the ability to formulate using, all four of these approaches (we call this Level 1 competence). In addition, they must have demonstrated competence in intervening (at either Level 2 or 3; see Table 1) using CBT plus at least one of the other core approaches. An overview of the different levels in the four approaches is presented in Table 1, along with information about how those standards are delivered and evaluated.
Overview of competence levels on the Manchester ClinPsyD programme
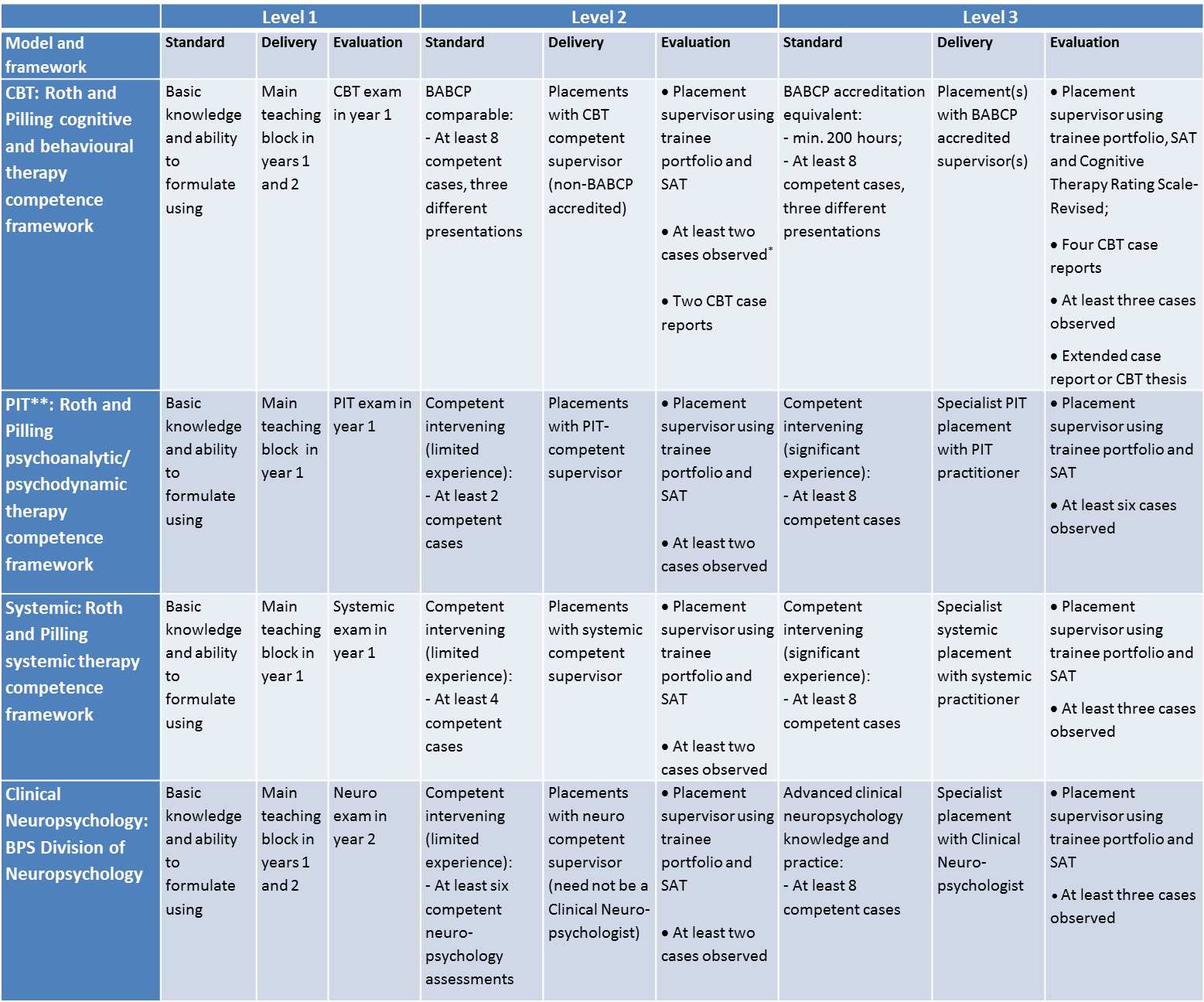
KEY: BABCP = British Association for Behavioural and Cognitive Psychotherapies; CBT = Cognitive Behaviour Therapy; CTSR = Cognitive Therapy Rating Scale-Revised; PIT = Psychodynamic Interpersonal Therapy; SAT = Supervisor Assessment of Trainee form; * Observations can be either live or audio/video recorded except for BABCP accreditation equivalence, where recordings must be live or video-recorded only; ** Level 2 psychodynamic competence can also be demonstrated in a different model to PIT.
The external frameworks specify the various competencies that are considered central to that particular psychological approach. Which competencies must be demonstrated in order to be considered competent in that approach depends on the model in question. Further information about this can be found by following the links above for the individual frameworks. None of the external competence frameworks themselves dictate how many clients must be seen before a practitioner can be considered competent using that approach. We have therefore set minimum standards in relation to this, making reference to other external standards as appropriate.
The basic competencies are the same for both Level 2 and Level 3 competence; however, we distinguish between these levels to recognise variations in the extent or level of experience gained in each therapeutic modality. Thus, someone who has achieved Level 2 competence in a particular model will have shown that they are able to intervene competently using that approach, but to a lesser extent or level than someone who has achieved Level 3 competence. A central function of the clinical portfolio is to track the trainee’s progress in relation to acquiring Level 2 and 3 competences in the four core clinical approaches.
Delivery and evaluation of competences
The taught programme is designed to provide Level 1 competence in each of the four models, which will be evaluated in the corresponding written examinations. At Level 2, competence is demonstrated through the delivery of interventions with a minimum number of cases on placement, which can either be core or elective placements as long as the supervisor has the required expertise (see placement section). In order to achieve Level 3 competence, the trainee must undertake a specialist placement in the relevant modality and demonstrate competence in a larger number of cases. We expect all of the generic competencies to be acquired through teaching and placement experience in general, and can be demonstrated on any placement using any approach.
In order for a case to “count” as an example of competent clinical work within one of the frameworks, the trainee and supervisor must agree that the primary approach to intervention falls under the umbrella of that framework. The supervisor must also confirm that the work was carried out competently. Each case can only count towards competence in one model (i.e., the predominant therapeutic approach), even if multiple models informed the work in question. When completing their Clinical Portfolio, trainees must indicate which of the relevant competencies were demonstrated with each case, and this must be signed off an accurate record of the work by the supervisor.
Can I demonstrate competence in other models instead?
Trainees are likely to acquire knowledge of, and experience using, other clinical approaches whilst studying for the ClinPsyD. Although we regard this as positive, all trainees will still need to demonstrate at least Level 2 competence in CBT plus one of the other core therapeutic models taught on the Programme in order to graduate.
Generic Clinical Competencies
In order to pass the programme, all trainees must have demonstrated the following generic competencies, which are based on the UCL Core Competency frameworks and assessed using the Supervisor Assessment of Trainee (SAT) form. A document mapping these competencies onto the SAT form can be downloaded here.
1. Knowledge and understanding of mental health problems
During assessment and when carrying out interventions:
- An ability to draw on knowledge of common mental health problems and their presentation
- An ability to draw on knowledge of the factors associated with the development and maintenance of mental health problems
- An ability to draw on knowledge of the usual pattern of symptoms associated with mental health problems
- An ability to draw on knowledge of the ways in which mental health problems can impact on functioning (e.g. maintaining intimate, family and social relationships, or the capacity to maintain employment and study)
- An ability to draw on knowledge of the impact of impairments in functioning on mental health
- An ability to draw on knowledge of mental health problems to avoid escalating or compounding the client’s condition when their behaviour leads to interpersonal difficulties which are directly attributable to their mental health problem
2. Knowledge of, and ability to operate within, professional and ethical guidelines
An ability to maintain awareness of national and local codes of practice which apply to all staff involved in the delivery of healthcare, as well as any codes of practice which apply to the therapist as a member of a specific profession
An ability to take responsibility for maintaining awareness of legislation relevant to areas of professional practice in which the therapist is engaged (specifically including the Mental Health Act, Mental Capacity Act, Human Rights Act, Data Protection Act)
3. Application of professional and ethical guidelines
An ability to draw on knowledge of relevant codes of professional and ethical conduct and practice in order to apply the general principles embodied in these codes to each piece of work being undertaken, in the areas of:
- obtaining informed consent for interventions from clients
- maintaining confidentiality, and knowing the conditions under which confidentiality can be breached
- safeguarding the client’s interests when co-working with other professionals as part of a team, including good practice regarding inter-worker/ inter-professional communication
- competence to practice, and maintaining competent practice through appropriate training/professional development
- recognition of the limits of competence and taking action to enhance practice through appropriate training/professional development
- protecting clients from actual or potential harm from professional malpractice by colleagues by instituting action in accordance with national and professional guidance
- maintaining appropriate standards of personal conduct for self:
- a capacity to recognise any potential problems in relation to power and “dual relationships” with clients, and to desist absolutely from any abuses in these areas
- recognising when personal impairment could influence fitness to practice, and taking appropriate action (e.g. seeking personal and professional support and/or desisting from practice)
4. Ability to work with difference (cultural competence)
An ability to maintain an awareness of the potential significance for practice of social and cultural difference, across a range of domains, including:
- ethnicity
- culture
- class
- religion
- gender
- age
- disability
- sexual orientation
For all clients with whom the therapist works, an ability to draw on knowledge of the relevance and potential impact of social and cultural difference on the effectiveness and acceptability of an intervention.
Where social and cultural difference impacts on the accessibility of intervention, an ability to make appropriate adjustments to the therapy, with the aim of maximising its potential benefit to the client
5. Knowledge of a model of therapy, and the ability to understand and employ the model in practice
An ability to draw on knowledge of factors common to all therapeutic approaches:
- a positive working relationship between therapist and client characterised by warmth, respect, acceptance and empathy, and trust
- the active participation of the client
- therapist expertise
- opportunities for the client to discuss matters of concern and to express their feelings
- learning factors:
- advice
- correctional emotional experience
- feedback
- exploration of internal frame of reference
- changing expectations of personal effectiveness
- assimilation of problematic experiences
- action factors:
- behavioural regulation
- cognitive mastery
- encouragement to face fears and to take risks
- reality testing
- experience of successful coping
An ability to draw on knowledge of the principles which underlie the intervention being applied, using this to inform the application of the specific techniques which characterise the model.
An ability to draw on knowledge of the principles of the intervention model in order to implement therapy in a manner which is flexible and responsive to client need, but which also ensures that all relevant components are included.
6. Ability to engage client
While maintaining professional boundaries;
- An ability to show appropriate levels of warmth, concern, confidence and genuineness, matched to client need
- An ability to engender trust
- An ability to develop rapport
- An ability to adapt personal style so that it meshes with that of the client
- An ability to recognise the importance of discussion and expression of client’s emotional reactions
- An ability to adjust the level of in-session activity and structuring of the session to the client’s needs
- An ability to convey an appropriate level of confidence and competence
- An ability to avoid negative interpersonal behaviours (such as impatience, aloofness, or insincerity)
7. Ability to foster and maintain a good therapeutic alliance, and to grasp the client’s perspective and ‘world view’
7.1 Understanding the concept of the therapeutic alliance
An ability to draw on knowledge that the therapeutic alliance is usually seen as having three components:
- the relationship or bond between therapist and client
- consensus between therapist and client regarding the techniques/methods employed in the therapy
- consensus between therapist and client regarding the goals of therapy
An ability to draw on knowledge that all three components contribute to the maintenance of the alliance
7.2 Knowledge of therapist factors associated with the alliance
An ability to draw on knowledge of therapist factors which increase the probability of forming a positive alliance:
- being flexible and allowing the client to discuss issues which are important to them
- being respectful
- being warm, friendly and affirming
- being open
- being alert and active
- being able to show honesty through self-reflection
- being trustworthy
Knowledge of therapist factors which reduce the probability of forming a positive alliance:
- being rigid
- being critical
- making inappropriate self-disclosure
- being distant
- being aloof
- being distracted
- making inappropriate use of silence
7.3 Capacity to develop the alliance
- An ability to listen to the client’s concerns in a manner which is non-judgmental, supportive and sensitive, and which conveys a comfortable attitude when the client describes their experience
- An ability to ensure that the client is clear about the rationale for the intervention being offered
- An ability to gauge whether the client understands the rationale for the intervention, has questions about it, or is sceptical about the rationale, and to respond to these concerns openly and non-defensively in order to resolve any ambiguities
- An ability to help the client express any concerns or doubts they have about the therapy and/or the therapist, especially where this relates to mistrust or scepticism
- An ability to help the client articulate their goals for the therapy, and to gauge the degree of congruence in the aims of the client and therapist
- Capacity to grasp the client’s perspective and ‘world view’ An ability to apprehend the ways in which the client characteristically understands themselves and the world around them
- An ability to hold the client’s world view in mind throughout the course of therapy and to convey this understanding through interactions with the client, in a manner that allows the client to correct any misapprehensions
- An ability to hold the client’s world view in mind, while retaining an independent perspective and guarding against identification with the client
7.4 Capacity to maintain the alliance, including recognising and addressing threats to the therapeutic alliance (“alliance ruptures”)
An ability to recognise when strains in the alliance threaten the progress of therapy
An ability to deploy appropriate interventions in response to disagreements about tasks and goals:
- an ability to check that the client is clear about the rationale for treatment and to review this with them and/or clarify any misunderstandings
- an ability to help clients understand the rationale for treatment through using/drawing attention to concrete examples in the session
- an ability to judge when it is best to refocus on tasks and goals which are seen as relevant or manageable by the client (rather than explore factors which are giving rise to disagreement over these factors)
An ability to deploy appropriate interventions in response to strains in the bond between therapist and client:
- an ability for the therapist to give and ask for feedback about what is happening in the here-and-now interaction, in a manner which invites exploration with the client
- an ability for the therapist to acknowledge and accept their responsibility for their contribution to any strains in the alliance
- where the client recognises and acknowledges that the alliance is under strain, an ability to help the client make links between the rupture and their usual style of relating to others
- an ability to allow the client to assert any negative feelings about the relationship between the therapist and themselves
- an ability to help the client explore any fears they have about expressing negative feelings about the relationship between the therapist and themselves
8. Ability to manage the emotional content of sessions
An ability to facilitate the processing of emotions by the client, including acknowledging and containing emotional levels that are too high (e.g. anger, fear, despair) or too low (e.g. apathy, low motivation)
An ability to deal effectively with emotional issues that interfere with effective change (e.g. hostility, anxiety, excessive anger, avoidance of strong affect).
An ability to help the client access differentiate and experience his/her emotions in a way that facilitates change.
9. Ability to manage endings
An ability to signal the ending of the intervention at appropriate points during the therapy in a way which acknowledges the potential importance of this transition for the client, for example:
- when agreeing the treatment contract
- as the intervention draws to close
An ability to help client discuss their feelings and thoughts about endings and any anxieties about managing alone
An ability to review the work undertaken together
An ability to say goodbye
10. Ability to undertake a generic assessment
An ability to obtain a general idea of the nature of the client’s problem
An ability to elicit information regarding psychological problems, diagnosis, past history, present life situation, attitude about and motivation for therapy
An ability to gain an overview of the client’s current life situation, specific stressors and social support
An ability to assess the client’s coping mechanisms, stress tolerance, and level of functioning
An ability to help the client identify/select target symptoms or problems, and to identify which are the most distressing and which the most amenable to intervention
An ability to help the client translate vague/ abstract complaints into more concrete and discrete problems
An ability to assess and act on indicators of risk (of harm to self or others) (and the ability to know when to seek advice from others)
An ability to gauge the extent to which the client can think about themselves psychologically (e.g. their capacity to reflect on their circumstances or to be reasonably objective about themselves)
An ability to gauge the client’s motivation for a psychological intervention
An ability to discuss treatment options with the client, making sure that they are aware of the options available to them, and helping them consider which of these options they wish to follow
An ability to identify when psychological treatment might not be appropriate or the best option, and to discuss this with the client, for example:
- where the client’s difficulties are not primarily psychological
- the client indicates that they do not wish to consider psychological issues)
- the client indicates a clear preference for an alternative approach to their problems (e.g. a clear preference for medication rather than psychological therapy)
11. Ability to make use of supervision
An ability to hold in mind that a primary purpose of supervision and learning is to enhance the quality of the treatment clients receive
11.1 An ability to work collaboratively with the supervisor
An ability to work with the supervisor in order to generate an explicit agreement about the parameters of supervision, for example agreeing about:
- how the agenda for supervision will be set
- the respective roles of supervisor and supervisee
- the aims and goals of supervision
An ability to help the supervisor be aware of your current state of competence and your training needs
An ability to present an honest and open account of clinical work undertaken
An ability to discuss clinical work with the supervisor as an active and engaged participant, without becoming passive or avoidant, or defensive or aggressive
An ability to present clinical material to the supervisor in a focussed manner, selecting the most important and relevant material
11.2 Capacity for self-appraisal and reflection
An ability to reflect on the supervisor’s feedback and to apply these reflections in future work
An ability to be open and realistic about your capabilities and to share this self-appraisal with the supervisor
An ability to use feedback from the supervisor in order further to develop the capacity for accurate self-appraisal
11.3 Capacity for active learning
An ability to act on suggestions regarding relevant reading made by the supervisor, and to incorporate this material into clinical practice
An ability to take the initiative in relation to learning, by identifying relevant papers, or books, based on (but independent of) supervisor suggestions, and to incorporate this material into clinical practice
11.4 Capacity to use supervision to reflect on developing personal and professional role
An ability to use supervision to discuss the personal impact of the work, especially where this reflection is relevant to maintaining the likely effectiveness of clinical work
An ability to use supervision to reflect on the impact of clinical work in relation to professional development
11.5 Capacity to reflect on supervision quality
An ability to reflect on the quality of supervision as a whole, and (in accordance with national and professional guidelines) to seek advice from others where:
- there is concern that supervision is below an acceptable standard
- where the supervisor’s recommendations deviate from acceptable practice
- where the supervisor’s actions breach national and professional guidance (e.g. abuses of power and/or attempts to create dual (sexual) relationships)
Cognitive Behaviour Therapy Competence Framework
The British Psychological Society Standards for the Accreditation of Doctoral Programmes in Clinical Psychology stipulate that all Clinical Psychology programmes have to equip students with the ability to intervene using Cognitive Behaviour Therapy (CBT). It is therefore a requirement that all trainees on the Manchester ClinPsyD meet at least Level 2 competence in CBT in order to graduate (see below for details of what Level 2 competence consists of). The Manchester ClinPsyD Programme has always been seen as very strong in CBT and, accordingly, we set quite high standards in relation to this aspect of training.
In this section, we set out the various CBT competencies that trainees are expected to acquire whilst on the Programme. They are closely based on the UCL competencies for Cognitive and Behavioural Therapy set out by Roth and Pilling (2007) and those set out in the Cognitive Therapy Rating Scale – Revised (CTS-R, Blackburn, James, Milne & Reichelt, 2000), although are not an absolute replica. Competencies have been added to take into account specific client presentations that trainees learn about through teaching, as well as the ability for trainees to use CBT across different populations.
Levels of CBT competence
As with all of the main therapeutic models on the Manchester programme, we distinguish between three different levels of competence. Levels 2 and 3 are benchmarked against the minimum training standards for the practice of CBT set out by the British Association for Behavioural and Cognitive Psychotherapies.
Level 1 competence
Level 1 competence corresponds to having essential knowledge about, and the ability to formulate using, CBT. This level of competence will, as a minimum, be delivered via the taught component of the Programme, particularly the CBT for common mental health problems and Specialist topics in cognitive therapy modules of the curriculum, and will be examined in the Adult and Child exams in Year 1. Teaching will cover all of the competencies outlined below, although it is recognised that a much greater level of knowledge and understanding will be acquired through supervised clinical work.
Level 2 competence
Competence at Level 2 has been set to approximate the minimum training standards for BABCP accredited practitioners. More specifically, trainees meeting this standard will, as a minimum, have:
- passed the Adult and Child exams;
- completed competent CBT work with at least eight clients, over at least five sessions;
- demonstrated all of the “basic” CBT competencies and all of the CBT metacompetencies described below (i,e., every competence within A and D);
- demonstrated problem-specific CBT competence with at least three of the different types of mental health condition (anxiety disorder, depression, psychosis etc.) listed below under C;
- at least three clinical cases must have been observed directly (either “live” or in a recording) by the supervisor;
- passed at least two case reports where CBT was the main approach used;
We adopt a broad definition of what constitutes CBT, encompassing all of the so-called “generations” or “waves” of cognitive behavioural therapies and their use with a wide range of clinical presentations and client groups. We anticipate that trainees will be able to acquire competencies in CBT in all of their core placements. For example, an intervention conducted with a client with learning disabilities could qualify as a CBT case if it is primarily informed by cognitive and/or behavioural principles, as could a piece of indirect work conducted via a system (e.g., an intervention for an anxious child, conducted via their parents).
At this level, there is no requirement that the intervention component of each piece of work involve a minimum number of sessions, as long as trainee and supervisor agree that a meaningful piece of therapy was conducted. There is also no minimum requirement in relation to any of the specific behavioural and cognitive therapy techniques (B competencies), although trainees should still record in their Clinical Portfolio where these competencies have been demonstrated so it is clear which skills have been acquired. The idea is that graduates will be able to say that they meet a basic standard in CBT, along with specific competencies using a, b and c skills/techniques with x, y and z clinical problems.
In order to say that a problem-specific competence has been demonstrated, the work must have involved one of the models referred to below or another evidence-based model, which must be specified. To count as evidence of problem-specific competence in using CBT for panic disorder, for example, the work must have been based on either the Clark or Barlow models of panic, or another model for which there is published evidence of validity and efficacy. Thus, whilst it is acceptable to use generic and/or idiosyncratic approaches to case formulation and intervention if they are clinically appropriate, formulations that draw on several models cannot count towards any of the problem-specific competencies, which all require dedicated use of a specific, evidence-based model to guide formulation and treatment. This applies even if the person in question would meet criteria for a specific presenting problem. Nevertheless, work based on a generic and/or idiosyncratic formulation could still count as a “CBT case” if CBT was the primary therapeutic approach used, and relevant skills, techniques and metacompetencies were demonstrated.
Our aim in bench-marking Level 2 competence in CBT against the BABCP minimum training standards are to (1) enable graduates of the Manchester ClinPsyD to be able to say that their CBT training is comparable to that of a BABCP accredited practitioner; and (2) to make it easy for graduates of the programme to apply for accreditation with the BABCP after they qualify should they wish to pursue this. Nevertheless, there are important differences between the BABCP training standards and Level 2 competence on the Manchester programme. In particular, there is no requirement that trainees must have conducted a minimum of 200 hours of supervised CBT assessment and therapy during the Programme, or that they must have been supervised by a BABCP accredited/accreditable therapist. In addition, trainees are only expected to produce two case reports where the primary intervention was CBT (rather than the four required by the BABCP) and there is no requirement for trainees to produce an extended case report or thesis based on CBT at Level 2.
