BSc (Hons) Healthcare Science (Audiology)
School of Health Sciences
Faculty of Biology, Medicine & Health
The University of Manchester
PROGRAMME HANDBOOK
September 2020
Version 1.12
Note: This handbook replaces all previous versions
Disclaimer
While every attempt has been made to ensure that the information given in this handbook is correct, errors may be present. Any subsequent amendments to this handbook will be published on Blackboard.
Other important documents relevant to your progress throughout your degree are the Personal and Academic Development Programme (PADP, Year 1) the Professional Skills Development Programme (PSDP, Year 2), the Practicals Handbook (years 1 and 2), the Research Project Handbook (year 3) and the Clinical Handbook (for clinical learning in all years). For details of clinic placements, clinical assessment and clinical professional issues (including health and safety) please see the Clinical Handbook.
Please note that due to the continuing development of this programme, some of the details in this handbook will change. Where changes occur, updated sections will be provided.
Covid19 statement
In response to the pandemic and in line with governmental guidance regarding social distancing, the BSc Healthcare Science (Audiology) programme will be delivered using a blended learning approach for the academic year 2020/21, commencing in Sept 2020.
This will affect the student learning experience in the following ways:
- Teaching: the majority of your teaching will be delivered online, with on-campus* activities where possible limited to a single day each week to limit the need to travel. On-campus teaching will take place in a safely socially-distanced environment. Practical classes* will be in small groups and PPE (for example, appropriate medical grade face masks such as those used in Audiology clinics) will be provided where necessary. For the online learning, we will use directed pre-reading and watching of broadcasts and pre-recorded material combined with ‘live’ timetabled teaching sessions which we expect you to attend via Zoom or Blackboard Collaborate. Where possible all ‘live’ timetabled sessions, whether online via Zoom/Collaborate or on campus in person will be recorded in order that any student unable to attend will be able to access the material. This may also serve others well for revision purposes.
- Online learning sessions: you are expected to attend and fully participate in the scheduled ‘live’ or ‘synchronous’ sessions as they appear in your timetable, via Zoom or Collaborate. Links to all scheduled Zoom/Collaborate sessions will be provided by individual course unit leads on the unit-specific timetables on course unit pages in Blackboard. Expectations for professional conduct for all Zoom teaching sessions for staff and students are as follows:
- You must be ready to join the Zoom session 5 minutes before the start time (just as you would for traditional lectures), in order that the lecturer can start the teaching on time, without the disruption of late arrivals.
- You should ensure your full name appears with your image on screen as courtesy to others, to facilitate participation in the session and so that we can monitor attendance.
- You should arrive on time and switch on your camera so you are visible to others but switch your audio off (mute) to begin the session (you may need to switch off your camera due to broadband issues, but you need to at least introduce yourself on camera)
- You should be fully dressed, indoors and sitting in a quiet space, with as few distractions as possible. If you are using a bedroom as your study space, then you may be sitting on the bed, but it is expected that you will not be in bed.
- You should ensure that no children or other household members appear in shot as most sessions are to be recorded.
- The same regulations apply to attendance as always (see Programme Handbook). You should email both the unit lead and/or lecturer leading the session you will miss and hcs.attendance@manchester.ac.uk if you are unable to attend any scheduled session, whether online or on campus.
- Student Support and Communications: your welfare under such unusual circumstances is more important to us than ever before. We fully appreciate the additional pressures upon you. You should contact your Academic Adviser in the first instance or ryan.hurst-2@manchester.ac.uk in order that we can ensure you have the support you need to progress with your studies. You should use your university email address, check your emails daily and use email as the means of making contact with all staff (email addresses in handbook).
- Assessment: all assessment will be completed by you online. In practice, this means little change to the nature of assessment for each course unit. Your learning in some course units is already assessed by assignment which is submitted online via Turnitin, so this will not change. For other course units, which may have used traditional exams or presentations, the assessment has been amended so that it can be completed online instead. You will be provided with clear information about assessment for each course unit lead. If you are at all unclear as to what is expected, you must ask the unit lead to be clear or ask the Programme Director for greater clarity.