Level 3 competence
Competence at Level 3 is designed to be directly equivalent to the BABCP minimum training standards. More specifically, trainees meeting this standard will, as a minimum, have:
- passed the Adult and Child exams;
- completed a third year specialist placement using CBT as the primary therapeutic approach, supervised by a BABCP accredited/accreditable practitioner;
- conducted a minimum of 200 hours of supervised CBT assessment and therapy whilst on the programme;
- demonstrated all of the “basic” CBT competencies and all of the CBT metacompetencies described below (i,e., every element of A and D);
- completed competent CBT with at least eight clients, consisting of at at least five intervention sessions each;
- demonstrated competence in problem-specific CBT with at least three different types of mental health condition (anxiety disorder, depression etc.) as listed under C below;
- at least three clinical cases must have been observed directly (either “live” or in a recording) by the supervisor, using a standardised assessment measure (e.g. Cognitive Therapy Rating Scale, Revised) in at least one;
- completed four case reports where CBT was the main approach used (of which two must be completed whilst on specialist CBT placement and evaluated by your supervisor);
- completed (one of) an extended case report critically discussing the evidence for CBT, a CBT relevant research dissertation or a CBT relevant research paper;
In addition to fostering the development of a deeper level of knowledge and competence in CBT, our hope in setting these additional requirements is to enable graduates with competence at this level to be able to apply for BABCP accreditation as soon as possible following qualification, with a minimum of additional work (in contrast, someone qualifying with Level 2 competence may need to do more clinical work, produce additional case reports, complete an extended essay and so on before applying for accreditation). It is our intention to pursue accreditation from the BABCP for this pathway through training, such that trainees meeting this level of competence automatically qualify as BABCP accredited practitioners. We will inform trainees as soon as we have further information about this.
Specific CBT competencies
Most of the individual competencies listed below are part of the UCL competence framework in CBT and have been reproduced verbatim. Click on the individual items in purple for further information about the elements of that competence. When completing the Clinical Portfolio, trainees and supervisors should refer to the content of each item to judge whether the overarching competence was demonstrated whilst on placement. There is no expectation that each of the individual elements within a competence will be “ticked off”, however, and the Portfolio is therefore not designed with this in mind.
A. Basic CBT competencies (required for Level 2 and 3 competence)
A1. Knowledge of the basic principles that underpin CBT and the rationale for treatment
A2. Knowledge of common cognitive biases relevant to CBT
A3. Knowledge of the role of safety behaviours
A4. Explaining and demonstrating the rationale for behavioural and for cognitive behavioural therapy
A5. Ability to agree goals for the intervention
A6. Ability to structure sessions
A7. Sharing responsibility for session structure and content
A8. Collaborative agenda setting
A9. Ability to adhere to an agreed agenda
A10. Use of bridging between sessions
A11. Ability to plan and to review out of session practice (‘homework’) assignments
A12. Use of summaries and two way feedback to structure the session
A13. Ability to use measures and self-monitoring to guide therapy and to monitor outcome
A14. Ability to develop hypotheses about a maintenance cycle and to use the maintenance cycle to set targets for intervention
A15. Ability to problem solve
A16. Ability to pace sessions and use time efficiently
A17. Ability to work collaboratively throughout therapy – evidenced by verbal skills, non-verbal skills and summaries (both verbal and written)
A18. Ability to end therapy in a planned manner and to plan for long-term maintenance of gains after treatment ends
A19. Ability to demonstrate interpersonal effectiveness (e.g. warmth, genuineness, empathy and understanding) within professional boundaries
A20. Evidence of teamwork with open and explicit two-way feedback.
B. Specific CBT competencies
B1. Knowledge of exposure techniques and how they can be used
B2. Knowledge of activity monitoring and activity scheduling
B3. Ability to use guided discovery and socratic questioning
B4. Ability to use thought records
B5. Ability to identify and work with safety behaviours
B6. Ability to detect, examine and help the client reality teach automatic thoughts and images
B7. Ability to elicit key cognitions and images
B8. Ability to identify and modify assumptions, attitudes and rules
B9. Ability to identify and help the client modify core beliefs
B10. Ability to employ imagery techniques
B11. Ability to plan and conduct a behavioural experiment
B12. Ability to formulate idiosyncratically from a CBT perspective and plan treatment
B13. Ability to understand a client’s inner world and their response to therapy
C. Problem specific competencies (Presentation, Theory, Assessment, Formulation, Intervention)
Knowledge and understanding of assessment, formulation and intervention (and ability to apply this in clinical practice using cognitive therapy) for:
C1. Specific phobias i) Butler model or ii) Craske et.al. model or iii) another evidence based model (to be documented.
C2. Panic and Agoraphobia ([i] Clark model; or [ii] Barlow model; or [iii] another evidence-based model [to be documented])
C3. Social Anxiety ([i] Heimberg/Hope model; or [ii] Clark and Wells model; or [iii] another evidence-based model [to be documented])
C4. Depression ([i] Beck model; or [ii] Jacobson Behavioural Activation model; or [iii] other an evidence-based model [to be documented])
C5. Health Anxiety ([i] Warwick and Salkovskis model; or [ii] another evidence-based model [to be documented]
C6. Obsessive Compulsive Disorder ([i] Steketee/Kozac & Foa model; or [ii] another evidence-based model [to be documented])
C7. Generalised Anxiety Disorder ([i] Borkovec model; or [ii] Dugas/Ladouceur/Freeston model; or [iii] Zinbarg/Craske/Barlow model; [iv] Wells model; or [v] another evidence-based model [to be documented])
C8. Anger related difficulties (evidence-based model to be documented)
C9. PTSD ([i] Foa/Rothbaum model; or [ii] Ehlers & Clark model; or [iii] Resick model or another evidence-based model [to be documented])
C10. Survivors of abuse (evidence-based model to be documented)
C11. Dissociation (evidence-based model to be documented)
C12. Eating Disorders (evidence-based model to be documented)
C13. Psychosis (evidence-based model to be documented)
C14. Bipolar Disorder (evidence-based model to be documented)
D. CBT Meta competencies (required for Level 2 and 3 competence)
D1. Ability to implement CBT in a manner consonant with its underlying philosophy
D1.1. Ability to use CBT in a collaborative manner, with the client and trainee CP working as a team, discussing and resolving any disruptions
D1.2. Ability to use the models in a manner that is flexible and responsive to the issues the client raises, yet is still underpinned by the theoretical aspects of CBT
D1.3. Ability to adapt interventions in response to the client feedback (implicit and explicit)
D1.4. An ability to avoid seeing the client themselves as a problem, but to maintain a problem-solving approach to the client’s difficulties
D1.5. An ability to detect unhelpful elements in the relationship (e.g. dependency and/or over reliance on the trainee) and an ability to discuss and attempt to resolve them with the client
D2. Ability to formulate and to apply CBT models to the individual client
D2.1. An ability to implement the CBT model in a manner which is consonant with a comprehensive formulation that takes into account all relevant aspects of the client’s presentation
D2.2. An ability to hold the formulation in mind in order to anticipate and to respond to the client’s needs in the context of applying the CBT model
D2.3. An ability to hold the formulation in mind in order to ensure that CBT is implemented in relation to the client needs and hence in a manner: (a) which is flexible and appropriately adapted; (b) which ensures that important aspects of the client’s presentation are acknowledged (and not ignored in order to simplify the intervention); and (c) which ensures that the intervention is not reductionist or simplistic
D3. Ability to select and skillfully apply the most appropriate CBT intervention method
D4. Ability to structure sessions and maintain appropriate pacing
D5. Ability to manage obstacles to working with a CBT approach e.g. when symptoms get worse; when client behavior is counter-therapeutic, for example: find it difficult to talk/tend to talk too much; have difficulty staying focused; are persistently late
D6. Ability to continue to work in a manner which is congruent with the CBT model when client’s symptoms/problems worsen
D7. Ability to identify one’s own unhelpful cognitions, especially self-defeating thoughts relating to lack of client progress
D8. Ability to tolerate frustration and to remain task focused (e.g. in the face of slow progress)
D9. Evidence of flexibly using cognitive therapy according to the needs of the client whilst still maintaining the theoretical underpinnings of the approach
Psychodynamic Interpersonal Therapy and Other Brief Psychodynamic Therapies Competence Frameworks
Overview: Psychodynamic Interpersonal Therapy (PIT) and Other Brief Psychodynamic Therapies Competence Frameworks
All trainees are expected to demonstrate Level 1 competence in PIT and may go on to demonstrate Level 2 or 3 competence in PIT or another brief psychodynamic approach if the required clinical work is completed.
Level 1 PIT competence
As with all of the other core therapeutic approaches on the Manchester ClinPsyD, Level 1 competence in PIT consists of basic knowledge about, and the ability to formulate using, this model. The specific Level 1 competences are described below. Competence at this level will be delivered through the PIT module of the academic curriculum and will be evaluated in the Adult exam in Year 1. This level of competence is comparable to the five day course in PIT run historically by members of PIT SIG UK.
Specific Level 1 PIT competencies
At Level 1, all trainees must demonstrate the following PIT-specific competences, which have been reproduced verbatim from the PIT section of the Lemma, Roth and Pilling psychodynamic/psychoanalytic competence framework.
- An ability to draw on knowledge of the psychodynamic, humanistic and interpersonal principles underpinning the PI model
- An ability to draw on knowledge that PI therapy focuses on understanding and changing the client’s characteristic patterns of feeling and behaving in relationships
- An ability to draw on knowledge that PI therapy: (a) sees the client’s presenting problems and symptoms as originating in interpersonal patterns established in early relationships, and that these patterns inform current relationships and contribute to specific vulnerabilities (e.g. to the experience of loss); (b) aims to foster the development of a collaborative, “personal conversation” between therapist and client; (c) assumes that the client’s problems are expressed, or enacted in the client’s “here-and-now” experience in the session and hence focuses primarily on the client’s immediate experience in the session and uses the evolving relationship with the therapist as the vehicle for exploring and resolving the client’s difficulties (i.e. helping the client to discover more helpful ways of relating)
In addition, trainees will be able to derive a PIT formulation and use it to generate hypotheses about the likely impact of emotional and interpersonal factors on psychological therapy regardless of the model used.
Level 2 competence
Competence at this level requires either competent use of PIT as a standalone therapy or a different brief psychodynamic approach (e.g., Luborsky’s supportive-expressive therapy; Intensive Short-term Dynamic Psychotherapy) as long as the trainee can demonstrate that (a) the approach is evidence-based, that is, there are relevant published data concerning its validity and effectiveness as a therapeutic approach for the problem in question; (b) they have delivered the intervention as a standalone therapy; and (c) they meet all of the basic/analytic competences (see below). Cognitive Analytic Therapy (CAT) or “CAT informed” case work can also count as a suitable dynamic approach under this system, although in this case a different set of competencies need to be acquired (see below).
In each case, the therapy in question must have been delivered competently with at least two clients, each lasting a minimum of four sessions. These cases can be seen on any placement as long as they are supervised by a clinician who identifies themselves as competent to delivery and supervise PIT/the model in question. This level of clinical experience is comparable to the number of cases identified by PIT SIG UK as a requirement for successful completion of their proposed Level 2 training in PIT.
Level 3 competence
This level of competence requires significant experience using either PIT or another psychodynamic therapy (defined above). Competence at this level requires:
- a specialist third year placement in PIT/another relevant model, with regular supervision in the approach from a supervisor who is competent in the model in question;
- competent use of PIT/another relevant model as a standalone therapy with at least eight clients, each lasting a minimum of four sessions;
- at least six clinical cases must have been observed directly (either “live” or in a recording) by the supervisor (this requirement is more significant than for other models, as observation of practice is considered a central element of PIT supervision);
- demonstration of all of the specific competencies (see below);
Specific Level 2 and 3 psychodynamic competencies
In addition to the Level 1 competencies, trainees meeting Level 2 or 3 competence must have demonstrated at least one of the following:
- the PIT-specific competences (if they are using PIT)
- the CAT-specific competences (if they are using CAT or doing CAT-informed work)
- generic psychodynamic competences (if they are using a different psychodynamic approach)
The PIT and generic psychodynamic competencies have all been reproduced verbatim from the Lemma, Roth and Pilling psychoanalytic/psychodynamic framework. The CAT competencies are based on those described by Roth and Pilling in the UCL CORE framework of psychological interventions for people with personality disorder, although have been adapted slightly for our use.
Specific Level 2 and 3 competencies in PIT
The PIT competence framework is derived from the UCL Competence Framework for Psychoanalytic/Psychodynamic therapies developed by Roth and Pilling, which identifies PIT as a specific, evidence-based adaptation of the psychodynamic model. The levels of competence are benchmarked against the training standards of the PIT Special Interest Group (PIT SIG UK).
If you are using PIT, you must demonstrate the following competencies in order to meet Level 2 or 3 competence.
1. Therapeutic stance
1.1. An ability to maintain a warm, involved, empathic manner
1.2. An ability to provide support and encouragement through (a) acknowledging the client’s progress; and (b) communicating hopefulness about progress;
1.3. An ability to work collaboratively with the client to develop “shared meaning” by (a) using direct and collaborative language (e.g. ‘I’ and ‘We’) that facilitates the development of an active, mutual dialogue with the client; (b) sharing the therapist’s understanding tentatively; (c) being responsive to the client’s experience of the therapy;
2. Assessment and engagement
2.1. An ability to be attuned to, and respond to, the emerging quality of the interaction between therapist and client, including feelings generated within the therapist in response to the client
2.2. An ability to assess the client’s characteristic patterns of feeling and behaving in relationships
2.3. An ability to appraise the nature of the client’s difficulties through the way they present and relate in the session (both verbally and non-verbally)
2.4. An ability to reformulate the client’s presenting problems in an interpersonal context and to communicate this understanding to the client
2.5. An ability to orient the client to the therapy by explaining the rationale for PI therapy
2.6. An ability to jointly agree the therapeutic focus with the client
3. Interventions
3.1. Ability to focus on the client’s here-and-now experience in the session
3.1.1. An ability to help the client to stay with, and explore, what they are currently feeling, including (a) an ability to identify and respond to verbal and non-verbal cues from the client to facilitate the client’s exploration and understanding of the client’s feelings; (b) an ability to identify and appraise the significance of the therapist’s countertransference; and (c) an ability to be explicit about the cues that the therapist is using to understand the client’s experience (e.g. the client’s tone of voice/posture
3.1.2. An ability to carefully track and the client’s emotional state during the session, and to communicate an understanding of this in order to help the client to (a)recognise and accept their feelings; and (b) differentiate feelings from actions
3.1.3. An ability to build on the client’s idiosyncratic use of language (especially their use of metaphors), to (a) support the exploration of the client’s immediate experience; and (b) deepen the level of emotional exchange between therapist and client
3.2. Ability to use the therapeutic relationship to explore and address the client’s interpersonal difficulties
3.2.1. An ability to identify and respond to recurring interpersonal patterns as they are enacted in the session, including (a) an ability to help the client reflect on their perceptions of the therapist; and (b) an ability to make appropriate use of self-disclosure by the therapist to develop a shared understanding of what is happening between therapist and client
3.2.2. An ability to maintain an ongoing, mutual dialogue with the client to help them explore, within the therapeutic relationship, alternative ways of approaching their interpersonal difficulties
3.3. Ability to work collaboratively with the client to generate hypotheses about their difficulties
3.3.1. An ability to use statements (as opposed to questions) to promote an ongoing “conversation” about the client’s experience (i.e. the primary goal is not to provide ‘explanations’, but to encourage further exploration of the client’s current experience)
3.3.2. An ability to share the therapist’s understanding of the client’s experience through exploratory statements that are couched tentatively (i.e. as hypotheses open to correction/further amplification)
3.3.3. An ability to promote the exploration and organisation of the client’s affective and interpersonal experiences by generating a “hierarchy” of hypotheses, including (a) “understanding hypotheses”, which aim to communicate empathy for the client’s experience and the therapist’s perspective on the client’s experience; (b) “linking hypotheses”, which aim to establish connections between affective and interpersonal experiences within the therapy and those occurring in other contexts; and (c) “explanatory hypotheses”, which aim to draw attention to repetitive interpersonal patterns and introduce a tentative account of the underlying reasons for these patterns
3.3.4. an ability to introduce hypotheses in a progressive manner (in which “explanatory hypotheses build on “understanding” and “linking” hypotheses)
3.4. Ability to monitor and respond to the client’s experience of the therapy
3.4.1. An ability to decrease the likelihood that clients will become “overaroused” or overwhelmed (e.g. by becoming very anxious in response to the therapist’s interventions) by (a) monitoring the frequency and intensity of challenging interpretations; (b) negotiating a shared account of the client’s experience of the session; and (c) supporting the client’s adult self at the end of the session (e.g. through the therapist’s tone of voice)
3.4.2. An ability to ensure that the client has sufficient time to assimilate and respond to any interpretation (i.e. by not introducing new, unexplored themes in the last few minutes of a session)
3.5. Working with endings
3.5.1. An ability to prepare the client for ending by explicitly referring to the time limited nature of the therapy at the outset and throughout the therapy, as appropriate (e.g. in connection to a discussion about loss)
3.5.2. An ability to help the client express feelings about termination, including any disappointment with the limitations of the therapy and of the therapist
3.5.3. An ability to help the client make connections between their feelings about ending and other losses/separations
3.5.4. An ability to help the client review what they have learnt and gained during the therapy
3.5.5. An ability to formulate and construct a “good-bye letter” that accurately conveys the main interpersonal themes that have been worked on, as well as the ways of managing these problems, in a way that is positive, warm and personal
Specific Level 2 and 3 competencies in Cognitive Analytic Therapy
If you are using CAT, you must demonstrate the following competencies in order to reach Level 2 or 3 competence. These competencies have been adapted from the CAT section of the UCL CORE Competence framework for Personality Disorder.
Knowledge of CAT
1. Knowledge of CAT theory
1.1 An ability to draw on knowledge that CAT is an interpersonal (or relational) therapy that focuses on repeating patterns in relationships.
1.2 An ability to draw on knowledge that CAT is an integrative therapy that draws on different theoretical perspectives.
1.3 An ability to draw on knowledge that individuals are assumed to develop a repertoire of characteristic “reciprocal roles” which reflect their early formative experience, particularly in relation to caregivers, and that reciprocal roles can be enacted in relation to others (e.g. treating others in an abusive manner) and/or towards the self (e.g. treating the self abusively through self -neglect or self-harm).
1.4 An ability to draw on knowledge that CAT focuses on reciprocal role “procedures” (aim directed sequences of mental and behavioural processes, associated with affect, usually out of awareness and used as guidelines for action).
1.5 An ability to draw on knowledge that reciprocal role procedures (RRPs) which become problematic are often developed as a means of coping with or responding to the unbearable feelings or unmet needs associated with the RRs.
1.6 An ability to draw on knowledge that CAT entails working in collaboration with the client to help them revise problem procedures (i.e. the identification of “exits”), for example by:
- adopting an alternative course of action
- enacting more constructive RRPs in specific situations
- finding ways of addressing the unmet needs and unmanageable feelings associated with specific poles of the RRs
1.7 An ability to draw on knowledge that CAT identifies three main types of “problematic procedure”:
- “Dilemmas”: where the individual feels constrained to choose a course of action or mode of being which is artificially polarised between two alternatives
- “Traps”: where the individual believes that action will lead to negative outcomes, and proceeds to act in ways which fulfil their negative expectations, hence confirming the original negative belief
- “Snags”: – where the individual abandons a legitimate aim or goal because of an expectation that its fulfilment will lead to negative consequences for the self or others
1.8 An ability to draw on knowledge that CAT involves helping the client develop awareness of their procedures, and so be able to predict and consider making changes to them.
2. Knowledge of key features of CAT
2.1 An ability to draw on knowledge that CAT is an integrative therapy incorporating methods from:
- cognitive therapies
- analytic therapies
2.2 An ability to draw on knowledge that CAT is a time-limited therapy which emphasises the importance of ‘ending well’ by using the time-limit to address issues such as separation, mourning, and dependence/independence.
2.3 An ability to draw on knowledge that CAT interventions progress through three stages (‘reformulation’ ‘recognition’, and ‘revision’)
2.4 An ability to draw on knowledge that CAT is based on an explicit proactive and collaborative therapeutic style that stresses the active participation of both the client and the therapist
2.5 An ability to draw on knowledge that CAT aims to work within the client’s “Zone of Proximal Development” (ZPD), and that:
- therapy builds on that which the client can already do for themselves unaided and within the zone of those things which the client cannot yet do unaided, but can with the aid of ‘scaffolding’ provided by the active support of another
- therapy aims to extend the client’s zone of understanding and ability, so that they can subsequently manage without the support of the therapist in this area of functioning
3. The Psychotherapy File
3.1 An ability to draw on knowledge of the role of the Psychotherapy File in CAT assessments.
This has a number of aims:
- to communicate to the client that the focus of the therapeutic dialogue will be on repetitive coping patterns and assumptions rather than on symptoms alone
- to engage the client in a process of self-reflection
- to provide a preliminary identification of the role procedures (dilemmas, traps and snags) and self-states with which the client clearly identifies
- to alert the therapist to the extent to which the client experiences themselves and others in terms of “unstable states”
- to convey to the client that their problems are not unique to them but reflect patterns and experiences which are recognisable and amenable to therapy
4. Knowledge of the reformulation process
4.1 An ability to draw on knowledge that CAT involves the use of an explicit “reformulation”, created and shared with the client, and assumes that clients come to therapy with a ‘formulation’ (the framework of RRs and procedures which they use to understand and manage interpersonal relationships and themselves) which does not function effectively.
4.2 An ability to draw on knowledge that the early work of therapy entails generating a new formulation (a “re-formulation”):
- that validates the client’s story
- describes how these reciprocal roles and role procedures have been established in the person’s life and identifies their impacts
- considers the possibilities for change
4.3 An ability to draw on knowledge that the reformulation has several components:
- a “reformulation letter” written by the therapist and read out to the client, (which can be revised and modified on the basis of feedback from the client)
- a “sequential diagrammatic reformulation” ( SDR) or “map” which sets-out as simply as possible, the key reciprocal roles and problematic procedures which underpin the client’s current difficulties
- a list of “target problems” (TPs) based on a shared agreement between the client and the therapist.
5. Knowledge of the importance of the ending of therapy
5.1 An ability to draw on knowledge that the ending of therapy is a central focus from the beginning of therapy.
5.2 An ability to draw on knowledge that the ending of therapy is an opportunity to help the client work though feelings about previous, unresolved endings of relationships and to help them desist from reverting to patterns they have previously developed to deal with such situations.
Clinical Skills in CAT
1. Assessment
1.1 An ability to conduct an assessment, which covers aspects of history, experience, and presentation common to all therapies, and also attends particularly to maladaptive repeating patterns in relationships and self-management
1.2 An ability to attend to the client’s narrative, listening for recurrent relational themes, enacted or experienced in relation to a number of significant others
1.3 An ability to introduce CAT specific assessments such as The Psychotherapy File
2. Reformulation
2.1 An ability to arrive at a written (narrative) and diagrammatic reformulation early in therapy (usually by session 3-5) which may be amended or added to subsequently, but which will provide the initial focus for time-limited therapy.
2.3 An ability to read the letter to the client, attending to their immediate reaction, and responding to any cues
2.4 An ability to invite feedback to the letter and to foster the client’s “ownership” by showing a readiness to make factual changes or to amend wording or phrasing
3. Constructing the Sequential Diagrammatic Reformulation (SDR) (or “Map”)
3.1 An ability to construct a sequential diagrammatic reformulation, working with the client to map key RRs, role procedures, symptoms and self-states and the interrelationship between these
3.2 An ability to encourage the client to use the map as a reflective tool during and between sessions to help them understand patterns and identify changes
4. Constructing target problem procedures (TPPs or “key issues”)
4.1 An ability to formulate several key target problem procedures that are unique to the client, and draw on the client’s own words or phrases, and which:
- describe strategies that may have originally represented attempts to cope with or respond to painful RRs and states of mind, but which have become problematic.
- reflect the issues that the client endorses strongly in the Psychotherapy File
- describe the way the individual moves between RRs or discrete self-states mapped in the SDR
5. Formulating Aims or Exits
5.1 An ability to work collaboratively with the client to formulate “exits” to the TPPs which:
- draw on and name solutions which the client may already have started to discover to their difficulties, thereby endorsing their capabilities and strengthening their ownership of the exits
- when the client finds it hard to envisage any exits, offering them a range of possibilities and helping them select those which seem realistic and fitting for them
- offer manageable and realistic ways forward
6. Moving between task and process
6.1 An ability to move between working on the tasks of therapy and attending to relational process issues
6.2 An ability to recognise when a process issue arises and to judge whether it would be useful to engage the client in reflection on this at that point in time
6.3 An ability to recognise that the task-oriented aspects of CAT are likely to evoke reactions in the client which are characteristic of the client’s particular RRs
6.4 An ability to make links between the client’s “process” responses and the formulation.
7. CAT methods of intervention
7.1 An ability to use CAT methods in the post-reformulation phase of therapy to help the client: recognise unhelpful RRPs and consider how these can be revised (i.e. experimenting with more constructive alternatives), for example by working with the client to agree on the best way of supporting self-monitoring, including CAT monitoring sheets or a diary
7.2 An ability to observe the way in which unhelpful RRPs identified in the reformulation are enacted within the therapeutic relationship, and drawing the client’s attention to this in an uncritical way that fosters self-awareness and reflection and allows revision of those procedures
7.3 An ability to reflect on the therapist’s own response to the client as a useful source of information about the procedures that may be salient in this particular client
7.2 An ability to draw on knowledge that the revision stage of CAT involves the client beginning to try alternative ways of relating to self, others and situations in order to develop exits to their patterns that lead to new learning and positive change.
7.3 An ability to use CAT as a framework within which to draw on a range of psychological approaches, for example psychodynamic, behavioural, cognitive-behavioural, gestalt, in order to employ therapeutic strategies which help the client to experience new learning and positive change
8. Ability to use CAT skills to manage the ending of therapy
8.1 An ability to address the ending in a planned, explicit and contained way, including regularly reminding the client about the number of remaining sessions, and inviting them to express a range of feelings about the ending and the time-limited nature of the therapy.
8.2 An ability to use “goodbye letters” with the client.
8.3 An ability to plan any follow up sessions as appropriate to the client and the service context.
Source: Ryle, A. and Kerr, I. B. (2002) Introducing Cognitive Analytic Therapy. Principles and Practice. Chichester: Wiley.
Specific Level 2 and 3 Competencies in Other Brief Psychodynamic Therapies
If you are using a different psychodynamic approach to PIT or CAT, you must demonstrate the specific competencies below in order to meet Level 2 or 3 competence. These competencies have been derived from the basic analytic/dynamic competencies in the UCL CORE competencies framework for psychoanalytic/psychodynamic therapies produced by Lemma, Roth and Pilling.
N.B. Further information about each of these competencies can be obtained by clicking on the relevant links in purple. Please note that the exact manifestation and application of each competence is likely to vary according to the specific psychodynamic approach being used. It is therefore up to the supervisor to use their judgement to determine whether each of the competencies has been met for the model in question, using the detailed information in the Lemma, Roth and Pilling framework as a guide only.
- An ability to undertake an assessment of likely suitability for analytic/dynamic therapy.
- An ability to engage the client in analytic/dynamic therapy.
- An ability to derive an analytic/dynamic formulation.
- An ability to establish and manage the therapeutic frame and boundaries.
- An ability to help the client explore the unconscious dynamics influencing their relationships.
- An ability to help the client become aware of unexpressed or unconscious feelings.
- An ability to maintain an analytic/dynamic focus.
- An ability to identify and respond to difficulties in the therapeutic relationship.
- An ability to work with the client’s internal and external reality.
- Ability to work through the termination phase of therapy.
Systemic Therapy Competence Framework
We aim to support trainees to develop competencies required to deliver effective systemic therapies as set out by Roth, Pilling and Stratton (2009) in the UCL Competence Framework. Opportunities to develop such competencies are provided via formal teaching, placements, assessments and wider learning experiences. Trainees will learn how to adapt systemic theory and practice to best meet the need of systems and/or their clients across the life span whilst still maintaining fidelity to evidence based models.
Reflective Practice Group (RPG) sessions are also designed to help you develop competence in working reflexively, which is a central component of working from a systemic approach. Each RPG sets its own ground rules and focus, and offer an opportunity to explore ‘who you are’ and what this means for your role as a clinical psychologist. There is support to reflect ‘in’ as well as ‘on’ action in terms of your evolving role within the group. Trainees gain valuable experience of being in a group, and making sense of, and managing, group dynamics (an increasingly key role post-qualification). Trainees are also encouraged to further reflect and consolidate their learning during RPGs, through the use of several helpful references to ground this wider learning in a systemic approach.
Levels of Systemic Therapy competence
All trainees are expected to demonstrate Level 1 competence in systemic therapy and may go on to demonstrate Level 2 or 3 competence if the required clinical work is completed.
Level 1 competence
As with all of the other core therapeutic approaches on the Manchester ClinPsyD, Level 1 competence in systemic therapy consists of basic knowledge about, and the ability to formulate using, this model. Competence at this level will primarily be delivered through the Systemic and Family Therapy module of the academic curriculum, although the Child module also provides a timely introduction to systemic thinking and ways of working with children and families. There are also a significant number of additional lectures that make reference to systemic theories and intervention throughout the three years of training. Competence at this level will be evaluated in the Child exam in Year 1.
Level 2 competence
Competence at this level requires competent use of systemic therapy as a standalone approach with at least four clients, of which two must have been observed (either “live” or via audio/video recording) by the placement supervisor. These cases can be seen on any placement as long as they are supervised by a clinician who identifies themselves as competent to deliver and supervise systemic work.
Level 3 competence
This level of competence requires significant experience using systemic therapy as a standalone model and will enable students graduating at this level to use the model clinically when they qualify, assuming (as for all therapeutic models) the availability of appropriate supervision. Competence at this level requires:
- a specialist third year placement in systemic therapy under a systemic competent supervisor providing regular supervision in the approach;
- competent use of systemic therapy as a standalone approach with at least eight clients, of which at least three must have been observed (either “live” or via audio/video recording) by the placement supervisor, using a professionally recognised and reputable session rating scale where possible;
Trainees at this level should also aspire to demonstrate all of the basic and specific systemic competencies and meta-competences described below.
Supervisors should be regularly reviewing trainees’ clinical work in session or via recordings (when appropriate). To assess Level 3 competencies, supervisors should ideally review a video clip of a one hour session and three further 10 minute clips using a reputable session rating scale.
Specific systemic competences
The individual competencies listed below are part of the UCL competence framework in systemic therapy and have been reproduced verbatim in most cases. Click on the individual items in purple for further information about the elements of that competence. When completing the Clinical Portfolio, trainees and supervisors should refer to the content of each item to judge whether the overarching competence was demonstrated whilst on placement. There is no expectation that each of the individual elements within a competence will be “ticked off”, however, and the Portfolio is therefore not designed with this in mind. The Supervisor Assessment of Trainee form will also be used to evaluate competencies at Levels 2 and 3.
A. Basic Systemic Competencies
A1. Knowledge of the rationale for the systemic approach:
A1.1. Knowledge of systemic principles that inform the therapeutic approach
A1.2. Knowledge of systemic theories of psychological problems, resilience and change
A1.3. Knowledge of the systemic approaches that enable therapeutic change
A2. Ability to initiate and undertake a systemic intervention:
A2.1. Ability to initiate and undertake a systemic assessment
A2.3. Ability to develop systemic formulations and help the client(s) identify appropriate goals
A2.4. Ability to establish the context for a systemic intervention
A3. Ability to maintain and develop a systemic approach:
A3.1. Ability to work in a reflexive manner
A3.2. Ability to use monitoring to promote change
A3.3. Ability to facilitate communication across the system
A3.4. Ability to manage endings
B. Specific Systemic Competencies
B1. Ability to use systemic hypotheses
B2. Ability to use circular interviewing
B3. An ability to use systemic techniques to promote change
B4. An ability to work towards resolving problems
B6. An ability to make use of enactments
B7. Ability to work with a systemic team
C. Problem Specific Systemic Competencies
C1. Systemic Couples Therapy for Depression (Jones & Asen)
C2. Eating Disorders (Lock and Eisler)
C3. Interventions for conduct disorder and related problems:
C3.1. Multi-Systemic Therapy (MST; Henggeler)
C3.2. Multidimensional Family Therapy (Liddle)
C3.3. Brief Strategic Family Therapy (BSFT; Szapocznik et al)
C3.4. Functional Family Therapy (FFT)
D. Systemic-specific Metacompetencies
D1. Ability to make use of the interpersonal perspective
D2. Ability to hold a non-pathologising view of the system
D3. Ability to maintain a relational approach
D4. Ability to implement systemic interventions in an adaptive manner
Clinical Neuropsychology competence Framework
Division of Neuropsychology (DoN) standards and competencies
The competency framework set out below represents an attempt to benchmark the Manchester ClinPsyD against the British Psychological Society Division of Neuropsychology (DoN) standards and competencies for the Qualification in Clinical Neuropsychology (QiCN). We adopted this framework as one of our four core intervention models to ensure that all trainees attain generic and measurable competency in neuropsychology in the first two years of the programme. There is also a third-year option of an advanced level of competence for trainees who wish to pursue qualification in clinical neuropsychology subsequent to clinical psychology training.
The QiCN is currently the gold standard for training in clinical neuropsychology within the UK, conferring eligibility for Full Membership of the DoN and entry to the Society’s Specialist Register of Clinical Neuropsychologists (SRCN). The DoN concluded a consultation on changes to the QiCN in 2014. A new “stages of training” approach was well received, along with a proposed ‘fast-track’ route. According to this approach, clinical psychology trainees who can evidence having already gained neuropsychology skills to a certain level should be able to have this learning accredited as part of the QiCN, meaning that they can complete the qualification in less time than the current two years.
The University of Bristol and North Bristol NHS Trust’s Diploma in Theoretical and Practical Neuropsychology has been designed to allow trainees to bring forward learning and case experience from the ClinPsyD to reduce the post-doctoral Clinical Neuropsychology training required to enter the SRCN. The Manchester ClinPsyD has linked with Bristol to facilitate this pathway for trainees who intend to go on to train as Clinical Neuropsychologists (see Levels of Clinical Neuropsychology competence on the Manchester ClinPsyD section below).
The stages of training approach recognises the following foundation stages and components leading to attainment of the QiCN competencies:
Levels of Clinical Neuropsychology competence on the Manchester ClinPsyD
The Manchester ClinPsyD distinguishes between three levels of competence in relation to clinical neuropsychology, which map onto different levels and aspects of the competencies specified within the QiCN framework. As of September 2016, negotiations are underway with the DoN over whether Accreditation of Prior Learning (APL) credits for the QiCN can be conferred for these levels.
Level 1 competence: Relevant knowledge (subsuming QiCN Level 1A)
Generic (clinical, educational or other transferable) skills are foundational for neuropsychologists, and are currently developed by undertaking either a Doctorate in Clinical or Educational Psychology. As such, all trainees will be expected to demonstrate QiCN Level 1A equivalent competencies during Years 1 and 2 of the ClinPsyD (see below for a full set of competencies), which will include dedicated teaching on Clinical Neuropsychology. Knowledge at this level will be assessed via the Clinical Neuropsychology written examination in Year 2. Further information about this exam will be made available to trainees in due course and no less than three months before it takes place.
Level 2 competence: Relevant practice
The QiCN Practice dimension requires students to obtain clinical experience within neuropsychology, consisting of six relevant cases. The requirement for Level 2 competence in Clinical Neuropsychology on the Manchester Programme is therefore supervised experience working with six clinical cases on placement where competent neuropsychological assessment and formulation is a central component of the work. At least two of the cases must have been observed (either “live” or via recording) by the supervisor. Cases can be seen on any placement and there is no expectation that the supervisor is a qualified Clinical Neuropsychologist, although they must identify themselves as competent to supervise and “sign off” the work as a valid Clinical Neuropsychology case in order for it to count towards Level 2 competence. This should be discussed with supervisors when the placement contract is being agreed. It is our expectation that all trainees will be able to reach Level 2 competence in Clinical Neuropsychology by the end of Year 2. Clinical Tutors will discuss your progress towards the different competences in mid and end of placement visits so that appropriate learning opportunities can be identified.
Both the adult and paediatric QiCN require experience with a range of cases, to demonstrate competency across conditions. In the adult form, it is strongly recommended that candidates include at least one case of Traumatic Brain Injury (TBI), one focal cerebrovascular accident (CVA) and one degenerative disorder. In the paediatric form, there should be at least one case each of TBI, epilepsy and congenital disorder. A list of disorders that fall into the above categories is provided in the QiCN syllabus. For both adult and paediatric QiCN, it is recommended that the purpose of the intervention is primarily diagnostic in at least two cases and rehabilitation/treatment/remedial (involving family and/or educational establishment in child work) focused. For the purposes of the ClinPsyD, there is no requirement that trainees work with specific ages or types of cases in order to reach Level 2 competence, although a range of presentations and types of clinical work is nevertheless expected. Moreover, the choice of cases is likely to have implications for any accreditation of prior learning on the QiCN, according to whether adult or paediatric qualification is being pursued.
Level 3 competence: Advanced neuropsychology knowledge and practice
In order to reach Level 3 competence in any of the four main approaches on the Manchester ClinPsyD, trainees must undertake a specialist placement in that approach in Year 3. For Clinical Neuropsychology, Level 3 competence requires a specialist placement under the supervision of a qualified Clinical Neuropsychologist, with at least eight clinical neuropsychology cases being completed competently in that setting. At least three clinical cases must have been observed directly (either “live” or in a recording) by the supervisor.
Experience with a variety of different types of presentation and clinical work is required, although there are no specific rules about which presentations and types of work are necessary to reach the required level. Nevertheless, trainees who are interested in bringing forward case experience to be considered for the practice dimension of Bristol’s Diploma in Theoretical and Practical Neuropsychology should be aware of the kinds of cases and clinical work that the DoN would consider relevant for completion of the practice component of the QiCN (see Level 2 competence section above). To be eligible for the Diploma, trainees must have at least 6 months placement experience and one case written up to DoN case report standard (4000 words).
With respect to bringing learning forward for the Bristol Diploma, Level 3 competence will also require registering for and accessing additional online teaching material provided by Bristol. The additional teaching covers the content of The Applied Clinical Neuropsychology and Principles of Neuropsychological Assessment unit of the Diploma and is assessed by an entrance examination and entrance essay administered by Bristol. If these assessments are passed the trainee would be exempt from 25 % of the knowledge dimension of the Diploma. This supplementary content is separate to Manchester’s Clinical Neuropsychology curriculum. While there is some overlap, the additional training required would be expected to add considerably to a trainee’s workload in year three. We would therefore expect trainees wishing to pursue the ‘Bristol route’ to consider this carefully and discuss this with the Manchester programme’s Clinical Neuropsychology module organiser. If it is agreed to be a viable option then the trainee can submit an expression of interest to study at the University of Bristol, which is authorised by the ClinPsyD’s Programme Director.
Level 3 competence would be expected to streamline the post-doctoral process for those on the ClinPsyD that are sure they want to qualify as Clinical Neuropsychologists subsequently. Of course not attaining Level 3 three competence would not preclude a trainee from deciding to pursue post-doctoral Clinical Neuropsychology training after qualifying. Trainees might also prefer the Glasgow training, which does not allow ClinPsyD learning to be brought forward as approved prior learning. Again these options can always be discussed with the Clinical Neuropsychology module organiser.
In the future, we anticipate that Level 3 competence will also require attendance at additional teaching on the topic in question. For Clinical Neuropsychology, we expect that teaching to be mapped onto some aspects of QiCN Level 1B (Advanced Psychometric and Cognitive Assessment Skills). An additional summative assessment may also be introduced at this level. Further information about this will be provided as it becomes available.
Specific Clinical Neuropsychology competencies
Below is a list of the specific competencies from the DoN framework that will be assessed on the Manchester ClinPsyD.
A. Generic clinical competencies
It is expected that all trainees will acquire and demonstrate the following generic clinical competences across the clinical, academic and research components of the programme.
A1. Underpinning knowledge and skills: With reference to theory and empirical evidence, synthesise complex relevant information within a clinical supervisory, or research context.
A2. Clinical work: Demonstrate effective interpersonal, assessment, formulation and intervention skills with individuals, teams and systems. Demonstrate appropriate links between assessment, formulation and intervention.
A3. Communication: Demonstrate effective communication in teaching, training, consultancy and broader professional practice.
A4. Personal and professional practice: To understand psychological processes in a broad professional context and use such understanding in collaborative strategic aspects of client work and service delivery.
B. Specific neuropsychological competencies
Underpinning knowledge and skills: Knowledge of clinical neuropsychology and its theoretical foundations, clinical application and relationship with related aspects of clinical psychology, neuroscience and other related disciplines.
Clinical Neuropsychology knowledge constitutes a key component of Level 1 competence on the programme. Much of this material will be taught in the Clinical Neuropsychology module and assessed in the corresponding written exam in Year 2, although a greater depth and breadth of knowledge will be expected at Levels 2 and 3.
The competencies in this area include knowledge of:
B1. fundamental principles underpinning neuroscience (and developmental cognitive neuroscience)
B2.normal ageing, brain pathology/injury and neurological recovery
B3: terminology, methodologies and paradigms relevant to the study of developmental brain/behaviour relationships
B4: conceptual approaches adopted in clinical neuropsychology and their historical foundations
B5: major theories of brain/behaviour development and how they inform approaches to neuropsychological assessment and interpretation of data
B6: contemporary theories of brain/behaviour relationships and their implications for clinical practice
B7: major theories of normal cognitive learning and brain development
B8: the relationship between underlying neuropathology and cognitive outcome
B9: psychometric and statistical principles
B10: specialist assessment for infants and children at risk of developmental delay
C. Clinical work: Utilise neuropsychological knowledge and experience in the delivery of assessment, formulation and intervention.
As the competencies in this and the sections on communication and personal and professional practice are inherent to all neuropsychological work it is not possible to distinguish between those that are specifically relevant to Levels 2 and 3 competence. Nevertheless, it is expected that trainees undertaking a specialist placement in Clinical Neuropsychology will take on more complex and challenging cases, allowing for a greater depth of knowledge and skill to develop at Level 3.
Where neuropsychology cases have been seen on placement, you and your supervisor will be asked to indicate whether you have demonstrated an ability to:
C1: understand the social, psychological, cognitive and educational/vocational impact of acquired brain injury and neurological conditions both for individuals and systems
C2: identify cognitive impairment, behavioural changes and emotional difficulties and provide integrated psychological/neuropsychological approaches to manage these
C3: use behavioural observations and to map them to possible neurological, cognitive or emotional underpinnings
C4: perform clinical assessment including history taking, bedside cognitive assessment and mental status examinations and carrying this through to management
C5: tailor neuropsychological assessment to clients, including children/young people, and to address appropriate questions
C6: select, administer and interpret a wide range of assessment instruments and be familiar with these
C7: understand of (and administer) neurodevelopmental assessment batteries and how these differ from neuropsychological measures
C8: understand of and administer the tools used to assess different components of cognition and behaviour
C9: understand psychometric principles underpinning cognitive testing, including cognitive change during development, and use these principles in the interpretation of assessment results
C10: describe the range of factors that could affect performance on neuropsychological/neurodevelopmental tests
C11: integrate neuropsychological data with measures of brain function to improve diagnosis and prognosis
C12: construct formulations about the client’s neuropsychological status by the deductive application of appropriate test instruments in the course of a broader investigation
C13: produce neuropsychological formulations that reflect the complex range of variables involved in pediatric clinical cases
C14: show knowledge regarding the neuropsychological profiles associated with a range of common neurological, neurodevelopmental and neuropsychiatric disorders
C15: use neuropsychological formulations dynamically to facilitate a client’s, including a child’s or young person’s, understanding and adjustment, and to plan interventions if required, coupled with the ability to revise formulations
C16: use formulation, and devise and deliver evidence based and tailored neuropsychological interventions, which are individually tailored to the client/child/young person/family
C17: adapt models of therapeutic intervention for psychological difficulty in the context of impaired cognitive functioning and developmental age
C18: implement psychological interventions appropriate to the presenting ‘neuropsychological’ difficulty and to the psychological and social circumstances of the client(s)
C19: demonstrate applied understanding of neurological recovery and neuropsychological rehabilitation
C20: apply principles of management and rehabilitation of neuropsychological/neurological disorders
C21: use up to date knowledge and understand the treatment approaches and management of a range of common neuropsychological, neurological, neuropsychiatric, developmental, and acquired conditions
C22: understand the role of clinical neuropsychology in adult and child mental health services
C23: demonstrate knowledge of methods of reintegration into the educational system after acquired brain injury and work with support staff, teachers, parents and children to support this process
C24: understand the relationship between patterns of cognitive function and appropriate learning intervention
C25: understand the relationship between cognitive impairment and educational progress and attainment
C26: demonstrate knowledge of specialist settings for acute or long term support for children with neuropsychological difficulties
D. Communication: Utilise neuropsychological knowledge and experience in communication with clients and professional colleagues
Where neuropsychology cases have been seen on placement, you and your supervisor will be asked to indicate whether you have demonstrated an ability to:
D1: communicate neuropsychological hypotheses and conclusions clearly and effectively to specialist and non-specialist audiences
D2: adapt style of communication to people with a wide range of neuropsychological disorders with differing levels of cognitive ability, sensory acuity and modes of communication, including children and young people of different developmental ages
D3: communicate effectively clinical and non- clinical information from a neuropsychological perspective in a style appropriate to a variety of different audiences
D4: provide feedback to clients/systems (including parents/caregivers, in the case of children and young people) clearly and sensitively
D5: understand the process of providing expert neuropsychological opinion and advice, including the preparation and presentation of evidence in formal settings
D6: supporting others’ learning in the application of neuropsychological skills, knowledge, practices and procedures
D7: engage and communicate with assistant psychologists in supervising the effective use of psychometric assessment tools and techniques, behavioural observation and elementary rehabilitation
D8: use neuropsychological formulations to assist multi-professional communication and understanding
D9: accommodate additional medical information from various sources
E. Personal and professional practice: Refer to and make use of contextual legislative and organisational aspects of neuropsychology practice.