- Placements: we plan to go ahead with block placements in physical settings across the Northwest region in 2020/21 as usual. The University, in collaboration with our partner placement providers are working very hard to ensure that students are supported to complete their placements safely and with the usual excellent learning opportunities that our varied clinical settings provide. Mindful of the vulnerability of clinical placements if we experience a second wave of the virus and further extensive lockdown, we are keen to augment your clinical learning in various ways, in order that you are well placed to complete your required clinical competencies, even if your placements are affected in the coming year.
NB *While we will endeavour to continue on-campus sessions throughout the year, we will clearly need to revert to online learning here too, in the event of return to complete lockdown. As you are aware, government guidance continues to change on a regular basis. While we will endeavour to adhere to the above planning as far as possible, it is subject to change as we continue to follow government guidance to keep students, staff, the public, our patients and their families safe during this ongoing global pandemic. If there are any changes to timetabled sessions, we will ensure that you are updated.
SECTION 1 INTRODUCTION
Welcome Message from the Programme Director
Welcome to the profession of Healthcare Scientist (Audiology). Congratulations on being selected as someone who has demonstrated excellent potential to develop and achieve both academically and clinically to become a healthcare professional we can be proud of. As a trainee Healthcare Scientist in the field of Audiology you are joining a team of dedicated, hard-working people, committed to supporting the health needs of people with communication, hearing and balance difficulties. We expect you will have high expectations of this degree programme and high expectations of yourself as you dedicate three years to preparing yourself, with our support, to become an independent healthcare professional, worthy of the title, ‘Healthcare Scientist’. Clearly the journey from first year student to qualified practitioner is a long and challenging one. We will endeavour to ensure that you are equipped with the necessary study skills, knowledge and understanding to take you further as you progress through the programme. Nevertheless, success on a demanding, vocational degree programme involves a great deal of commitment and sustained effort on the part of you as a student. You will become very familiar with the terms ‘independent learner’ and ‘enquiry-based learning’ whereby you are expected to be the driving force behind your own learning experience. If you are to be a respected clinician and/or researcher at the end of your training and throughout your career, able to work autonomously and keep up to date, then you need to be clear from the outset that you need to take responsibility for your own learning.
We endeavour to support you and to ensure that you are equipped and fully prepared intellectually, practically and emotionally for the many challenges you will face as a student healthcare scientist. You will need physical good health, mental agility and emotional resilience to negotiate the tremendously varied and demanding learning experiences of this healthcare programme. In Section 4 of this handbook, you will find more detail as to our programme philosophy in terms of student support and guidance.
From the University of Manchester’s Strategic Vision 2020, one of the University’s three core goals is “To provide a superb higher education and learning experience to outstanding students, irrespective of their backgrounds, and to produce graduates distinguished by their intellectual capabilities, employability, leadership qualities, and their ability and ambition to contribute to society”
In order to achieve this goal your learning journey with us is a partnership between the University and yourselves with expectation from both sides For more information on commitments from the University, and the commitments that you are signing up to see the University of Manchester Student Charter:
http://www.yoursay.manchester.ac.uk/student-charter/
I sincerely hope you enjoy your three years of studying with us here in Manchester and that your passion for the subject grows as you acquire more knowledge and skills.
Best wishes,
Dr Tim Wilding
Programme Director
BSc Healthcare Science (Audiology)
How to use this Programme Handbook
This programme handbook is absolutely central to your studies. You should endeavour to carry it with you, as you will need to refer to it frequently (an electronic version is available on Blackboard). It provides you with key information about the degree content, how your work is assessed, what is expected of you as a student and what you can expect from staff. It directs you to other useful sources of information. It is, in part, a record that you keep of exactly what you studied across the 3 years.
Keeping a Record
During your studies, especially in the first year, you will receive a great deal of information both in paper and electronic format. This will include handbooks of various kinds, timetables, handouts, email communications, appointments (with academic and administrative staff, occupational health, library staff, clinical teams, other students and others). One of the key factors that will make your life as a student easier is being organised.
Handy-tip: Organise your paperwork and keep your diary up-to date at all times.
It is important for you to have an accurate record of exactly what your cohort has studied: apart from your transcript of marks, future employers, particularly in other countries, may like more detail of your course content. In the first few sections you will find general information about the degree programme and how it all fits together, providing general guidance on the degree programme itself, how your work will be assessed and what the main sources of support for you are as a student. The appendices provide more detailed, specific information. Appendix 1 contains the course unit outlines for each course unit you will take in the first year. Updates to the Programme Handbook will be provided in electronic format in subsequent years, along with course unit information for those years. Because changes may occur from year to year so it is important that you keep hold of all 3 programme handbooks (electronic copies only will be available for year 2 and 3).