Where neuropsychology cases have been seen on placement, you and your supervisor will be asked to indicate whether you have demonstrated knowledge of:
E1: formal documents in relation to ethical principles of practice, legal and statutory obligations and general professional standards as applied to clinical neuropsychology practice
E2: the political and organisational context of health care delivery as it relates to neuropsychological clients, as well as relevant aspects of NHS and social services procedures
E3: health and educational policies that are relevant to children and young people who have developmental learning difficulties, acquired brain injuries or neurological conditions
E4: the differing roles and requirements for neuropsychology and child neuropsychology in a range of professional settings and contexts
E5: general professional issues, and developments in professional arrangements and practice within a national and international context
Research
Introduction to research on the Manchester ClinPsyD Programme
This section provides information on the research elements of the Manchester ClinPsyD Programme, which are designed to ensure that trainees develop required competencies in conducting and evaluating clinically relevant research. It describes the types of research required as part of the Programme, as well as the teaching and support available for trainees and how these are assessed.
As a ClinPsyD researcher you are registered within the Division of Psychology and Mental Health in the School of Health Sciences, within the Faculty of Biology, Medicine and Health. The Doctoral Academy oversees postgraduate research degrees within the Faculty and can provide advice, support, training opportunities and information about the wider researcher community.
Further information about the Doctoral Academy, as well as links to Facebook, Twitter and up-to-date blogs, can be found at:
https://www.bmh.manchester.ac.uk/doctoral-academy/
Research in clinical psychology is a central part of professional practice. Evidence-based clinical practice is an established foundation of the professional ethos of the National Health Service. As practising clinical psychologists, we are expected to keep ourselves appraised of the most recent and relevant scientific research and to be in a position to evaluate published research reports. Through our training we gain skills not only as critical consumers of research, but we are also expected to contribute to this knowledge base through carrying out research at doctoral level. The British Psychological Society (BPS) sets the standards for doctoral programmes in Clinical Psychology (May 2014) and provide guidance for research and research methods (2017); thus, trainees are expected to meet the following five competencies in research:
- Being a critical and effective consumer, interpreter and disseminator of the research evidence base relevant to clinical psychology practice and that of psychological services and interventions more widely. Utilising such research to influence and inform the practice of self and others.
- Conceptualising, designing and conducting independent, original and translational research of a quality to satisfy peer review, contribute to the knowledge base of the discipline, and merit publication including a) identifying research questions, b) demonstrating an understanding of ethical issues, c) choosing appropriate research methods and analysis (both quantitative and qualitative), d) reporting outcomes and e) identifying appropriate pathways for dissemination.
- Understanding the need and value of undertaking translational (applied and applicable) clinical research post-qualification, contributing substantially to the development of theory and practice in clinical psychology.
- The capacity to conduct service evaluation, small N, pilot and feasibility studies and other relevant research which is consistent with the values of both evidence based practice and practice based evidence.
- Conducting research in respectful collaboration with others (e.g. service users, supervisors, other disciplines and collaborators, funders, community groups, etc.) and within the ethical and governance frameworks of the BPS, the Division of Clinical Psychology, HCPC, universities and other statutory regulators as appropriate.
In order to deliver this element of clinical training, trainees will undertake and submit three mandatory pieces of work:
- One formally assessed Audit of Clinical Activity (ACA)
- One Service Related Project (SRP) whilst on clinical placement.
- An independent, doctoral-level, Large Scale Research Project (LSRP) that requires them to conceptualise, design, carry out and communicate the results of research that is relevant to clinical psychology theory and practice.
Trainees are supported in their learning in the following ways:
- Formal training in research ethics and governance (online Good Clinical Practice course, completed in
Year 1) - Lectures which are part of the Research Methods module (mostly delivered in Year 1)
- Lectures which are part of the Statistics module (mostly delivered in Year 2)
- Undertaking programmatic research in which all trainees, without exception, undertake their LSRP in an area of research initiated and overseen by academic supervisors with relevant research and expertise within the University of Manchester’s School of Health Sciences
- Undertaking their LSRP under the supervision of at least one clinical psychologist who is part of their supervisory team
Aims of the research element of the Manchester ClinPsyD Programme
The aims of the research element of the Manchester ClinPsyD Programme are to:
- Develop competence in clinically relevant psychological research, adopting a broad scientific approach.
- Enable trainees to critically assess scientific documents with clarity and rigour.
- Practise a range of research skills including critical assessment and conduct of research in a variety of settings.
Intended learning outcomes of the research element of the Manchester ClinPsyD Programme
After completing the Manchester ClinPsyD Programme, trainees will:
- Be able to plan research investigations in a variety of settings, and to use a range of research methodologies.
- Be familiar with specific research tools, including information sources and databases, tests and measures, statistical procedures and referencing support services.
- Be able to complete an independent research project, including writing and modifying a proposal, gaining ethical committee approval, preparation and data collection, analysis and writing-up.
- Be able to disseminate their research work via publication in academic peer-reviewed journals and/or at relevant conferences .
More detailed aims and objectives for each lecture in the Research Methods module are detailed in the Academic Curriculum, which is available on the programme intranet/Canvas.
The large-scale research project facilitates the trainee’s progression through all stages of the process of independent research, from an initial idea through to final submission. Trainees learn to select feasible ideas to evaluate through the programmatic research process of the Manchester ClinPsyD Programme (see Hare & Wittkowski, February 2015). For example, psychologists and affiliated research-active clinicians provide summaries of their current research and potential trainee research projects which are presented in the form of a research project booklet to Year 1 trainees, so that they can identify an appropriate supervisor and research area of interest to them. The research project ideas presented in the research project booklet in Year 1 will have been pre-screened by the Research Director predominantly with a focus upon feasibility and suitability for a ClinPsyD trainee LSRP. Each trainee has two academic supervisors (one will serve as the main supervisor and the other as the co-supervisor) and often a field or external supervisor for their project (see University of Manchester’s supervision policy for postgraduate research degrees). Research will normally take place at the University or an NHS provider setting within the North West.
The process by which trainees select projects and the process by which projects are allocated are outlined in detail in documents on the intranet/canvas under research downloads. The Manchester ClinPsyD programme offers programmatic research which means that academic staff only supervise projects within their own areas of expertise. Although it might not be possible to accommodate a trainee’s preferred topic area, ensuring that supervisors are experts within the area helps to ensure the quality of the supervision provided and the outputs of the work.
Trainees submit a formal proposal of their planned study (see timetable below for further details). Through the Research Sub-Committee process, trainees may be instructed to further develop and refine their ideas. Submitting an ethics application provides further practical learning. All stages of the research enhance the skills of the independent researcher. Statistical analysis consolidates the formal teaching, and trainees may learn new statistical approaches at this stage. There are opportunities to carry out projects using quantitative or qualitative methods which are supported by formal teaching and supervision in line with BPS guidance for research and research methods (2017). Formal academic writing skills are developed through discussion of drafts. Research leave days are designated for trainees to undertake their LRSP which must be presented for oral examination in the form of a typed and bound thesis. As part of their thesis, trainees are expected to produce a literature review as well as an empirical study paper of publishable standard and they are encouraged to disseminate their findings (see timetable below for details).
Depending on their workload, trainees can negotiate up to one half day per week on placement with their supervisors to undertake their audit of clinical activity (ACA) and their service related project (SRP). It is required that these activities take place on the site of the trainee’s current clinical placement and as such are placement-based activities. Within one of the first four placements (i.e. during Year 1 to Year 2 of training), trainees must carry out an ACA based on their work within that placement. The service related project (SRP) focuses on service development and will be carried out during the trainee’s final placement in Year 3. In designing the ACA and SRP on placement, trainees learn the practicalities of applying their research skills to real problems or clinical needs in NHS-based settings. In this context, there is an emphasis on close supervision by an experienced practitioner and learning through directly supervised, collaborative work whilst on placement. For this reason, supervision of ACAs and SRPs is not regulated by the policy on programmatic research, but negotiated by trainee and placement provider. The ACA report and the SRP report must be presented for examination in a manner designated by the Programme organisers; please see the audit and service related project sections for more information.
Research Methods Teaching
The Research Methods module extends across all three years of the programme but is primarily delivered within the first year. It has three main aims:
- To provide support for the completion of the large-scale research project (LSRP)
- To provide support for the completion of the audit of clinical activity (ACA) and the service related project (SRP)
- To facilitate the development of competencies in clinical research
Format of Research Methods sessions across the years
| Type | Title | Duration | Year |
| Procedural Research Information | Introduction to the Research Methods Module | 1 hour | Year 1 |
| Procedural Research Information | Introduction to Research Governance | 1 ½ hours | Year 1 |
| Procedural Research Information | Research Governance: Good Clinical Practice (online training course) | 3 hours | Year 1 |
| Procedural Research Information | Introduction to the Audit of Clinical Activity (ACA) and the Service-Related Project (SRP) | 1 hour | Year 1 |
| Procedural Research Information | Using e-Resources for Research | ½ hour | Year 1 |
| Procedural Research Information | Selecting a Supervisor and Method | 1 hour | Year 1 |
| Procedural Research Information | Preparing the Large Scale Research Project Proforma (LSRP) | 1 ½ hours | Year 1 |
| Procedural Research Information | LSRP Public and Patient Involvement (PPI) | 2 hours | Year 1 |
| Procedural Research Information | Clinical Liaison Group (CLG) Consultation Sessions | Individual sessions are arranged | Year 1 |
| Procedural Research Information | Survive a viva | 1 hour | Year 3 |
| Procedural Research Information | ClinPsyD Thesis Presentation | 1 hour | Year 3 |
| Reviewing the Literature | Introduction to Reviewing the Literature | 3 hours | Year 1 |
| Reviewing the Literature | Meta-synthesis (including quality appraisal) | 2 hours | Year 1 |
| Reviewing the Literature | Meta-analysis | 2 hours | Year 1 |
| Reviewing the Literature | Appraising the Literature | 1 hour | Year 2 |
| Specific Methods and Designs | Qualitative Research Methods | 12 hours | Year 1 |
| Specific Methods and Designs | Evaluation of Treatments | 1 hour | Year 1 |
| Specific Methods and Designs | Quasi-experimental Designs | 1 hour | Year 1 |
| Specific Methods and Designs | Experimental Designs and Analogue Sampling | 1 hour | Year 1 |
| Specific Methods and Designs | Longitudinal Designs | 1 hour | Year 1 |
| Specific Methods and Designs | Small N Designs | 1 hour | Year 1 |
| Specific Methods and Designs | Questionnaire Design | 2 hours | Year 1 |
| Specific Methods and Designs | Q Methodology and Repertory Grid Technique | 1 hour | Year 1 |
| Specific Methods and Designs | Experience Sampling Methodologies: Applications for Mental Health Research | 1 hour | Year 1 |
LSRP: Supervisory support for Research
Research supervision
Once you have been allocated to a project/supervisor you should arrange to meet them as soon as possible. The initial priority is the completion of the Research Contract, where expectations of the roles of trainee and supervisor(s) as well as the supervision process can be explicitly discussed and agreed.
As stated in the Research Contract, you will receive a minimum of 1 contact hour per month from your supervisor(s). It may be typical to meet with your supervisory team more frequently at first and then, once the project is designed and progress is well under way, you may decide to meet less frequently. This frequency would be decided by yourself and your supervisor(s). Some supervisors may agree to alternative methods of contact on occasions where a face to face meeting is difficult to schedule (e.g. a skype/zoom or telephone call). The initiative for requesting supervision meetings lies entirely with you.
Working with a supervisor is an important element of the research process. Supervision is provided under the general principle that the thesis must be the trainee’s own work. Guidance and discussion throughout the supervisory process will enable you to develop and present your work effectively and in accord with expectations of doctoral research. Your supervisor will provide you with the necessary support (e.g., conceptual design, methodological issues, statistical advice) or direct you to an appropriate member of staff if there are issues outside their expertise (see LSRP: Technical and Statistical Support for Research section)
In line with the University’s Postgraduate Research (PGR) guidance, trainees should have more than one academic within their supervisory team, with one academic designated the primary supervisor. Your primary supervisor will usually be responsible for reading through drafts of your LSRP proposal, commenting on your research ethics application, and providing feedback on your thesis papers.
The supervisor’s role is to give advice and help on the nature and standard of the work, and direct you to useful literature and appropriate methodology. But remember, the ultimate responsibility for the LSRP project remains yours. It is not the supervisor’s responsibility if you fail to attend meetings or miss deadlines. This is part of your training in project management and managing the ‘research process’. Your supervisor will guide you through the research process and may agree deadlines for sharing draft work with you. Make sure you do not miss these deadlines and take heed of the feedback
Review of drafts
To ensure consistency and fairness across trainees, we have strict guidelines on the number of occasions when feedback can be provided by supervisor(s). These guidelines are also detailed within the Research Contract. Your supervisor will be limited to offering comments as follows:
- No more than two drafts of your review paper
- No more than two drafts of your empirical paper
- No more than one draft of your critical appraisal / reflective paper
Your supervisor will be limited to providing comments on each section of the thesis papers as they are completed OR to providing overall comments on the full draft of each paper. This should be agreed with your supervisor in advance.
Where there are two or more supervisors the draft papers may only be read once by one supervisor. This will normally be the primary supervisor. It would be acceptable to ask for a secondary supervisor to look at some sections (for example if the second supervisor has methodological expertise that the first does not, then you may ask them to look at the methods) but each section must be looked at only once and your primary supervisor could no longer comment on this section within the current draft. As such, you should decide, along with your supervisors, which supervisor will provide feedback on which sections for each draft of each paper.
Be mindful that most supervisors have multiple trainees and a variety of other commitments and will need to book time in their diaries to review your drafts. If you send your draft after the agreed draft submission deadline then you may find that your supervisor does not have adequate time to look at it, or you will not have sufficient time to incorporate the suggested changes. This will not be considered grounds for an extension.
Writing style
When writing drafts of your papers, pay particular attention to the grammar and style remembering, for example, to use the past passive voice for most statements. It would be helpful to phrase your aims, objectives and plans in the past tense rather than the future – this will allow you to re-use the text for your final thesis papers without having to change all of the tenses. You may find it helpful to look at previous ClinPsyD theses to get an idea on style, length etc. A useful technique to aid good writing skills is to read your written work out aloud: this will help you to identify poor grammar and muddled sentences.
Supervisors are not to be expected to proof read or to correct spelling/grammar. Trainees remain responsible for ensuring their work has been appropriately proof read and spelling/grammar corrected prior to seeking feedback from supervisors. Even if your supervisor reads your entire thesis and you make the suggested changes, this is no guarantee that it is of a ‘pass’ standard; the work is yours and its quality is dependent on your output.
Supervision meetings
You should seek to arrange supervision meetings via prior appointment. There will be periods when your supervisor is not available, either because they are heavily committed with other duties such as examining, clinics, research, lecture preparation, administrative work and writing commitments. You are therefore advised to agree methods of getting in contact with your supervisor: email is usually the best way. Supervision meetings should always be prearranged: never expect on-the-spot supervision. Make sure that you and your supervisor are aware of each other’s periods of absence.
Your supervisor will likely be involved with a variety of other projects; therefore, you should not assume that they will immediately recall the last discussion you had together about your project. It would be good practice for you to prepare an agenda for each supervisory meeting (a short list of points you would like to discuss) and take minutes of the meeting (brief notes on what was discussed or decided and any action points for you and or your supervisor). Reviewing the minutes will help your supervisor and yourself recall what was discussed at the previous meeting. Minutes of supervisory meetings should be uploaded to your Research Study Master File on the trainee intranet.
Reflective Journal
You are also advised to keep a ‘logbook’ or ‘reflective journal’ throughout the duration of your research project so that you keep a record of all discussions with your supervisor. This should document all aspects of work, and specifically the decisions made (e.g. why one methodology was chosen over another). You will be surprised how many of the finer details of your study become difficult to recollect by the time you are writing up your thesis and so having a single place for future reference can be a good idea.
LSRP: Timetable
The table below presents an overview of the various steps involved in developing and conducting the large-scale research project (LSRP) and their timings.
Year 1
| September- December | Trainees familiarise themselves with research work and ongoing LSRPs in the department/school
Trainees complete online courses in Good Clinical Practice and Research Integrity to ensure familiarity and obtain a certificate in research governance skills |
| October | Research Project booklet: presentation of research areas and ideas by potential supervisors for this time period or trainee cohort.
Trainees approach potential supervisors after receiving the booklet to discuss potential research projects with them. |
| December | Trainees submit their choice of preferred projects (in order of preference) to Admin who will collate and convey choices to supervisors |
| January | Trainees notified by Admin who their allocated supervisor will be |
| February | Deadline for completion of Research Contract with academic and field supervisors.
Trainees set up an electronic Study Master File and continue to update this file as appropriate throughout their research period |
| February – May | Trainees develop their LSRP proposal with supervisors and carry out background reading as appropriate; they undertake an initial review of the literature
Trainees also develop links with relevant NHS services and obtain clinical service agreement |
| May | Submission of LSRP proposal and related documents to Admin and preliminary review |
| July | The first Research -Sub-Committee panels review the LSRP proposal and complete subsequent revision of project as appropriate |
| July | Review of revised project by the second Research Sub-Committee panels. Letters of approval issued. |
Year 2
| September – December | After receiving an approval letter from the Chair of the Research Sub-committee panel, in accordance with research governance requirements, trainees prepare and submit their ethics applications to relevant NHS and/or university research ethics and governance committees. |
| January – March | Trainees finalise research governance requirements and continue liaison with host service(s). Trainees begin data collection after final ethical and HRA approvals have been granted |
| March – September | Trainees continue with data collection and draft their systematic literature review. |
| September | Annual appraisal of clinical, academic and research progression |
Year 3
| October–December | Dedicated research block for ongoing data collection and analysis where appropriate. Trainees complete first draft of their systematic literature review and sections of the main empirical paper(s) |
| January-March | Completion of data analysis and writing up of thesis |
| End of April | Completion of thesis and electronic submission and hand in of two paper copies for examination |
| April – June | Preparation for viva and submission of papers to target journals |
| July | Viva voce examination |
LSRP: Research Sub-committee
Constitution of the ClinPsyD Research Sub-committee
The Research Sub-committee (RSC) is a sub-committee of the Executive Committee of the ClinPsyD Programme. The overall RSC is chaired by the Research Director of the ClinPsyD Programme who reports back to the Executive Committee on matters relating to the research components of the ClinPsyD Programme. The Research Director also reports to the School of Health Science’s Postgraduate Research Committee. The RSC is made up of ClinPsyD Programme team members, other academic supervisors who provide input into the programme, IT Support, Community Liaison Group and representatives of all three years of trainees.
The sub-committee, in the form of two concurrent panels, meets on two separate occasions (with the second meeting of each panel being for re-submissions only) to review the LSRP research proposals submitted by trainees. The Research Director will chair one RSC panel and the Deputy Research Director will chair the other. Trainee reps are invited to RSC panel meetings to ensure transparency of the review process, however reps are required to respect the confidentiality of the RSC panel and should refrain from divulging details about trainee proposals outside of the panel.
In exceptional circumstances, it may occasionally be possible for an extraordinary RSC panel to meet to receive and consider LSRP research proposals from trainee’s seeking peer review outside of the scheduled dates set for the RSC panels. Such extraordinary RSC panels are at the discretion of the Research Director.
Other “business meetings” may be held outside of the scheduled RSC panel meetings at the request of the RSC and/or the discretion of the Chair of the RSC. There are typically two or three RSC business meetings per year.
The RSC has two statutory duties:
- Scientific peer review of the large-scale research project (LSRP) proposals through two RSC panel meetings held in Year 1.
- Overseeing the ongoing support and supervision of the LSRP including
- Scrutinising any changes to the regulations under which the LSRP is examined.
- Scrutinising changes to the ClinPsyD Research Methods module
- Research governance issues as these appertain to the LSRP
- These duties are discharged through a minimum of one meeting per year, to which the Research Methods module organiser reports. Additional meetings, whether relating to the above statutory duties or to other appropriate matters relating to the research components of the ClinPsyD programme can be held outside of the scheduled meetings at the request of the RSC and/or the discretion of the Chair of the RSC.
- The membership of the RSC comprises:
- Research Director (RSC Chair)
- Deputy Research Director (Deputy RSC Chair)
- Research Module organiser
- Programme Director
- Academic Director
- All lecturers and Academic Advisors on the ClinPsyD Programme team
- Trainee representative(s)
- External members from the School of Health Sciences and NHS clinical psychology departments as invited by the Chair
- All members of the RSC are invited to all statutory meetings as set out above.
- Actions under the jurisdiction of the RSC can be taken by Chair’s action, with the approval of the RSC.
- The decision of the RSC is final in matters appertaining to the ClinPsyD programme that fall under its jurisdiction.
Evaluation and scrutiny of Large-Scale Research Projects (LSRP)
During Year 1, trainees are introduced to and provided with guidance on how to complete the LRSP proforma (see Research Methods module). Completion of this proforma is also overseen and finalised by their supervisors. In the summer term of Year 1, trainees submit their large-scale research proposal (see intranet for downloadable proforma), which must include a realistic budget and timetable for the research.
If the proposed LSRP will be recruiting from an external organisation or service (e.g. an NHS clinical team), the proposal must be accompanied by a letter or email from an authorised manager at the service or organisation in question. Trainees should be aware that a letter/email from a field supervisor is not sufficient in this instance.
All LSRP proposals must be reviewed by the Research Sub-committee prior to the trainee commencing work on the research project. As such, each trainee’s proposal will be reviewed at an RSC panel. It is mandatory for a trainee’s LSRP proposal to be approved by the Research Sub-committee panel before the trainee can proceed with the project. Please note that trainees are not required to present their LSRP proposals to the RSC panel in person. To ensure transparency of process, trainee reps will be invited to contribute to the RSC panel discussions. Although trainee reps are actively encouraged to engage in RSC panel discussions, all feedback on specific LSRP proposals is expected to be provided by the panel chair. Trainee reps are required to respect the confidentiality of the RSC panel and should refrain from divulging details about trainee proposals outside of the panel.
The purpose of the RSC panel is to provide written feedback to the trainee as to the appropriateness of the proposed design, hypotheses, methodology, scope and the study’s feasibility as described within the LSRP proposal. Whilst all of these areas are potentially open for review, the RSC is likely to place a stronger emphasis on the viability and feasibility of the proposal, given the timeframe available within the ClinPsyD programme. As such, scrutiny of the original design and methods and related contingency plans for the project should be expected.
Whilst the LSRP proposal form requires the trainee to outline a proposed literature review, it is expected that this outline will be at a preliminary stage. Trainees are encouraged to propose a research question, design, and justification for their literature review, and how the review links with the proposed empirical work. The RSC panel may offer comment on the perceived feasibility of the proposed review.
The scholarly peer review conducted by the RSC panel aims to offer constructive criticism on the trainee’s research proposal, with the intention of ensuring all approved proposals are likely to meet the standards required of a doctoral research thesis, which are that the LSRP makes an original, distinct and quality contribution to knowledge.
The ClinPsyD programme team recognise the potential for submission of the LSRP proposal to the RSC panel to be anxiety provoking for trainees. As such, the RSC panel will aim to provide written advice and guidance relating to the trainee’s LSRP proposal, especially if significant feasibility issues are raised. However, whilst the RSC may be able to offer guidance and suggestion for how such feasibility issues could be addressed, the decision on how to revise the proposal rests with the trainee, in collaboration with their supervisors.
Informal feedback should not be sought by the trainee author of the LSRP proposal from the trainee representative attending the RSC panel and the trainee rep should not divulge any details from the discussions of a specific trainee proposal to anyone outside of the panel. General feedback on the overall process of peer review could be shared by the trainee rep with their year group. Any concerns regarding the fairness of the peer review, or any other procedural matter, should be raised by the trainee rep to the chair of their RSC panel and/or the Research Director.
Almost invariably, the RSC will identify a number of changes to be made to trainees’ LSRP proposals before final approval can be granted. A letter describing the revisions to be made to the proposal will be sent to the trainee no more than 1 week after the RSC panel meeting.
The letter from the RSC panel chair will provide feedback across three levels, as detailed below:
- Required / Essential Changes: Such changes are required to address fundamental threats to the feasibility of the completion of the proposed project or the perceived ability of the project to make a novel, meaningful contribution to the literature. Examples of required changes may include proposed recruitment strategies that are perceived to be unlikely to be successfully achieved by the trainee, or the trainee’s research question and/or aims and objectives not being met by the proposed design and methodology stated within the protocol, or where the proposed study contains an insufficient focus upon clinical psychological theory or practice.
- Recommended Changes: These changes are recommended by the RSC panel but are not required to be made for RSC panel approval to be given. Examples of recommended changes may include a lack of clarity of expression within the protocol, or more clearly and simply stating a limited number of hypotheses for the proposed study, or methodological suggestions which the panel feel could make substantial improvements to the study (including measure selection, participant eligibility criteria).
- Further considerations: These suggestions are made by the panel for the trainee to consider but no changes are required to be made to the protocol. Examples of further considerations may include some guidance towards a key paper/text which was omitted from the proposal, views held by panel members about potential concerns or problems that the trainee may want to develop additional contingencies for.
It is expected that the revised proposal will be re-submitted not later than two weeks after the first RSC panel meeting. Therefore, trainees should expect to have to prepare a revised proposal and plan accordingly (e.g. pre-arrange access to timely supervision).
A second meeting may be convened by each RSC panel, towards the end of Year 1, solely for the purpose of considering revised research proposals. Under exceptional circumstances, trainees may be invited to attend to present their revised proposal. New proposals cannot be submitted to this second Research Sub-Committee meeting, except at the discretion of the Research Director.
Following receipt of a letter confirming approval by the RSC, trainees may initiate their research, beginning with an application to the relevant NHS Research Ethics Committee (via IRAS) or to the University Research Ethics Committee (UREC) as appropriate.
Please note: The decision of the Research Sub-Committee as to the suitability or otherwise of any given LSRP proposal is final, and RSC panel approval of an LSRP proposal in Year 1 offers no guarantee of the trainee passing the viva voce examination in Year 3.
LSRP: Ethics, Governance and Indemnity for Research
For the latest guidance on processes and procedures relating to Research Governance, please visit the FBMH Research Governance webpages where a resource pack can be downloaded: www.staffnet.manchester.ac.uk/bmh/research/ethics-and-regulatory-support/
Additional support for trainees conducting studies requiring approval from the Health Research Authority (HRA) / NHS REC, via the IRAS system, can also be found in the HRA Student Research Toolkit: www.hra.nhs.uk/planning-and-improving-research/research-planning/student-research/student-research-toolkit/
Ethical review and sponsorship
All projects which involve recruiting participants in the NHS will need to complete IRAS forms to obtain ethical approval which can be obtained from the following link.
https://www.myresearchproject.org.uk/
The University will generally expect to act as research governance sponsor for studies carried out by UoM staff and supervised students. The IRAS forms therefore need to be authorised by the sponsor before they can be submitted anywhere. Lynne MacRae, Research Practice Governance Manager, is the sponsor signatory for the Faculty of Biology, Medicine and Health. Before the sponsors can sign off the study they need to review the study/application as part of the sponsorship review process.
Full guidance on this internal review process can be found on the Faculty’s Research Ethics and Governance webpages (http://www.staffnet.manchester.ac.uk/bmh/research/ethics-and-regulatory-support/).
A brief summary of the steps in this process now follows.
Step 1 – Prepare your project’s ethics application in IRAS and generate all study documents (see below for list of required documents).
- IRAS full project dataset (Draft, and in PDF format)
- Protocol
- Information sheet(s) and consent form(s) (if applicable)
- HRA approval documents (Schedule of Events and Organisation Information document)
- Any other supporting documentation to be submitted to the REC e.g. CVs, interview schedule, questionnaires
- In addition, the following forms need to be completed. These need to be in place before the IRAS application can be signed, but we don’t need them to start the review process:
- Research Data Management Plan (RDMP) reference – The research data management policy requires that a data management plan is in place for all research (funded, unfunded, staff and student research)
- http://www.library.manchester.ac.uk/services-and-support/staff/research/services/research-data-management/
- Insurance assessment form – Please note that if any of the responses on the form are ‘yes’ then you will need to refer to the insurance office before the application can be signed off. http://www.staffnet.manchester.ac.uk/services/insurance/.
Step 2 – Submit a copy of your IRAS application to the Faculty’s Research Governance team (RGT): FBMHethics@manchester.ac.uk
Step 3 – The study will undergo a review by the RGT. Studies applying for NHS REC/HRA approval should expect to receive a response from the RGT within 15 working days although longer responses should be expected at busier times of the academic year (November – February). The RGT website contains a traffic light system to provide you with an indication as to how busy the RGT is currently.
Step 4 – The RGT will send feedback to you. Typically, further information or changes to the application are requested.
Step 5 – Revise your ethics applications in light of the RGT feedback and then submit the revised application form to the RGT along with any new/revised documents.
Step 6 – The RGT undertake final checks and confirm when the application is ready for authorisation. Once sponsorship has been confirmed, arrangements will be made for your forms to be signed off so that they can be submitted to the IRAS/HRA. Letters confirming sponsorship and insurance arrangements will be provided, along with confirmation of the University’s insurance cover which will need to be included as part of your application.
Documenting indemnity in IRAS forms
Once trainees have received ethical approval from NHS governing bodies, they must register their project for indemnity with the University Research Ethics Office (REO). Please note that research that is not registered with the University REO will not be covered by the University’s insurance.
As part of the IRAS application, trainees will be required to demonstrate that they are indemnified for any risks that may arise from the research. Trainees can download more detailed information about insurance statements from the intranet under research downloads, but a brief summary is provided here.
All trainees are covered by the University of Manchester’s policies and these should be referred to in the following sections of the IRAS form:
IRAS A76-1, -2 and -3:
The University of Manchester will arrange insurance for research involving human subjects that provides cover for legal liabilities arising from its actions or those of its staff or supervised students, subject to policy terms and conditions.
IRAS A77 (this question will only appear for certain types of study):
The University of Manchester will arrange insurance for research involving human subjects that provides compensation for non-negligent harm to research subjects occasioned in circumstances that are under the control of the University of Manchester, subject to policy terms and conditions.
There may be circumstances where, because of what is involved with the study, the insurance office confirms that a study is covered on a legal liability basis only i.e. non-negligent cover is not available but trainees will be informed of this when they submit their IRAS application for the internal review progress.
Reference to harm in Participant Information Sheets (PIS)
For research undertaken in conjunction with the NHS (or any other organisation not able to provide cover for non-negligent harm) the PIS should include only the NHS-approved wording – specifically it should not make any reference to cover for non-negligent harm. A reference to non-negligent harm could be seen to take priority over liability cover – even if the fault lay with the NHS. The following statement is recommended:
“In the event that something does go wrong and you are harmed during the research you may have grounds for a legal action for compensation against the University of Manchester or <insert names of other participating organizations> but you may have to pay your legal costs. The normal National Health Service complaints mechanisms will still be available to you.”
For research that is undertaken wholly by the University (or in conjunction with organisations that provide cover for non-negligent harm) the following wording can be used.
“In the event that something does go wrong and you are harmed or suffer loss as a result of taking part in the research you may have grounds for claiming compensation from The University of Manchester or <insert names of other participating organizations>.”
In order to protect you, the University of Manchester has insurance in place that provides:
– compensation for non-negligent harm to research subjects occasioned in circumstances that are under the control of the University,
– cover for legal liabilities for injury, loss of or damage to property, or financial loss arising from the University’s actions or those of its staff or supervised students.
If you make a claim in respect of legal liability you may have to pay your legal costs.
Registering research protocols and review protocols:
It is good practice to register both protocols for your empirical research (paper 1) and your literature review (paper 2) prior to carrying out the work. For example, supervisors will typically encourage trainees to register their review protocols on PROSPERO (https://www.crd.york.ac.uk/prospero/). There are also a number of registries available for protocols for empirical research studies (e.g. www.researchregistry.com). Trainees should consult with their supervisors about the most suitable register to use for their empirical research protocol. Whilst not always mandatory, registering protocols is good practice in terms of increasing transparency of the research process and ensuring that researchers report data in line with initial hypotheses and data analysis plans.
LSRP: Presentation as a Thesis
The Manchester ClinPsyD Programme has taken the paper-based (i.e. a collation of papers ready for submission to relevant journals) format as the default form of the doctoral thesis. Trainees will be expected to submit their theses in the paper-based format unless there is sufficient reason for them to submit in the standard, chapter-based format. Trainees wishing to opt out of the paper-based format will be requested to outline their reasons for doing so on their proposal submitted to the Research Sub-Committee (RSC) at the end of Year 1. This will be discussed by the RSC and notification sent to the trainee with approval for the project.
Thesis format
In all aspects other than format, the thesis must otherwise conform to the regulations governing a standard PhD thesis. Typically, the ClinPsyD thesis will comprise 1) a systematic literature review prepared for submission to a pre-determined journal (‘review paper’), 2) a draft of a paper prepared for submission to a pre-determined journal (‘empirical paper’) and 3) a critical appraisal of the review and empirical study carried out (‘critical appraisal paper’ not for submission to a journal). Following advice from supervisors, trainees may submit two empirical papers in addition to the review paper and critical appraisal paper. However, in these instances the overall length of the four collective papers must not exceed 25,000 words, excluding ancillary sections. This means that the title pages, abstracts, references and appendices are not included within this word count. In addition to the three papers, trainees must submit an overall scientific abstract (as per PhD thesis guidelines) and a lay abstract which can also be used to facilitate dissemination of the findings to stakeholders.
Thesis format: Literature review
The default format for the literature review is a systematic review closely linked to the main research project. A systematic review seeks to a) identify all relevant published and unpublished evidence, b) select studies or reports for inclusion, c) assess the quality of each study or report, d) synthesise the findings from individual studies or reports in an unbiased way and e) interpret the findings and present a balanced and impartial summary of the findings with due consideration of any flaws in the evidence (Hemingway & Brereton, 2001). Trainees should be guided by their supervisors about whether or not to use a previously published quality appraisal scale or a more bespoke component approach to quality appraisal. A document detailing the issues raised by each approach is also available from the intranet under research downloads.
If a systematic review is unfeasible (for example, because insufficient appropriate studies have been published in the relevant field), the trainee should discuss other options (e.g. narrative review) with the supervisory team. The format and guidelines for the target journal should be adhered to but when no word limit is stated, it is expected that the review will be a maximum of 8,000 words, excluding ancillary sections. This means that the title page, abstract, references and appendices are not included within this word count.
Thesis format: Empirical paper
This paper should also be prepared in accordance with the guidelines of a specific journal, which should be included in the appendices of the thesis. Whilst is it permissible for the paper to have been submitted to the journal in question, it is not permissible to include a published paper (including proofs or on-line format) as the empirical paper in the thesis. The word limit of the target journal should be adhered to in all cases when this is stated, but when no word limit is stated, it is expected that the empirical paper will not exceed 8,000 words, excluding ancillary sections. This means that the title page, abstract, references and appendices are not included within this word count.
Thesis format: Critical appraisal
As the ClinPsyD thesis is a doctoral level thesis, the focus of this section should be a consideration of how your present study fits in with and contributes to the overall programme of research of which it is part and how it more generally contributes to theory and practice in the particular field. If you have done a systematic review and study, the critical appraisal paper should put the current review and study in the wider context of research and practice and link the review /study findings to relevant theoretical underpinnings.
It should be borne in mind that in writing this section, the trainee should be referring to and appraising the research process as a whole, making reference to what was not done and why it was not done, as well as to the work that was actually carried out. When writing this section, the trainee should consider the following points (NB these are not necessarily headings):
- Strengths and weaknesses of the present study (i.e. the work actually carried out rather than the methodology or line of enquiry as a whole)
- Advantages and disadvantages of the broad methodological approach used in the present study and consideration of alternative methodologies that could have been utilised.
- Limitations of the line of enquiry as a whole
- Consideration of diversity and inclusivity issues (i.e. reflections upon the cultural appropriateness of the review and empirical study, with particular attention paid to the psychological constructs investigated and decisions affecting design and methodology)
- Implications for theory
- Implications for practice
- Suggestions for further research
We recommend that trainees create a document/journal where they record their reflections and decision making processes throughout the research process. Whenever decisions are being about the research (e.g. about which measures, design, groups, analysis to use), a brief note could be made in this document recording the different options that were considered and how you decided which to pursue. This will not only inform the content of the critical reflection paper but also foster a systematic approach to making decisions about research.
As the discussion sections of the review paper and the empirical study paper will have addressed some of the issues relevant to this section already, it is expected that this section will not exceed 6,000 words, excluding ancillary sections. This means that the title page, abstract, references and appendices are not included within this word count.
The trainees can include personal reflections on the research processes or their development as a researcher, but they have to bear in mind that the thesis will become a public document approximately two years after submission. Thus, they are advised to use an appropriate academic writing style throughout.
In addition to the above reflections, trainees are encouraged to include comment, within the critical appraisal paper, on the broader impact of their research including a dissemination strategy for both the review and empirical papers. As part of this strategy, it is expected that both of these papers would be submitted for publication in an academic journal. Trainees are also expected to engage in broader dissemination activities, including providing a lay summary of results to participants and services that supported recruitment, presentations to community organisations, public conferences, etc.
Submission of ClinPsyD thesis
There is a thesis submission deadline towards the end of April in Year 3 for trainees. Please check the Academic Dates section of the handbook for the specific date. At least six weeks in advance of the submission date of the thesis a Notice of Submission Form for each trainee has to be submitted on eProg.
The LSRP is presented for examination as a thesis in accordance with the University of Manchester regulations for PhD theses (see Canvas under research downloads for University guidance on the presentation of the alternative format thesis). Two bound copies and an electronic version of your original thesis and the final version must be submitted; copies for first examination may be soft-bound. The final version of the ClinPsyD thesis is submitted online only. Electronic copies will be retained indefinitely by the University, but trainees will be able to limit access according to their preferences and those of the supervisors. Trainees are expected to limit access to their thesis for two years to enable them to publish their findings in peer-reviewed journals.
Theses should be submitted to:
Doctoral Academy, Faculty of Biology, Medicine and Health,
Simon Building, Room 1.97
The University of Manchester,
Manchester M13 9PL
Tel: 0161 275 1437 / 1430
thesis-support.doctoralacademy@manchester.ac.uk
https://www.bmh.manchester.ac.uk/doctoral-academy/essential-information/thesis-submission/
LSRP: Assessment
Assessment format and process
In order to graduate on time, the research thesis must typically be presented by the end of April in Year 3. Please check Academic Dates for specific date. The thesis must represent a substantial and original piece of research of clinical relevance. The thesis should be presented in a form that complies with the general University Regulations on the Presentation of Theses which are supplied prior to submission.
As stated within the LSRP Research Contract (downloadable from intranet/Canvas), prior to thesis submission, the trainee is required to prepare drafts of the literature review, empirical paper, and the critical reflection paper. The academic supervisor(s) are allowed to review a maximum of two drafts of the thesis papers (one draft for Paper 3) and give feedback in written form. Supervisor(s) are to provide feedback to the trainee within no more than two weeks of receiving thesis drafts, unless otherwise arranged by both trainee and supervisor(s).
Following submission, the thesis will be reviewed and examined by both internal and external examiners. Examiners for the viva will be set by the Research Director and Programme earlier in Year 3. The examination process will be confirmed each year with each intake, and exact dates and timescales given.
The thesis is assessed in the same manner as a PhD, via an oral viva voce examination, which lasts approximately 45-60 minutes. This is typically held in July of Year 3. Trainees may be asked to defend any aspect of their thesis (in addition to any aspect of other work undertaken as part of the ClinPsyD) during this oral examination. Following examination, the examiners send a report on the thesis to the University of Manchester Faculty of Biology, Medicine and Health Research Degrees Panel, which in turn recommend acceptance, revision or rejection. Typically, trainees are notified of the outcome of the viva verbally by their internal examiner at the end of viva day and the formal report with a detailed list of correction will be sent by the examiners office at a later date. We ask trainees to wait until the end of the day before informing them of the outcome of the viva rather than immediately after the viva, so that examiners have an opportunity to discuss and resolve any discrepancies in consultation with other members of the examinations meeting.
Minor revisions should be completed before the end of the programme. Trainees are given six to twelve months to complete major revisions, although it may also be possible to complete the revisions before the end of the programme depending on how extensive they are. If this is not possible it may delay graduation in December and registration with the HCPC, which may have employment implications.
Possible awards for the thesis are:
- Award
- with no corrections
- subject to minor corrections being made to the satisfaction of the Internal Examiner
- Refer for re-examination by both examiners
- permitting submission of a revised thesis for examination without further research and without further oral examination
- permitting submission of a revised thesis for examination without further research but with a further oral examination
- permitting submission of a revised thesis for examination with further research and with a further oral examination
- Reject
The University does not have an alternative award in place for those students who are unable to complete the programme due to extreme mitigating circumstances. Such cases would be considered on an individual basis but students should be aware that, in these circumstances, they would not be eligible to apply for HCPC registration.
Timescales for revisions
For Aii awards (minor corrections), trainees will have four weeks in which to complete any changes required, although 12 weeks may be allowed in exceptional circumstances. The internal examiner must confirm that changes have been made to a satisfactory standard.
For Bi-Biii awards (major corrections), trainees are provided up to six or twelve months to complete any changes, depending upon how extensive they are. The internal examiner (and the external examiner for Bii-Biii awards) must confirm that changes have been made to a satisfactory standard.
Upon receipt of this confirmation, the Programme will send the trainees’ details to the HCPC to confirm completion of degree. In order to attend the winter graduation ceremony in December, confirmation that corrections have been successfully completed should be received by the end of September.
Interruptions and extensions
All requests for an extension must be supported by the thesis supervisors and must be submitted to the School of Health Sciences in the first instance on the relevant forms obtained via the supervisors. Please note that all decisions regarding deferment and extensions are made at Faculty level and not by the ClinPsyD Programme. All requests for an extension must include a schedule of work and a projected submission date. Requests for short extension periods (i.e. less than six months) will generally not be supported by the Faculty without very good reason. In addition, once an extension has been granted it is very unlikely that the extension period will be extended if the thesis is not submitted within the specified time. It should be noted that failure to collect sufficient data for any reason is not an acceptable reason for an extension.
It is expected that a request for an extension will only be made if there have been insurmountable difficulties beyond the control of the trainee, for example, if the research project has had to be substantially changed at a late stage. If there are substantive reasons for a trainee to request an extension to the submission date for the thesis, permission must be obtained from the University of Manchester Research Degree Panel. This can be either on the grounds that a “writing up period” is required or that an “extension to programme” is being sought. There are different procedures and different fees attendant on each of these options; trainees should discuss any concerns with their supervisors and Programme staff as early as possible.
Please note: It is generally the Panel’s view that requesting a few more weeks to write up the thesis is indicative of poor planning and time management and will not be considered as a valid basis for requesting an extension.
If it is necessary to temporarily suspend the LSRP, for example, due to maternity leave or long-term illness, this must be logged with the University as well as with the NHS as appropriate. The relevant form must be obtained via the research supervisors.
The Programme Administrator and Research Director must be informed of all requests for a deferment of the submission of the thesis, whether because of an interruption or extension, and any such request should be made as early as possible. In the case of an interruption or extension, the necessary oral examination will be arranged at the convenience of the external examiner concerned. Trainees should be aware that interruptions and extensions could significantly delay the award of the ClinPsyD, which has implications in terms of employment during the period between the formal end of the Programme and the award of the qualification.
Mitigating Circumstances
Trainees should note that mitigation is not normally considered for the submitted ClinPsyD thesis of their LSRP, because in extenuating circumstances an extension or interruption is usually the recommended course of action. However, should events immediately prior to examination necessitate mitigation, students should contact the Programme Director, Research Director or Programme Administrator as soon as possible to discuss if mitigating circumstances apply.
Plagiarism
If either the internal or external examiner suspects that thesis or a proportion of the thesis has been plagiarised, the relevant text will be submitted to ‘Turnitin’ to help determine the originality of the work.
LSRP: Technical and Statistical Support for Research
The Programme is able to provide and facilitate some technical and practical resources for the completion of the large-scale research project. Libraries in Manchester are excellent and are well supplied with electronic information access systems. Computerised networks (Intranets, access to centralised computerised information services and access to the Internet) are rapidly being developed, as is the provision of personal computer facilities. Specific advice and support for on-line and other computer-based research methodologies is available within the Programme team from Austin Lockwood in the first instance.
Trainees have access to a range of statistical software (usually through the library) and practical statistical support and advice from Dr Lesley-Anne Carter (0161 275 5886, or lesley-anne.carter@manchester.ac.uk).
The Programme has a selection of commonly used assessments and measures (or licenses for such) and technical equipment (HR monitors, actigraphs, video cameras and audio recorders), which can be made available for use in trainees’ large-scale research projects, subject to availability. Handbooks and manuals for tests will be provided on a reference basis by the Programme, although trainees are responsible for purchasing their own consumable portions of the test (i.e., questionnaires and scoring sheets), batteries etc., and these should be budgeted for accordingly. In the case of the Audit of Clinical Activity and the Service Related Project, it is generally expected that any materials required would be obtained from the relevant placement.
Trainees needing specific assessments or measures should discuss their requirements with Tracey Hepburn as early as possible and before instigating any research. Full details of each assessment required must be provided, including cost and supplier, along with a completed ‘Request for Test Materials’ form, available in the department or to download from the trainee intranet. Trainees should ensure they have considered availability of test materials at the proposal submission stage.
LSRP: Funding
Typically, a budget of £400.00 is available for each LSRP, to cover purchase of test materials, photocopying, postage, travel and Patient and Public Involvement (PPI) expenses. Mileage for the LSRP should always be claimed from the University and not from the NHS. The University pays 45p per mile and the relevant claim forms can be found on the intranet and must be submitted to Tracey Hepburn for processing. Please note that it is not permissible to claim for printing or binding of the thesis. Conference expenses can constitute a legitimate claim, provided that the trainee will be presenting their LSRP findings at the conference and that they make the claim during their training period. Payments/reimbursements made to participants should also come from this budget, but trainees should be aware that the procedure for claiming participant payments is subject to change from year to year. Trainees wishing to reimburse participants should contact Tracey Hepburn before submitting a proposal to discuss this procedure. Trainees will not necessarily be reimbursed for unapproved expenditure related to their LSRP and proposed spending will be comprehensively reviewed as part of the research proposal by the Research Subcommittee. For more detailed up-to-date information about the type of items that can be claimed from the research budget and the process for doing so, please see the documentation available to download from the ‘Research Downloads’ section of the intranet.
In order to support PPI input into the development of trainees’ LSRP proposals, trainees are permitted to access their research budgets for PPI activities prior to approval of the LSRP proposal by the Research Sub-Committee panel. Access to the research budget for all other research project related expenses is prohibited until after RSC panel approval.
Requests for additional research funds
Evidence suggests that £400 is sufficient for the majority of trainee projects. However, we are aware that some projects could cost more than this. If your proposed project falls into this category then you are invited to make a case for extra funds as part of your research proposal. These requests for additional funds, which should be clearly costed and fully justified, must be made in writing within the LSRP proposal submitted for scrutiny by the Research Sub-Committee. The Research Director will consult with the Programme Director, Deputy Research Director and Head of Division regarding the feasibility of the request. We will try to consider your funding request alongside the Research Sub-Committee process, as the availability of funds is likely to have a bearing on the feasibility of the project.
The Programme will do its best to meet reasonable additional costs but we cannot guarantee that the additional funds will be available. We will not be able to reimburse additional costs that are not agreed prior to the project starting.
Where possible all equipment should be borrowed from the programme or supervisory team (e.g. recordings, testing manuals, software, foot pedals, mobile phones).
Reasonable project costs include but are not limited to:
- Travel expenses at current University rates
- Questionnaires
- Excess transcription costs (trainees are expected to complete at least 5 x 1 hour interviews themselves)
- PPI consultation at INVOLVE rates
- Participant reimbursement (e.g. vouchers or cash)
- Translation costs
- Presentation at conferences (attendance alone is not a justifiable cost)
- Specialist training courses for project-related methods that are not available for free within the University
- Any equipment that is not available through the programme or supervisory team
- Stationary, printing, photocopying or postage
LSRP: Data Protection
his page should be read in conjunction with the page on information governance and data protection more generally.
All research work that involves the collection and storage of data must be carried out in accordance with the provisions of the Data Protection Act (2018).
The University of Manchester adheres to the principles set out in the Russell Group’s Code of Good Research Governance which requires that all research data are recorded, dated and subsequently stored securely, preferably at a level higher than the individual. Archiving of data, research results and records should be in such a manner as to be immune to subsequent tampering and falsification (e.g. password protected archives for images, numerical data and other records, etc.).
By the completion of training, all data (including hard copies and electronic files) collected for all of the ACA, SRP and LSRP should normally be stored after the study is completed at the clinical and/or University bases associated with the research. This must be logged in with the Programme Administrator, together with any appropriate keys and codes.
Data storage must conform to both data protection and ethical procedures, particularly with respect to any statement about data storage that has been included in an ethics application or in information given to research participants. Thus, where it has been stated that data are to be destroyed at a certain point, trainees must ensure that this is carried out. Where data are to be stored without identifying information, this must be achieved with appropriate care. The normal expectation is that data used in published research, where this does not infringe participants’ rights, should be available for scrutiny up to five years after a paper is published.
Where trainees do not have an appropriate clinical base at which to store research data during the course of their research, on no account must raw data be stored at their home on anything other than on a short-term basis (e.g. overnight or over a weekend) and any such storage must necessarily be secure. Appropriate arrangements should be made to store data at either an appropriate clinical base or at their academic supervisor’s University base. The Programme team and the University data protection service should be consulted if there are any queries about data protection. It is also beholden on trainees to ensure that they are operating in accordance with any NHS Trust or other relevant organisational data protection procedures and protocols. Trainees should be aware that in some circumstances, lapses in data security will have to be reported to the University and possibly to the Data Commissioner with potentially serious consequences.
At the end of the research project, trainees should ensure they have discussed data storage with their supervisory team. The Programme does not provide any data storage space as standard, and supervisors must arrange this on a case-by-case basis.
For further information on data protection contact:
Records Management Office
Compliance and Risk
G.011, John Owens Building
The University of Manchester
Oxford Road
Manchester
M13 9PL
Email foi@manchester.ac.uk
LSRP: Use of Social Media
Trainees may decide to use social media to either recruit to their projects or to disseminate their findings. The programme has a twitter account to publish research activity and any trainees wishing to post messages on this account should contact Katherine Berry. Both the BPS Division of Clinical Psychology and the programme have general guidance on the use of social media, which can be downloaded from the general forms and procedures section of the intranet. Both the University Research Ethics Committee guidance for social media use and the BPS ethics guidelines for internet-mediated research are also available in the research downloads. The following link provides further information about how researchers might use the social media to communicate and collaborate with the public:
LSRP: Guidance for Meta-Analyses
Meta-analysis is a powerful technique for combining the results of multiple different studies to provide an overall estimate of a particular effect or association. Meta-analysis can be seen as an extra step when undertaking a systematic review, providing a particular approach to synthesising the results of the papers in a review once the data form individual studies has been extracted. Meta-analysis will not be suitable for every review question. A common alternative to a meta-analysis is to undertake a systematic review with a narrative synthesis whereby the author compares and contrasts the results between studies themselves, noting common themes and gaps within the studies’ results.
Where trainees are undertaking a systematic review of quantitative research, a clear rationale for why meta-analysis was not undertaken should be given. This should ideally be discussed in the review paper itself.
During the programme, specific teaching on meta-analysis will be provided, although those intending to undertake a meta-analysis are advised to read more widely around the subject.
Undertaking a meta-analysis does not necessarily entail a large amount of additional work beyond completing a systematic review. In some cases, meta-analysis provides a more direct and streamlined way of synthesising data from multiple papers, and may not require much additional work compared to a narrative synthesis. Notably, narrative syntheses often involve many challenges in terms of how studies are meaningfully compared and contrasted, and how the subjectivity of the author conducting this process is managed.
A common reason for not conducting a meta-analysis is that the available studies are too heterogeneous. In other words, although all studies in the review pertain to the same research question, methodological differences (different samples, measurement, designs) mean that it would not be valid to aggregate the results from the papers into a single overall effect using meta-analysis. Heterogeneity can be a valid reason for not conducting meta-analysis, but the presence of heterogeneity does not always rule out meta-analysis. Some researchers argue that in situations with heterogeneity between studies, meta-analysis is still preferable to a narrative synthesis (e.g. Loannidis et al., 2008). In such cases, meta-analysis may provide a more explicit means of summarising the amount of heterogeneity and explaining the possible causes of this, compared to a narrative synthesis where the impact of between study heterogeneity may be lost or understated.
Thus, argument against using meta-analysis merely on the ground of high heterogeneity between studies needs to be carefully considered and argued. Let us consider an example of a situation where high heterogeneity would prevent meta-analysis. In a review of the psychological mediators between trauma and self-harm, the likely range of possible mediators that would be identified is large (e.g. emotion-regulation, coping skills, attachment, beliefs, self-esteem, etc.), including many phenomenologically distinct constructs, and so combining data from measures of all these constructs into a single effect is unlikely to be meaningful. It is this lack of a meaningful result that prevents us from pursuing a meta-analysis for this review, and so a narrative synthesis is preferred.
The decision to undertake meta-analysis, or not, as part of a systematic review should be carefully considered with one’s supervisory time. The points below provide some general advice on when meta-analysis may be appropriate and when it may not be appropriate.
- Meta-analysis is well suited to research questions concerning simple bivariate associations between variables. For example, looking at the association between trauma and psychosis, or low self-esteem and depression.
- Meta-analysis is often well suited to reviews of trials focused on whether a particular treatment is effective for a particular outcome (e.g., “Is CBT effective for reducing anxiety in young people”)
- Meta-analysis is less likely to be suitable where a review is focused on a broad set of potentially distinct constructs or variables. For example, a review looking at the “psychological risk factors for social anxiety in adulthood” is likely to result in a very broad range of risk factors being identified. It would not necessarily be meaningful to combine the effects of these distinct risk factors into a single meta-analysis. However, if there were adequate numbers of studies focused on a particular risk factor (e.g. self-esteem, beliefs about others) then a series of meta-analyses focused on particular risk factors may still be possible.
- Meta-analysis may be less suitable or more challenging if the constructs of interest (e.g. shame or attachment style) have been conceptualised in multiple highly distinct ways. In such cases it may still be possible to conduct a meta-analysis by focusing in on a particular subtype of the construct of interest (e.g. body-related shame)
- Meta-analysis is less well suited to more complex relationships between multiple variables. For example, studies focused on mediation or moderation effects, can be more difficult to meta-analyse because of the increased scope for heterogeneity. Similarly, study designs that involve repeated assessment of variables over time, such as ESM or longitudinal studies, may be more challenging to apply meta-analysis to. However, meta-analysis may still be possible in some instances.
- It is possible to undertake meta-analysis to answer questions about the prevalence of certain phenomena (e.g. “how prevalent is suicidal ideation in people with psychosis”).
References:
Loannidis, J., Patsopoulos, N., Rothstein, H., 2008. Reasons or excuses for avoiding metaanalysis in forest plots. Br. Med. J. 336, 1413–1415.
Professional Conduct, Ethics and Other Responsibilities of Trainees
Lines of responsibility
Formal responsibilities
For the academic component of the Programme, trainees are formally responsible via the Programme Director to the Head of the Division of Psychology and Mental Health. In all placement-related matters, the trainee is responsible to the Clinical Directors. While on placement, the supervisor carries clinical responsibility, and the trainee is therefore responsible to him or her for all aspects of clinical work. Greater Manchester Mental Health NHS Foundation Trust (GMMH) carries vicarious liability for trainees on placement, and retains overall management of the trainee. Professor Gillian Haddock, Head of the Division of Psychology and Mental Health, carries line management responsibility for trainees on behalf of GMMH. As Programme Director, Dr Richard J. Brown carries overall responsibility for the organisation and delivery of the training programme and in this respect is accountable to the University, the Health and Care Professions Council and the British Psychological Society.
For detailed information about trainee responsibilities see the Other Trainee Responsibilities section of the handbook.
Staff Responsibilities
Staff members adhere to the University of Manchester Manual of Academic Procedures (MAP), and are mindful of their responsibilities in relation to both academic and personal support.
NHS Constitution
All staff and students are expected to abide by the NHS Constitution, which is referred to in the Personal and Professional Development teaching during the induction block. It can be accessed online at:
http://www.nhs.uk/choiceintheNHS/Rightsandpledges/NHSConstitution/Pages/Overview.aspx
The key principles of the constitution are:
- Patients come first in everything we do
- We value every person as an individual, treating them with respect and dignity at all times
- We are committed to quality of care
- Compassion is central to the care we provide
- We strive to improve people’s lives
- Everyone counts: no-one is excluded, discriminated against or left behind
Disciplinary Policy
As employees of GMMH, all trainees are also subject to Greater Manchester West NHS Mental Health NHS Foundation Trust’s Disciplinary Policy, which outlines how matters pertaining to staff conduct and discipline are managed. The Disciplinary Policy is available from the Trust intranet and should be read alongside the ClinPsyD handbook. The Policy provides examples of what might constitute a disciplinary matter (i.e., misconduct or gross misconduct) and the actions that should be taken in the event of such a matter coming to light. The Programme will follow the processes set out in the Disciplinary Policy in all cases where possible misconduct has been identified. In such cases, the ClinPsyD Programme Director (or, in exceptional circumstances, the ClinPsyD Clinical Director) will have delegated authority to administer the disciplinary procedure, in consultation with the Trust Lead for Psychological Services.
Trainees should consult the Disciplinary Policy for general examples of misconduct or gross misconduct. Other behaviours that would be considered examples of misconduct in the context of the ClinPsyD include (but are not limited to):
- unwillingness to correct behaviours previously identified as inadequate performance;
- writing offensive comments in lecture feedback;
- failure to observe the British Psychological Society and Health and Care Professions codes of conduct;
- failure to observe formal University policies, procedures, protocols and guidelines;
- unjustifiable refusal of a reasonable instruction issued by the Programme, a supervisor or line manager (including failure to complete non-assessed but mandatory pieces of work);
- any behaviour suggestive of dishonesty that does not reach the threshold for gross misconduct;
Other behaviours that would be considered examples of gross misconduct in the context of the ClinPsyD include (but are not limited to):
- plagiarism;
- other forms of cheating in academic assessments;
- falsification of research data;
- other types of academic malpractice;
- wilful unauthorised absence from lectures or placement;
Depending on the seriousness of the matter in question, a range of possible outcomes of the disciplinary procedure are possible, including dismissal from GMMH. In the event of dismissal, the trainee will automatically be deemed to have failed the ClinPsyD programme. As the basis for employment with the Trust is attendance on the ClinPsyD programme (which requires employment in a specific capacity at a given level), downgrading or transfer are not possible outcomes of the disciplinary process.
Professional Conduct, Fitness to Practise, Academic Malpractice and Plagiarism
In addition to the responsibilities that apply to all University Programmes, trainees are employed as NHS practitioners and are expected to behave at all times in accordance with the NHS constitution. Trainees are also expected to behave in a way that is consistent with the Standards of Conduct, Performance and Ethics set out by the Health and Care Professions Council (HCPC), the professional regulatory body for clinical psychologists, and with the British Psychological Society’s Code of Ethics and Conduct. Ultimately, a high standard of professional conduct is expected at all times, and trainees are expected to approach all aspects of their studies with this in mind. Trainees should familiarise themselves with the HCPC Standards and the BPS code, as well as their responsibilities as students of the Manchester ClinPsyD, and behave accordingly.
All new entrants are required to sign the Code of Professional Conduct and Fitness to Practise for Clinical Psychology Students, which sets out standards for personal behaviour, behaviour towards others, learning, barriers to learning or professional practice, duty of care, duty to report and confidentiality.
Students should be aware that the Faculty of Biology, Medicine and Health has a duty to ensure that students are fit to practise, and their procedures will be followed if there is a question over a student’s fitness. Postgraduate students need to be aware that in the event of misconduct, dishonesty, unprofessional behaviour or anything else that raises the possibility that the student’s fitness to practise may be impaired, the University has a duty to protect the public and may have to inform the relevant professional regulatory body. This means, for example, that where a clinical psychology student has been found to be dishonest (e.g., plagiarism, collusion, falsification of research data or other forms of cheating) the matter may be reported by the University to the HCPC. Students who are dishonest not only risk failing to be awarded the intended degree, but also place at risk their whole professional career.
Unprofessional conduct can take many different forms and can arise both on clinical placements and during the academic component of the course. Students should be aware that unprofessional conduct includes academic malpractice (e.g., cheating, plagiarism, falsification of research data), as well as behaviours such as missing programme activities without permission, consistently arriving late for programme activities, inappropriate behaviour (e.g. using a mobile phone during teaching, being rude or disrespectful to others), breaching information governance rules, allowing their GMMH email account to lapse, making personal remarks in feedback to lecturers, handing non-assessed pieces of work in late and so on.
Any concerns about professional practice should be brought to the attention of the Programme Director in the first instance, who will then gather views and evidence from the Clinical Tutor and Academic Advisor. Depending on the level of concern, the matter may be dealt with locally or we will initiate further steps as outlined in the Faculty’s Fitness to Practise procedure and/or the employing Trust’s Capability and Disciplinary processes.
Please note that details of any instances of unprofessional conduct may be recorded in a trainee’s file and may be referred to when members of the programme team write references for potential future employers. Instances of unprofessional conduct will be dealt with by the Programme Director or their nominee (e.g., clinical tutor) in the first instance; if the incident is considered serious enough (or there is evidence of several less serious incidents) then a Student Progress Meeting (involving the trainee and their tutors) may be called and/or further steps taken as per the Faculty Fitness to Practise procedure.
Ground Rules
The Ground Rules below were originally developed by the Programme Team following a Personal and Professional Development session with Year 2 trainees. All year groups develop their own set of ground rules during the Induction block, but previous trainees have found the examples below helpful.
As with all professional working relationships, certain standards of professional behaviour in the workplace are taken as read. The starting point for the development of these Ground Rules is that similar standards of professional behaviour are expected by the Programme Team and visiting lecturers as on placement. It is expected that trainees will:
- Approach the appropriate member(s) of staff for information on particular subjects (e.g., Research Director/Tutor about research, Clinical Directors/Tutors about placements etc.)
- Use web pages for routine information regarding the Programme
- Use year group representatives on committees and sub committees to maximise effective communication
- Adhere to a system for communicating with trainee year group to be adopted by all three year groups (e.g. e-mail, “telephone tree” etc.)
- Approach each aspect of the Programme recognising that there are opportunities to be sought and that it is all organised in good faith
- Be mindful of the personal impact of their feedback about lectures and the implications for the future curriculum
Academic Malpractice and Plagiarism
The University does not permit plagiarism or other forms of academic malpractice under any circumstances, and individuals found to have committed such an incident can expect a harsh penalty, which in some cases results in exclusion from the university. To ensure that you are fully informed about University expectations and understand your responsibilities with regard to academic malpractice please ensure you have read the guidance provided by the University to students on this topic. This is available at:
http://documents.manchester.ac.uk/display.aspx?DocID=2870.
If you have any doubts or further questions please contact your academic advisor or the programme director.
As further support the Faculty of Biology, Medicine and Health training team has developed a mandatory course unit entitled “Understanding Academic Malpractice”. This unit is mandatory for all postgraduate students and will allow you to test your understanding of what constitutes plagiarism and academic malpractice. You can access the course from your Blackboard course list in My Manchester. The course unit should be completed as soon as possible after you begin your programme, but must be completed before you submit your first piece of academic writing for assessment.
For more information on the University’s governing Regulations, please see the University website at: www.manchester.ac.uk/aboutus/governance or contact a member of staff.
Working Practices and Deadlines
As Doctoral students, we expect trainees to be independent, responsible and self-directed in learning, and to establish patterns of study that will contribute to their capacity for life-long learning. It is the responsibility of the trainee to familiarise him or herself with what the requirements of the programme are, and to take the lead in ensuring that these are met. Trainees should, for example, familiarise themselves with the dates of examinations, the specifications for clinical reports and research work to be handed in and the deadlines for these. Failure to do this could result in a failure of a piece of work. Deadlines for submitting work are always 9.00am on the specified date, unless otherwise communicated to trainees.
PLEASE REFER TO THE ACADEMIC DATES SECTION OF THE HANDBOOK FOR FURTHER INFORMATION
Information Governance, Confidentiality and Data Protection
The Data Protection Act
Trainees are given information about information governance and the Data Protection Act (2018) in the Induction Block and are required to complete a short, examined course on this as part of the mandatory training for GMMH. This course is completed on an annual basis. It is important that trainees familiarise themselves with the Data Protection Act and adhere to it.
Students must ensure that they understand all professional and programme requirements in relation to confidentiality in undertaking and reporting on work with service users and their families during their training. All trainees are expected to follow the Data Protection Act and the NHS Code of Conduct in relation to confidentiality, which set out how personally sensitive information should be protected and what information can be shared and under what circumstances.
Confidentiality in Case Reports and presentations
It is absolutely essential that Case Reports and Case Presentations preserve the confidentiality of the client(s) and the Service. Information identifying clients, other professionals and institutions must be removed. You must go through any letters or reports that you are enclosing and ensure that you have deleted the name of the client and other information that could lead to identification of them (including diaries, thought records etc. that may be in the appendices). The obvious points are: the hospital file number; name of supervisor; addresses; place of work; job title, specific dates (the year is acceptable)
The name of the individual may be shortened to one initial, but in many cases you may prefer to use an assumed name (stating on your report that you have done so). Without losing track of the sense of the report, information such as the name of a previous hospital or of a doctor who has seen the patient should be removed. We appreciate the need to provide some details about the client in order to explain social context but it is always better to give general descriptions rather than specific details. Date of birth must not appear, although year of birth and age are acceptable. When you blank out the reports please use tippex and then photocopy to ensure that the information is completely erased. If the material is crossed out but can still be read underneath it has not been anonymised. You should be aware that clients are now legally entitled to access case reports.
Failure to systematically anonymise your work will result in a Fail being awarded for “Style and Presentation” if the breaches occur in the main body of the report, or for “Appendices” if the breaches occur here. Oversights, in the context of a predominantly well anonymised report, will be highlighted by the markers. In both cases, trainees will be required to rectify any breaches of anonymity before their overall mark can be formally recorded.
As it is difficult for you to make sure that you have picked up every occurrence of the client’s name or other identifying features, we strongly recommend that you edit your reports in conjunction with a service colleague, who could also read through the report for you to see if you have made any errors.
Securing sensitive data
We would like to draw particular attention to the Data Protection Act’s requirement that personal data (such as that pertaining to clients on placement or research participants) is kept securely and appropriately. In practice, this means that any personal information held electronically (e.g., on a computer, laptop, memory stick, recording device) must be stored in encrypted form and/or on an encrypted device. All hard copies of personal information (including case reports) should also be stored securely, that is, in a locked filing cabinet or similar. Every effort should also be made to anonymise personal information where possible, such as in clinical case reports. Even when this has been done, encryption/secure storage should still be used, as trainees often make mistakes in anonymisation, or the client might be recognisable from the incidental and contextual information provided in the report. These rules pertain to both final and draft versions of case reports.
Individual files can be encrypted using the encryption function in 7-Zip or Word 2007 and later versions (not Office 2003 or earlier versions). File encryption passphrases should be a minimum of 7 characters but longer passphrases are stronger. Passphrases should use a mixture of upper and lower case letters, numbers and special characters (!ӣ$% etc.); recognisable words should be avoided. When communicating passphrases (e.g. for case report submission), it is safer to do so by speaking with the recipient in person, by telephone or by text; e-mail is generally regarded as less safe, particularly when using non-University systems.
When handing in case reports, trainees should give their memory stick/CD to one of the admin staff in person and communicate the passphrase to them. They will write this down and store it separately to the memory stick/CD (both under lock and key).
The University’s Data Protection policy is available from the University website at:
http://documents.manchester.ac.uk/DocuInfo.aspx?DocID=14914
Please also see the page on Data Protection in relation to the Large Scale Research Project.
Consent
Overview
It is essential that trainee clinical psychologists obtain informed consent for all assessment and interventions offered. In practice this means providing the following information:
- What the psychological work involves, including any risks and alternatives.
- That the client(s) are being seen by a trainee clinical psychologist.
- Limits to confidentiality – that this may entail discussion in supervision, video/ tape recording, writing case reports and case presentations.
All discussions regarding consent should be documented. When undertaking clinical work on an NHS placement, trainees should use the host NHS Trust’s own policies and procedures for obtaining consent. This should be discussed with supervisors who should be able to provide advice on local policies and documentation such as consent forms. Points to consider when obtaining consent:
- Consent is both voluntary and continual (clients can opt out of treatment/being recorded etc. at any point).
- All consent should be well documented.
Gaining Consent
Everyone aged 16 and above is presumed to be able to give consent for themselves unless it can be demonstrated that they are unable to do this.
If someone is mentally competent to give consent but physically unable to sign the form then an independent witness can be asked to confirm that the patient has given oral consent.
Consideration of Specific Client Groups
Children Under 16
Parental consent must be obtained. If a child under age of 16 years has sufficient understanding they may sign the form with a parent countersignature.
Young people 16-18 years
Parental involvement recommended but not necessary.
Clients who lack capacity to give informed consent
Some adults over 18 years may find it difficult or lack the capacity to give or withhold consent e.g. impaired cognitive capacity, brain injury, learning disabilities or dementia or severe mental health conditions.
If it is still not possible to gain consent from the individual concerned then the course of action taken must be deemed to be in the client’s best interest (Mental Capacity Act, 2005).
Discuss with appropriate relevant people including supervisor, clients care manager, key worker, relatives and/or advocate.
Consent Form Practicalities
The Programme has introduced a sample Consent Form (see Downloads on the Programme Intranet) that can be used or adapted if no standard consent form is in available within the service.
The following checklist may also prove helpful if trainees and supervisors prefer to develop their own consent form. The following information should be stated clearly on the form:
- Both the consent form and any recordings are Private and Confidential.
- Address of placement.
- Indication of who you are (Trainee Clinical Psychologist), University affiliation (University of Manchester) and level of study (Doctorate in Clinical Psychology).
- A statement of what the client is consenting to e.g. audio/ video taping.
- Clear sentence of consent which the client can highlight in some way to indicate agreement/disagreement in recording.
- Client name, signature and date.
- Trainee name, signature and date.
If you are using audio/ video recording, within the context of the consent form it should be indicated that any recording is:
- Voluntary and consent can be withdrawn at any time.
- Recordings will be kept securely (locked) and note how long they will be kept.
- Will be destroyed after use.
- Will not be part of patient records.
- Will only take place with prior consent.
- Is a learning tool and will not affect level or quality of care.
- Can be switched off at any point.
- Confidential with the exception that it may be listened to by your supervisor who will adhere to strict confidentiality policies.
Further Reading
- British Psychological Society (2009). Code of ethics and conduct. Leicester: BPS.
- Department of Health (2001). Good Practice in consent implementation guide. London: Department of Health. Health
- Professions Council (2016). Standards of conduct, performance and ethics. London: HCPC.
- https://www.justice.gov.uk/protecting-the-vulnerable/mental-capacity-act
Attendance and Notification of Absence
Overview
An important principle is that as employees of the NHS, trainees must be accounted for on every working day. Attendance at academic events, including all lectures, is compulsory.
In order to ensure that we have a clear record of attendance for the teaching programme, trainees are asked to sign in as present at lectures on teaching days. If a trainee is unable to be present, he or she must telephone and let the administrative staff know at the earliest opportunity. It is the trainee’s responsibility to ensure that their reasons for non-attendance are recorded. Unexplained absence from any activity represents a breach of contract, and disciplinary action will be taken. See ‘Sickness Absence’ for more information on procedures for notifying us when you are absent.
The programme prescribed is a continuous one of three years of full-time study. ClinPsyD students are expected to work for the duration of the programme throughout semesters and vacations, with the exception of reasonable holidays, which must be logged with the Programme. Except for these holidays a student should be available for consultation with his/her supervisor throughout this period.
Research days taken outside the usual timetable must also be recorded. On placement, the supervisor will tell you what the expectations concerning working hours are and you must comply with these. Programme staff must be informed of days absent from placement.
Sickness Absence
If a trainee is unwell, whether on a placement, teaching or study day, they must telephone the department and let the administrative staff know. This should be at the earliest opportunity. The Trust requires that all staff, including trainees, provide a reason for their absence for recording purposes. The trainee must also ring the department and let the administrative staff know when they have returned to work. Trainees should also contact their placement if they are unwell and unable to attend on a clinical day. Following a period of sickness absence, the trainee’s clinical or academic tutor will contact the trainee to conduct a return to work interview.
Special Leave
As NHS employees, trainees may request time off for unexpected events such as the sudden illness of a child/dependant (Unplanned Carers Leave) or following the death of a close relative (Bereavement Leave).
For the maximum amount of paid special leave an employee can receive in any rolling 12 month period please refer to the NHS policy. There are other types of special leave; for further information please see the NHS policy which can be downloaded from the intranet or contact Tracey Hepburn.
Anticipating Difficulties and Self-Care
The Programme Team want trainees to get the best out of the opportunities offered by the Programme, and enjoy their training. Trainees on the Programme are all graduates, with a wide range of experience. The Programme Team are keen for trainees to take the initiative, assume responsibility and act proactively in relation to difficulties. We know that problems sometimes arise that have an impact on the training experience. It is very helpful if trainees make us aware when such problems arise, and we will act in good faith to try to help. We are well aware of the sensitivity of some issues that can arise and will discuss issues of confidentiality with trainees.
Sometimes, problems arise which may prevent a trainee from submitting or undertaking an assessment at the specified time. In this case, the Programme must be advised as soon as possible, and formal notification of mitigating circumstances given using the procedures and forms set down by the University. For further information on this, please see the page on mitigating circumstances.
Health and Safety
Overview
The legislation governing health and safety of all employees is the Health and Safety at Work Act (1974): http://www.hse.gov.uk/legislation/hswa.htm
It states the duty of employers to provide a safe working environment for employees and the responsibility of employees to take reasonable precautions to ensure their own safety and adhere to the policies of the employing agency.
The University of Manchester has Health and Safety policies that apply to staff and students. Trainees need to read the relevant policies, including those relating to lone working and research. Risk assessments will be completed with supervisors as part of research studies. Further information can be found on the University Safety Services website: http://www.healthandsafety.manchester.ac.uk/
All trainees will complete the University online mandatory training in Health and Safety as part of their first-term teaching. This provides information about managing risk and about reporting incidents and accidents to the University.
Reporting incidents
All accidents, incidents and near misses, however minor, occurring on University premises or arising from University business must be reported to a member of the ClinPsyD administration team, using the appropriate form available on the intranet (under Downloads > General Forms and Procedures). There are two forms, an Accident Report Form and an Incident/Near Miss Report Form. Please submit completed forms to the admin team who will then forward them to the relevant Programme Team Members and Health and Safety Officers within the School.
For your information:
An ACCIDENT is defined as any unplanned or unwanted event that results in injury, damage or loss and should be reported using the accident report form.
A NEAR MISS is any unplanned or unwanted event that had the potential to result in injury, damage or loss, and an INCIDENT is any event that results in physical damage to property but no injury has occurred. Both should be reported through the incident/near miss report form.
In addition, trainees will need to read and follow the Health and Safety policies and procedures of their employer (Greater Manchester Mental Health and NHS Foundation Trust). Training will be provided on these as part of the NHS mandatory training for all trainees. On placements, the HCPC Standards of Education and Training state that “practice placements must provide a safe and supportive environment.” This is monitored by clinical tutors in supervisor inductions and placement visits, and also by trainee feedback at the end of each placement – on the Trainee Evaluation of Placement (TEP) form. On placement, trainees must be aware of and abide by the policies of the placement provider and finding the relevant information must form part of the placement induction. Further guidance on this can be found in the section below.
Please note that if an accident, incident or near miss occurs on placement then trainees will need to report this to the placement provider using the relevant local guidance and reporting system AS WELL AS reporting to the University using the relevant forms as described previously.
Guidance for Trainee Health and Safety Induction
This document is intended to support Supervisors in ensuring the health and safety of ClinPsyD Trainees during their time on placement. It is suggested that Supervisor and Trainee use this document as a framework for discussion during placement induction.
It is important that Supervisors are aware that whilst Trainees are on placement they are covered by and must abide by the health and safety policies of their host service. It is recognised that, in some cases, the departmental/Trust policies might not address the specific needs of Trainees and that different issues are pertinent in different specialisms and locations. This guidance is therefore intended to assist Supervisors in the induction of Trainees on placement within a service and provide a structure for the discussion of health and safety issues with Trainees.
- Departmental Procedures
- Signing in and out of the workplace(s)
- Indicating one’s whereabouts if not in the office base
- What (if anything) will happen if a member of staff does not return at an expected time
- Telephone answering protocols
- Fire evacuation
- First Aid
- Incident reporting (trainees must complete a University Accident/Incident Form as well as following NHS procedure)
- Other
- Case Files
- Storing of case files
- Status and storage of supervision notes
- Removal of files from the department
- Seeking consent for audio and video recording
- Storing of data on computer
- Sending client information electronically or by fax
- Other
- Home Visiting
- Home Visiting Policy
- Other
- Risk Assessment
- Ensuring the safety of client and therapist at all places of work on placement e.g., self harm, aggression, boundaries etc.
- Other
- Use of Equipment
- Booking procedures
- Training requirements
- Liability for loss or damage
- Use of personal equipment for placement work e.g., laptop computer, mobile ‘phone etc.
- Other
- Transport
- Requirement for car use within placement
- Insurance requirements (onus on Trainees to ensure appropriate cover)
- Risk assessment of providing transport for clients
- Other
- Security
- ID badges
- Security codes/keys
- Personal alarms
- Security within workplace
- Security within site and parking areas
- Security within surrounding area
- Other
- Specialist Training/ Health Requirements
- CPR/Disengagement training requirements (not provided by the ClinPsyD Programme)
- Immunisation requirements (available for Trainees from Occupational Health)
- Other
Programme Policy on Social Networking Sites
Social networking sites (such as Facebook, Twitter and Instagram) are increasingly popular ways of keeping in touch with friends and peers. Whilst we recognise that many people will wish to use such sites, it is important for trainees to remember the potential risks of using them and to take care when placing information in the public domain; trainees must also ensure that their privacy settings are appropriate.
The University has social media regulations, including guidance for students which can be found here. Trainees are advised to also refer to the Faculty of Biology, Medicine and Health guidelines on social networking. In addition, NHS England has developed a document for professionals entitled An introduction to: Using social media during your career, which can be downloaded here.
We understand that trainees may already be aware of potential risks of these sites but are seeking to raise awareness through this part of the handbook and remind trainees of their responsibilities in this regard.
Managing Personal and Professional Risks of Social Media Use
Boundaries
Whilst the majority of clients will understand and respect therapeutic boundaries, trainees should be mindful that clients might become curious about their therapist and attempt to look up information using these sites or cross boundaries by making contact. Vice versa, it would not be appropriate for trainees to attempt to search for clients on these sites. We are aware of several instances where clients have attempted to contact health professionals, and feel this may increase as the popularity of such sites grows.
Confidentiality
Client confidentiality should be respected at all times and no information about clients or Trusts (direct or indirect) should be shared on any sites. This also applies to ‘closed’ groups, even if privacy settings are maximised. BPS, HCPC and Trust guidelines relating to confidentiality should be adhered to at all times. See the section on Information Governance, Confidentiality and Data Protection for further information.
Groups
Be aware of the groups that you create/join and the impression that this might give to others.
Personal information
Trainees should be aware of who can access personal information (such as telephone numbers, addresses, relationship status etc.) on social networking sites and consider their privacy settings in line with safe practice guidelines. Trainees should also be aware of information that they might place about others on these sites.
Cyber-bullying, cyber-harassment and e-defamation
Cyber-bullying, cyber-harassment and e-defamation are types of behaviour which are prohibited under English law, and being accused of such behaviour may result in legal action being taken against you by the affected party. You may also be subject to University, Trust, or Professional Regulatory Body discipline if you are found guilty of such activities.
What is cyber-bullying?
Cyber-Bullying can take many forms, for example sending threatening or upsetting emails or setting up social networking profiles with the intention of making fun or humiliating someone. “…victims of cyber-bullying have complained that they have seen personal photos, emails or blog postings posted where others could see it without their permission” (http://www.directgov.org.uk).
What is cyber-harassment?
Cyber-harassment is to “pursue a course of conduct which amounts to harassment of another and which the defendant knows or ought to know amounts to harassment of another” (HMSO, 1997).
Examples include racial, religious or sexual aggravation and putting people in fear of violence through the sending of inappropriate and offensive text messages, emails or internet postings. Legal protection against cyber-harassment is provided in the UK by the Protection against Harassment Act (HMSO, 1997) and covers all forms of communication including electronic.
What is defamation?
Defamation is the communication of a statement that makes a false claim, expressly stated or implied as factual, that may harm the reputation of an individual. Posting inappropriate comments relating to University or Trust staff, colleagues or patients can put your professional registration and your place on the programme at risk.
Professional Practice and Safeguarding
We would like to advise trainees to be aware that their general behaviour may have an impact on the professional life and they need to be clear that their professional reputation is not compromised. Below are some guidelines and suggestions that may be helpful:
- Review and consider using privacy settings that restrict access to your profile, allowing access and visibility to only those you are aware of.
- Consider who will be able to see personal information such as your address, mobile, telephone and detailed social plans on these sites and adjust your security settings accordingly or amend information.
- If a client or member of their family attempts to contact you via a social networking site, do not respond and discuss this with your supervisor as a priority. It is likely that this will need to be recorded in an incident report for monitoring. If this happens, ensure that you discuss ways to manage this with a senior colleague before seeing the client again. We strongly advise that you do not accept the friend request.
- In line with professional practice, do not name clients or describe a client/situation that cumulatively might lead to identification of the client.
- Be mindful that some postings will be in the public domain. Do not post information that might be embarrassing or unacceptable if seen by work colleagues, potential employers or clients and their families.
- Be aware of information that may be shared if a mutual friend link exists between a client/supervisor and trainee. Consider carefully the language or terminology used within your site or postings.
- Remember that personal photographs can be viewed, copied, altered and posted elsewhere. It may be advisable to try to make sure that you have permission from others before adding photographs of them.
- Be mindful that others might post information or photos about/of you and that their settings might not be secure and therefore accessible by others.
- If commenting on identifiable individuals or places, consider what you say and bear in mind that this may be viewed by anyone with access to the site. Do not post offensive or derogatory remarks about others. Laws related to defamation, bullying and harassment all apply online and can lead to penalties.
- If accessing sites from a University or Trust computer, make sure that you abide by University or Trust regulations.
- Consider very carefully before joining groups that could be seen as discriminatory or judgemental. Ensure that sensitive information is not discussed, even in ‘closed’ groups.
- Be mindful that privacy settings do not always work perfectly and can be compromised inadvertently. Also be aware that privacy settings may change when social networking sites update their security and so it might be helpful to frequently review them.
Students are reminded that the appropriate place to provide feedback on the programme or any other aspect of university life is through the appropriate feedback mechanisms already in place i.e. through any member of the programme team, Executive committee, Placement Forum, Research Subcommittee, Staff-Student Liaison Committee or Student Support Office.
References and Resources
- HMSO (1997). Protection against Harassment Act, Available at: https://www.hmso.gov.uk/acts/acts1997/ukpga_19970040_en_1 Website accessed on 16.09.09.
- Guseh, J. S., Brendel, R. W. & Brendel, D.H. (2009). Medical professionalism in the age of online social networking. Journal of Medical Ethics, 35, 584-586.
- Guidelines from School of Nursing, Midwifery and Social Work, University of Manchester (Nov. 2009).
Please note that these guidelines are correct at the time of writing.
Giving Gifts
Trainees wishing to make a gift to members of the programme team are asked to do so once all examinations have been completed. Gifts over £20 must be declared by Staff. Please refer to the university’s policy for further information.
Sustainability on Campus
The University is committed to embedding environmental sustainability as a key priority across the full range of its activities. There are many ways that students can assist with this, including by:
Here are a couple of general links where you can learn why it is important to take active steps to help our environment:
- http://www.guardian.co.uk/environment/climate-change
- http://www.newscientist.com/topic/climate-change
Doing your bit
The “Student Sustainability Forum” (http://www.sustainability.manchester.ac.uk/students) is where students can express their concerns and share their ideas on campus environmental issues with University management.
Food
- “Food on campus”: look out for symbols indicating that the food and drink you purchase on campus are fair trade, local and sustainable.
- Other food venues around campus: see our handy guide, written by one of our students: http://psychologyatmanchester.edublogs.org/2012/03/01/eating-sustainably-on-campus/
- Join ‘hug a mug’, a scheme to reduce number of paper cups. A reusable cup costs £6 but you get 20p off on every drink you buy.
- Water: Bring your own bottle! Water coolers are available throughout School buildings. It takes 5 million litres of oil each year in Europe to produce, fill, ship and bulldoze the bottles discarded.
Waste: Please recycle!
- Separate bins for plastic bottles, cans, and general (non-recyclable) waste are available in the Zochonis building.
- Many other things can be recycled on campus, including glass bottles, batteries, CDs and DVDs, and more. Here’s where the collection points are: http://www.sustainability.manchester.ac.uk/campus/recycling/atoz
- Many cluster printers, e.g. in the main library, will allow you to print double-sided – please make sure you choose this option whenever it is available.
Travel
- Learn to cycle – receive free training; join monthly ‘free breakfast’ cycle to work groups from your neighbourhood; enjoy discounts on bike hire and accessories here: http://www.sustainability.manchester.ac.uk/campus/travel/cycling
- Learn about discounts for students on public transport and the free 147 bus: http://www.sustainability.manchester.ac.uk/campus/travel/buses
- Use your car sustainably by car-sharing; receive discounts on parking when you share or swap some car commutes by more sustainable travel: http://www.sustainability.manchester.ac.uk/campus/travel/cars
For further info, suggestions and feedback:
For a wealth of local info: http://www.sustainability.manchester.ac.uk
SPS Sustainability contact: Helen.Leah@manchester.ac.uk (Zochonis 128)
How to Communicate with and Influence the Programme
Communication and Information Sharing
Programme staff generally communicate via e-mail; we will always use your University email account, so please ensure that you check this on a regular basis. Each Year group also has a pigeonhole for correspondence in the main office. However, we will also occasionally need to correspond with you directly, and it is therefore vital that we have your current address and telephone number on file. Please don’t forget to inform us when you move; you can update your address, and telephone number on the intranet site under the ‘My Details’ link. This sends a link which will update our records; the Programme Assistant will then send information regarding how to update the Trust’s records and the central University system.
The Programme has also set up an online SMS-messaging service which is used to notify students of cancelled lectures. It is, therefore, important that we have your most recent mobile phone number if you wish to receive these updates. This can also be updated on the intranet.
You can get information to us via the:
- Administrative Staff: Megan Brown (306 0404), Indre Miskunaite (306 0401), Tracey Hepburn (306 0400).
- Directors: Richard Brown, Adam Danquah, Adrian Wells, Daniel Pratt, Claire Fothergill, Lara Bennett (0161 306 0400).
- Committee meetings: your Trainee representative may raise matters of general concern at the monthly Executive Training committee meetings; information/queries pertaining to teaching can be raised at quarterly Curriculum sub-committee meetings, whereas information/queries pertaining to placement can be raised at the bi-annual Placement Forum
- Trainee Advocate, who is a member of the Executive Training Committee
- Quarterly Staff-Student Liaison Committee meetings.
Student Representation on Committees
All of the programme committees have student representatives from each of the three year groups. Trainees are asked to nominate their own representatives at the start of the programme. Roles can be shared and representatives can change if the year group agrees. There are dedicated slots for trainee matters on all of the committee agendas, which offer an opportunity for concerns to be aired, feedback to be given and requests to be made. Trainees are full members of the committees and are expected to contribute to discussions in meetings, where they should feel free to offer their perspective and represent the views of their peers to the best of their ability.
Clinical supervisors should allow trainees time off placement to attend committee meetings, although this should always be confirmed with supervisors in advance.
Staff-Student Liaison Committees
At the end of each teaching block , the Programme Director and Academic Director meet with each year group to discuss matters of mutual concern. These staff-student liaison committee meetings were set up as an on-going dialogue between the Programme and students, and provide an opportunity for consultation, discussion and feedback. The agenda for each meeting is generated collaboratively and feedback on actions arising from the previous meeting is given. Most meetings take place within year groups but there is a larger liaison committee meeting every year that all staff members, trainees and CLG members are invited to. This takes places on the same day as the Programme Annual Review in September.
Giving Feedback
We take student feedback very seriously, and have made many changes to the Programme as a result of trainee views. Indeed, students have seen us completely re-structure the timetable in line with their comments. Our last BPS accreditation report commended the Programme on its feedback systems, noting that they “ensure that trainee concerns are given serious consideration”.
Teaching quality
Students fill in web-based ratings for every teaching session. Trainees’ names are not attached to their feedback (so it is effectively anonymous) but, if offensive or otherwise unprofessional comments are made, our electronic system allows us to track the author and take appropriate action if necessary. There is also a review as part of each Staff-Student Liaison Committee where the Programme Director, Academic Director and a member of the administrative staff meet the year group and discuss feedback on teaching sessions and the Programme as a whole. Minutes of the meeting are made and circulated to Module Organisers and students where appropriate. The Module Organisers also receive a list of the ratings for lectures and student comments. Module organisers write individually to lecturers to pass on the feedback, and make modifications to the Programme as necessary. Where a particular lecturer has been the subject of poor feedback, the chair of the Curriculum Sub-committee will make personal contact with the Module Organiser and decide what action should be taken to help the lecturer improve the quality of the teaching. We are subject to a system of peer review of teaching operated by the School of Health Sciences.
Placement quality
Students fill in rating forms on all placements. If there is a difficulty with a specific placement, feedback will be given. If there is no improvement, the Programme will give further feedback and decide whether or not to continue to use that placement.
Commenting on Training Overall
At the end of Year 3, there is a final review where trainees are asked to review the training experience as a whole. The overall experience of balancing teaching, exams, placement-based work and assessments and research is discussed. As a result, numerous changes have been made in recent years. For example, the reflective practice curriculum was introduced to the programme as a result of trainee feedback, with the aim of providing increased opportunity to explore and enhance reflective skills.
Academic Dates
Year 1
September 2021
- 20 Sept – 29 Oct: Induction block (6 weeks)
November 2021
- 1: Commencement of placement
December 2021
- 17: End of teaching
January 2022
- 05: Teaching begins
March 2022
- 7, 8, 10: Live observation assessment
- 18: End of teaching
- 23, 25: Study days (Research Proposal Development)
- 28 – 31: Study days
April 2022
- 1: Adult Exam
- 6,8,13,20,22: Study days (Research Proposal Development)
- 25-29: Placement handover week
May 2022
- 3 – 20 : Child induction teaching
- 23: Commence of placement 2
June 2022
- 10: ACA placement 1 submission (9:00am deadline)
July 2022
- 1: End of teaching
- 4 – 7: Study days
- 8: Child exam
September 2022
- 2, 5: Exam resits
- 9: Annual Review and Programme Trainee Liaison Meeting (compulsory attendance)
October 2022 (Yr 2)
- 24-28: Placement handover week
Year 2
October 2021
- 27 Sept-15 Oct: Induction Teaching (3 weeks)
- 1: Case report 2 submission (9:00am deadline)
- 18: Placement begins
November 2021
- 5: Submission date, ACA (9.00 a.m.) (Placement 2)
December 2021
- 17: End of teaching
January 2022
- 05: Teaching begins
March 2022
- 18: End of teaching
- 21-25: Placement changeover period and Interview Week (trainees to be released from placement)
- 28 Mar – 1 Apr: Study Week
April 2022
- 4: New placement begins
- 8: Case Report No.3 Submission (9a.m.)
May 2022
- 6: Submission date, ACA(9.00 a.m.) (Placement 3)
June 2022
- 18: Teaching finishes
- 20,21,23,27: Study days
- 22,24,28: Exams
August 2022
- 12,15: Resit exams if required
September 2022
- 9: Annual Review and Trainee / Programme Liaison Meeting (attendance is compulsory)
- 26-30: Changeover period
October 2022 (Yr 3)
- 7 TBC : Submission date CR4 (9.00 a.m.) tbc
Year 3
October 2021
- 27 Sep-16 Oct:Research days
- 18-22:Teaching begins (1 week block followed by 1 day a week)
November 2021
- 05: Submission ACA (9.00 a.m.) (Placement 4)
December 2021
- 13: End of teaching
January 2022
- 04: Placement begins
- 31: Teaching Day
February 2022
- 28: Teaching Day
March 2022
- 28: Teaching Day
April 2022
- 29: Thesis Submission
July 2022
- 7: Vivas
September 2022
- 08: Teaching Day
- 09: Annual Review, Trainee Programme Liaison Meeting
- 30: End of Programme
Support, Guidance and How to Raise Concerns
Trainees may encounter a wide range of difficulties in the course of their training, some arising specifically from the training experience, some from external factors, and some from a combination of these. Trainees have access to a number of support systems, both formal and informal, which may be of use at these times. These are discussed with trainees early on in their training, and include the following:
- The Programme Team
- Training Co-ordinator/Clinical Tutor
- Academic Advisor
- Supervisors
- Trainee representatives
- Buddy system
- Group support from other trainees/Peer Supervision sessions
- Trainee Advocate
- School of Health Sciences Student Support Officer
- University Student Guidance Service
The Programme Team is aware that training in Clinical Psychology is a demanding process and trainees may need a range of networks to ensure that they are supported adequately. Following extensive discussions between the Programme and trainees over a number of years, the Programme has now evolved a number of support systems. As the needs and views of trainees change, however, the personal support systems are reviewed by the Programme in collaboration with trainees. The Programme does not offer individual or group therapy to trainees, who are advised to seek help, if necessary, from a range of different possible providers, including their GPs. A system of confidential contacts is available to help trainees seek advice.
Our current policy can be summed up as follows.
- All trainees should have access to formal support and guidance systems within the structure of the Programme Team.
- There should be flexibility in the forms of support available, with formal, informal and confidential sources of support available.
- The existence of these forms of support should be made explicit to trainees on entry into the Programme.
- The support and development needs of trainees should be reviewed on an annual basis by a working party made up of Programme Team members and trainees.
- Trainee stress and its fluctuations should be recognised as a normal part of training, and the need to problem solve effectively encouraged.
The Programme has both formal and informal systems, some of which are trainee-led, and others of which are Programme-led. These are outlined in the Induction Block, and trainees meet their tutor and advisor at this stage. Trainees also have a session dedicated to establishing ground rules for the conduct of the group, and emphasis is laid on the value of the trainee group as a source of continuing support throughout training.
There is good representation of student views through the committee structure, and our systems are kept under review with the trainees. Questionnaires are used to assess trainees’ views. A working party of staff and trainees is formed when there are suggestions for change.
Academic Guidance and Tutorial Support
Academic Support
Throughout the Programme trainees have formal tutoring relationships with members of the Programme Team. All trainees have a Clinical Tutor and an Academic Advisor to whom they are allocated at the start of training, and who follow their progress throughout the three years of the programme. In addition, trainees have a series of clinical supervisors and a research supervisor, all of whom provide individual teaching, guidance and support. All tutors and supervisors are keen to help students make the most of all aspects of their training, and are happy to be approached over personal issues that may affect the trainee’s learning experience.
Clinical Tutor
The Clinical Tutor acts as training co-ordinator, overseeing all placements and carrying out placement visits. The Clinical Tutor visits placements every 3 months. One primary aim of the Clinical Tutor is to ensure that trainees have good placement experiences through assisting in identifying needs and goals in training, and in helping to ensure that trainees have a good experience of supervision. A further important aim is to maintain an overview of the process of training. Trainees should use meetings with the tutor as an opportunity to appraise their progress through training. An important aim is therefore for trainee and tutor to maintain an overview of the process of training, and to review all the major aspects of training on a regular basis. The Clinical Tutors also encourage discussion of any personal issues that may be affecting the trainee.
Academic Advisor
The Academic Advisor will advise on any aspects of academic work in relation to the taught programme, including performance in exams and other examined pieces of work. Tutorial support is available throughout the programme but particularly after exam and case report results have been issued, at which point trainees are encouraged to discuss their results with their Academic Advisor in order to review their results and the written feedback provided by the markers. One role of the Academic Advisor is to assist the trainee in selecting a research project and supervisor and to be an independent means of support during completion of the thesis. Therefore, the Advisor is not involved in the supervision of the research work in the second and third years of training. In Year 2, once the research supervisor has been chosen, if students choose their Advisor as supervisor they will be allocated a different Advisor. The Advisor formally oversees the progress and the supervision of the research project in accordance with the University of Manchester procedures for doctoral level research. Academic Advisors will be drawn from all academic staff.
Pastoral and Welfare Support
The Clinical Tutor and Academic Advisor are aware of the importance of providing support for the individual student, and are alert to welfare issues. Trainees also have a “buddy system” and a Trainee Advocate, who is a qualified psychologist with full membership of the Executive Training Programme Committee. We also have a range of Confidential Contacts, who are mental health professionals within and outside the Region who are prepared to help trainees think about how best to proceed with difficulties. Trainees are encouraged to use the University of Manchester Counselling Service as appropriate. We have had feedback from trainees that all these systems are useful. Additionally, the School of Health Sciences has a Student Support Officer whom students can access for pastoral support.
Trainee Advocate
The trainees elect a Trainee Advocate who is a qualified Clinical Psychologist independent of the Programme management. He or she will act on behalf of trainees with respect to all aspects of the Programme, and attends the monthly Executive Training Committee meetings. The Advocate has access to reserve business at meetings that trainees are not allowed to attend. See the Who’s Who section for contact information.
Buddy System
Before the start of the Programme new students will be contacted by one of the trainees already on the Programme who will act as a ‘buddy’. New entrants should be able to make use of their local knowledge and experience to help to settle in.
Confidential Counselling
A range of different systems exist to help trainees who may have personal difficulties. Trainees are given information on these at the start of the Programme. Contact information can be found on the Counselling service website: http://www.staffnet.manchester.ac.uk/personalsupport/counselling/
School of Health Sciences Student Support Officer
The School has a dedicated Student Support Officer, Ryan Hurst, whose role is to provide pastoral support to both undergraduate and postgraduate students. The SSO is not available to provide academic support, but can liaise with Programmes regarding academic issues if students are experiencing difficulties. Contact information may be found on the Programme intranet.
Student Support Service
Details of student support services in the University can be found here.
Supporting Trainee Clinical Psychologists experiencing a Serious Incident (SI)
The team is committed to supporting trainees who may experience a serious incident on any part of the programme, for example a risk-related event to self or others involving clients, research participants or trainees themselves or a client taking their own life. To this end we have developed a matrix of support which can be found on the intranet and which refers to support provided by both the programme and the employing Trust. We recommend that the support matrix is read in conjunction with relevant Trust and University policies, notably the University Incident Reporting policy and (employing and placement) Trust and University lone Working policies. In the event of a trainee experiencing a serious incident, they should contact their clinical or academic tutor in the first instance or if they are not available, any other member of the programme team, who will be able to guide the support process thereafter. This is in addition to any incident reporting systems that have to be followed on placement.
PGR Doctoral Academy Support
Support can also be accessed via the Doctoral Academy. A number of support groups can be accessed by PGR students, including Financial Support and a Student Parents & Carers Group. Further details can be found on their webpage.
Trainee Wellbeing
General approach to supporting trainee wellbeing
While we recognise that training is an exciting and stimulating experience, we are aware that it can also be a demanding process at times both professionally and personally. It is common for trainees to experience periods where they may feel overwhelmed and it can feel difficult to know when it may be helpful to access support particularly as these periods can be transient. In addition to this, professionals working in mental health may feel that it is difficult to seek help because of the view that they should be able to cope and because of worries about how this may be perceived.
We hope that the programme offers a supportive environment to counter these views and will always respond compassionately to any trainee or staff member seeking support with distress and mental health difficulties. Please be reassured that we will not automatically assume that you are unfit to practise and instead see your approach as a sign of good professional behaviour. Indeed, being true to the values of our own profession, we believe that acknowledging our own potential vulnerability and taking steps to maintain our emotional wellbeing requires personal maturity and strength. We also endorse the DCP position statement, which states that “lived experience of mental health difficulties does not have to be a barrier to training or practising as a clinical psychologist. On the contrary, people with lived experience are an asset to the profession and make a significant contribution to it.”
Trainees who recognise that they need support with their emotional wellbeing are encouraged to talk with a member of the Programme Team. This would usually be your clinical tutor, who will help you think about the best way forward. They will encourage you to reflect about whether you need to take time off work or seek additional support and are very happy to assist you with such decisions, but will do so without prejudice and assumption.
Sources of support/guidance
Following extensive discussions between the Programme and trainees over a number of years, the Programme has now evolved a number of support systems. As the needs and views of trainees change, however, the personal support systems are reviewed by the Programme in collaboration with trainees.
Internal sources of support/guidance
Student Counselling Service, offers a variety of support re emotional wellbeing, individual therapy and workshops
https://www.counsellingservice.manchester.ac.uk/
0161 275 2864
University Mental Health Service
Accessed through the Student Counselling Service, offering individual and group therapy ( up to 20 sessions) for complex mental health difficulties
Togetherall
A free online mental health and wellbeing support available 24/7 to University of Manchester students, staff and researchers, monitored by trained clinicians
University of Manchester Student 24 Hour Mental Health Service
A new 24 hour mental health service is now available to all University of Manchester students. The service includes a 24 hour helpline and app, and offers access to mental health support from trained counsellors and advisors who are ready to listen and provide help whenever you need it. It’s anonymous, non-judgmental and available 24 hours a day, 365 days a year.
You can call the helpline for advice and support on a whole range of issues you might be facing, big or small. Things you could call for include mental and emotional health, managing relationships, feeling worried about yourself or someone else, dealing with stress and anxiety, money advice, and everything in between.
The mental health helpline is provided by an independent external provider, Health Assured, and is a means for all University students and staff to access practical help, information, advice and support to address and resolve problems and issues you may be facing. The service is free, independent, confidential and available 24 hours a day, and Health Assured’s advisors are highly trained to talk your problems through and help you think about next steps.
How to access the helpline
You can access the helpline right away for help if you’re struggling, and it’s really easy to use. Call 0800 028 3766 and one of Health Assured’s advisors will answer. You’ll be asked to confirm which University you’re calling from and what your issue relates to so you can be put through to the right advisor to help you.
My Healthy Advantage App
As well as the helpline, you will also get access to the My Healthy Advantage App. You can request a call back, which means no call charges if you’re not in the UK. The app provides you with interactive resources to help track and improve your wellbeing. Within the app, you will get access to a library of resources personalised to your preferences, wellbeing articles, videos, mood trackers, 4-week plans, mini health checks and more.
The app also allows you to chat directly to an advisor using the online chat function. This option will only appear when an advisor is available to speak to ensure you get the direct support needed. This may be helpful for those people who feel anxious phoning the health assured number.
To access the My Healthy Advantage app you will need to enter the unique code below when creating your account. Code: MHA147866
External services and resources of support
Sometimes this might involve a referral through their GP, however below are a list of other resources which may be useful when considering support for emotional wellbeing.
Hub of Hope
A national mental health database of help and support services by postcode
https://hubofhope.co.uk
Self Help Services
Mental health charity offering a variety of services including self-help e-therapy and self-help talking therapies both individual and group therapy
Self referrals accepted
pws.manchester@selfhelpservices.org.uk
0161 226 3871
42nd Street
Greater Manchester Charity, (11-25 yrs) supporting emotional wellbeing and mental health. Offers a variety of services including CBT, EMDR, Counselling
Self referrals accepted
42ndstreet.org.uk
0161 228 7321
Manchester Institute for Psychotherapy
Offers low cost psychodynamic therapies by trainee psychotherapists
Mcpt.co.uk/low – cost-therapy-clinic
0161 862 9456
TLC
BACP accredited relationships charity offering individual and couples therapy
0161 872 1100
LGBT foundation Manchester
National charity offering groups, talking therapies, advice, pop in service
Https://lgbt.foundation
0345 3 30 30 30
Pink Therapy have a directory of therapists who work with gender and sexual diversity clients from an affirmative standpoint
www.pinktherapy.com
Mood Swings
Free, confidential information, advice and support for people with mood disorders, their families and friends
0161 832 3736
BABCP
The British Association for Behavioural and Cognitive Psychotherapies maintain a register of accredited CBT therapists
ACAT
The Association for Cognitive Analytic Therapy maintain a register of accredited CAT therapists
Manchester Mind
Local mental health charity offering a range of services including peer support and advice
0161 769 5732
Helplines
Samaritans: 0161 236 8000 (local call charges apply) or 116 123 (free to call). Open 24 hours a day. They offer confidential emotional support. This can be by telephone, email, letter and face to face for people in distress.
Saneline: 0300 304 7000. Open 4.30pm – 10.30pm every day. They provide emotional support and information.
Campaign Against Living Miserably (CALM): Helpline for men. 0800 58 58 58. 5pm–midnight, 365 days a year.
Domestic Abuse: 24 hour National Domestic Violence Freephone Helpline 0808 2000 247
Greater Manchester Mental Health NHS Foundation Trust – see Help! Leaflet that outlines useful contacts for mental health support in Manchester recommended by trainee’s employer trust.
Student Appeals and Complaints
Academic Appeals
Students have a right of appeal against any decision affecting their academic status or progress under University General Regulation XIX – Academic Appeals Procedure, which can be found here. The University sets out strict criteria for what constitutes appropriate grounds for appeal, which are articulated in Regulation XIX.
If a trainee wishes to appeal against a mark on one of the designated grounds then they should contact Richard Brown for an informal discussion in the first instance.
If, following this discussion, the trainee still wishes to appeal the decision then they must submit a formal appeal to the Faculty of Biology, Medicine and Health. This must be done in writing via the appropriate form, which can be found here. Appeals must be submitted within 20 working days of the date when the decision was communicated to the student.
Appeals should be directed to: Faculty Appeals and Complaints Team, Room 3.21, Simon Building, University of Manchester, M13 9PL (email: FBMHappealsandcomplaints@manchester.ac.uk).
Should I resubmit a failed piece of work even if I am appealing the mark and am still waiting to hear the result?
As a default, we would expect students to abide by the original mark and time frame for any resubmission unless and until they have written confirmation that their appeal was successful and that resubmission is no longer required. Whilst this could mean that students complete work unnecessarily (dependent on the outcome of the appeal), the alternative of ‘stopping the clock’ on the resubmission could result in them having longer to complete the work than students in a similar position who do not submit an appeal, which we believe would be more unfair. Although some aspects of the appeals process are out of the Programme’s control, please be assured that we will do our best to conclude the process as swiftly as possible.
Student Complaints
There is a University procedure (Regulation XVIII) for dealing with student complaints. Information about this can be obtained by clicking the links below:
Student Complaints Procedure (Regulation XVIII)
User Friendly Guide to Student Complaints
Regulation XVIII indicates that, wherever possible and appropriate, attempts should be made to resolve complaints informally and as soon as possible after the matters to which they pertain have occurred/become apparent. With that in mind, we request that any issues of complaint are brought to Dr Richard Brown as Programme Director in the first instance, to discuss whether the matter in question can be resolved informally.
If a trainee is not satisfied with the outcome of this informal discussion, or they decide that an informal approach is inappropriate, then they can make a formal complaint using the procedure and form referred to above. This must be submitted within 40 working days of the event or action to which the complaint pertains.
Confidential Contacts Network
The Programme has contacted a number of mental health professionals within and outside the Region who are prepared to help trainees think about how best to proceed with difficulties. These people should not be approached with an expectation that they will take on the trainee for therapy; rather, their role is to offer the trainee an opportunity to reflect on the nature of the problems and what they should do next. The Contacts have been selected on the basis of their range of experience, and knowledge of therapy networks, in and out of the Region. Material discussed with them would not be fed through to the Programme unless the trainee wished this to happen. They are as follows:
Dr Jan Hughes, Clinical Psychologist and Clinical Director, Leeds ClinPsyD Programme. Tel: 0113 343 2732, or email: j.hughes@leeds.ac.uk
Dr Ruth Butterworth. Tel:07854878026, or email: Ruth.butterworth@protonmail.com
Equality and diversity
The University is committed to providing an environment free from discrimination, bullying, harassment or victimisation, where all members of its community are treated with respect and dignity. It aims to create a culture of diversity within its community, providing a dynamic working and learning environment, where all members are valued for their contribution and individuality.
We are committed to providing equality of opportunity for all, irrespective of:
- age
- disability
- ethnicity (including race, colour and nationality)
- gender (including gender reassignment, gender identity, marital status, pregnancy or maternity)
- religion, belief
- sexual orientation (including civil partnership status)
The University’s Equality and Diversity policy can be downloaded here. Further information about the University’s activities in relation to equality, diversity and inclusion can be found here.
Any cases of harassment, discrimination and bullying will be taken very seriously by the University and, where necessary, the appropriate procedure will be used to investigate complaints. Further information about the University’s policies and procedures in this regard can be found here.
Disability Support
The Programme is dedicated to supporting students with disabilities and has implemented a number of changes to its training over the past few years in response to trainee needs. Trainees with a disability are not obliged to disclose this, but are encouraged to do so in order to help the Programme team to fully support his/her learning. Choosing not to disclose a disability may have implications on the support available. Although trainees are encouraged to disclose disabilities at the beginning of training, this may be done at any point throughout the Programme.
The Disability Advisory and Support Service (DASS) offers a wide range of support to students with disabilities and (with permission) will advise the ClinPsyD Programme on reasonable adjustments that can be put in place to support trainees across the three years in all aspects of their role (i.e. academic teaching, clinical placement and personal study).
Claire Fothergill (Clinical Tutor) acts as the ClinPsyD Programme DASS co-ordinator (Linda Steen is covering this role in her absence). Trainees wishing to declare a disability should in the first instance contact either Claire Fothergill, their Clinical or Academic Advisor or the Disability Advisory and Support Service directly. If you would like further information regarding the role of the DASS or support services that are available please contact Claire on claire.fothergill@manchester.ac.uk alternatively you could contact the DASS directly via the following link:
http://www.dass.manchester.ac.uk/
Following informal discussions, a review meeting will be arranged where trainee needs and reasonable adjustments are discussed. The Programme has a number of options available for support and, with advice from the DASS, will tailor support to each individual trainee.
Supporting Trainees Experiencing a Serious Incident
The Programme team is committed to supporting trainees who experience a serious incident on any part of the programme, for example a risk-related event to self or others involving clients, research participants or trainees themselves, or a client taking their own life. To this end we have developed a matrix of support which can be found on the intranet (Downloads section in the left hand menu) and which refers to support provided by both the Programme and the employing Trust. We recommend that the support matrix is read in conjunction with relevant Trust and University policies, notably the University Incident Reporting policy which can be found under the Downloads section of the intranet, General Forms and Procedures and (employing and placement) Trust and University Lone Working policies: Downloads, Support for Serious Incidents.
In the event of a trainee experiencing a serious incident, they should contact their Clinical Tutor or Academic Advisor in the first instance or, if they are not available, any other member of the Programme team, who will be able to guide the support process thereafter. This is in addition to any incident reporting systems that have to be followed on placement.
Learning and Physical Resources
The Programme
In planning the curriculum, we have focussed on recognised local strengths in evidence-based, cognitive behavioural therapies to provide a Programme that can help the student in developing expertise. This distinguishes us from other Programmes that may have more eclectic approaches. Teaching and placement-related experience is also offered in Psychodynamic Interpersonal Therapy, clinical neuropsychology and systemic work. The Programme always aims to appoint academic staff with a strong academic record and good teaching skills so that the excellence of the research base of the Department provides exposure for trainees to a stimulating, research-led environment.
Teaching accommodation
The Programme is based on campus in the Zochonis Building and has two dedicated teaching rooms, a meeting room and three smaller breakout rooms for group work. We also have access to rooms across campus for occasional workshops when necessary.
Technical and administrative support
IT Provision
Trainees have access to computer clusters in the basement of Zochonis with free printing facilities. They also have use of other machines on the University campus. University computers have statistical packages such as SPSS, NVivo to support analysis of qualitative data and reference manager programmes. School IT staff are available to help with queries or needs. The majority of students also have access to computers on placement.
eLearning
The Programme has a dedicated eLearning Technologist, Austin Lockwood, who is expanding our intranet site with useful student information. The Programme is developing an online bank of student multimedia resources, including videos demonstrating of therapeutic techniques. Austin has also developed a number of IT resources to support trainee research on the programme, including an online questionnaire system, a system to enable online Experience Sampling Methods research, an online Q sort programme and an online system for completing Delphi studies.
Library
The University of Manchester Library provides extensive access to relevant literature. The hospital libraries also run a service to obtain materials. As part of the contract for the Programme, we have a library budget with which books and journals can be purchased, and we welcome information from students on books and journals that may be suitable.
Equipment and Facilities
All the teaching rooms have audio-visual facilities available. Each year group is allocated a pigeonhole in the main administrative office to use for correspondence, and all trainees will be given a locker for the duration of their training. Year 1 and 2 trainees are able to loan either a camcorder or audio recorder and an encrypted memory stick, which they can use to facilitate reflection and supervision on clinical skill development. Year 3 trainees can request access to camcorders or audio-recorders, although these are not routinely provided, however a number of encrypted audio recorders are available for Year 3 trainees to borrow for their research if necessary. Client consent must be obtained to record clinical sessions and both local and national information governance rules must be followed when acquiring and storing clinical recordings (see section on information governance).
Trainees have a research budget of £400 and are able to use this money to purchase any equipment or materials they may need for their research projects. Trainees have access to rooms in the Zochonis Building and in other parts of the University for testing experimental participants under quiet conditions.
Trainees may access the departmental photocopier free of charge, and photocopying/printing is also available across campus facilities for a nominal charge. There is a large common room/canteen area in the basement of the Zochonis Building, with tea-making facilities and fridge/freezer. Trainees are expected to keep common areas tidy at all times and report any problems with facilities to the Programme Administrator. There is also a café (Food for Thought) on the ground floor of the Zochonis building that serves food and drinks during the day, within a larger social area (The Hub) that is also used by other members of the School of Health Sciences.
Placements
The Committee on Training in Clinical Psychology (CTCP) of the BPS has set down minimum criteria for facilities on placement, and the majority of placements are able to meet these. Where there are difficulties, these are discussed with the Clinical Tutors. It is appreciated that, in order to make use of placements where high-quality supervision and experience is available, trainees may have to compromise on physical resources, for example, desk space, and this is generally understood by the trainees. Health Education North applies “top down” pressure on Chief Executives of Trusts to provide adequate accommodation, while the Programme and supervisors work “bottom up” to try to bring about improvements. We welcome information on placement resources, and endeavour to act on any comments.
Intranet Link
Intranet Link for all policies and documents referred to in this handbook:
https://www.psych-ssl.manchester.ac.uk/clinicalpsychology/intranet2/login.aspx