Handy-tip: Make sure you keep copies of your programme and other handbooks.
The History of Audiology and Deafness at Manchester
In 1919 the Department of Education of the Deaf was founded by Sir James E Jones in memory of his deaf son, Ellis Llywd Jones, and was one of the first such departments in the world. Since that time Manchester has played a major role in the development of audiology and deaf education both nationally and internationally. In 1974 the training of speech and language therapists began and thus the group were unique in the country in providing training programmes for teachers of the deaf, audiologists and speech and language therapists within the same department.
Since the creation of the new University of Manchester in October 2004, The Audiology and Deafness and Speech and Language Therapy groups moved from the Faculty of Education to the School of Health Sciences in the new Faculty of Medical and Human Sciences.
In the 2014 Research Excellence Framework, the system for assessing quality of research in UK higher education institutions, we were reviewed within Unit of Assessment 3 (Allied Health Professions) and ranked first in the UK (out of 94 submissions) in terms of research power.
Handy-tip: For more details on the research we do visit the ManCAD web page at http://research.bmh.manchester.ac.uk/mancad
The University
On 1 October 2004, the Victoria University of Manchester and University of Manchester Institute of Science and Technology (UMIST) joined forces to create The University of Manchester, a new university which aimed to unite the strengths of the two former institutions. The academic structure of the University of Manchester is made up of Faculties and Schools. There are three Faculty of Biology, Medicine and Health, Faculty of Science and Engineering and Faculty of Humanities
The Faculty of Biology, Medicine and Health (FBMH)
In 2015, the University took the strategic decision to merge the Faculty of Biology, Medicine & Health with the Faculty of Life Sciences in order to take full advantage of the world-leading basic biomedical and translational/clinical research strengths present in both Faculties, by creating a unified structure. Creation of the merged Faculty of Biology, Medicine and Health, which will commence operations in August 2016, will be a key component of the University’s mission to be among the top 25 research universities in the world by 2020.
The single Faculty structure will also concentrate the teaching of biological sciences, medical sciences, healthcare professional training, and provide outstanding opportunities for recruitment and training of junior scientists in a broad range of disciplines.
The current Faculty of Biology, Medicine & Health is a leading international centre for research and education in medicine and a spectrum of health-related professions including nursing, midwifery, social work, pharmacy, dentistry, psychology, audiology and speech and language therapy. We are the largest supplier of healthcare graduates to the National Health Services within the North West of England and many of our graduates go on to deliver healthcare provision across the globe.
We have a diverse portfolio of the highest quality teaching and research activity, represented through our component Schools and Institutes. Our scale, breadth and structure provide outstanding opportunities for basic biomedical research discoveries to be rapidly translated into effective new therapies with a strong emphasis on knowledge transfer and partnerships with industry. Our academics have the benefit of access to the large, stable population in the North West providing unique opportunities to study and address most causes of disease and deprivation. The opportunities are further enhanced by strong links to our partner Faculties and the NHS.
Handy-tip: For more details on the faculty visit: https://www.bmh.manchester.ac.uk/
Division of Human Communication, Development and Hearing (HCDH) – School of Health Sciences.
The Head of School is Professor Kay Marshall , who is a pharmacist. There are three Schools in the new Faculty of Biology, Medicine and Health. The Division of Human Communication, Development and Hearing sits within the School of Health and spans the disciplines of developmental psychology and psycholinguistics, child speech and language therapy, and hearing health, audiology and deaf education.
For further information about the see the website links below:
Handy-tip: For more details on the faculty visit: https://www.bmh.manchester.ac.uk/speech-hearing
The Programme
Programme context and outline
The BSc (Hons) Healthcare Science (Audiology) programme is a 3 year programme of entry level training for clinical audiologists within the NHS. Audiology is one of the Healthcare Science disciplines that fall under the Department of Health’s “Modernising Scientific Careers” (MSC) Programme.
“Audiology – healthcare scientists measure and evaluate people’s hearing and balance, fit and adjust aids, and offer therapeutic techniques to improve the quality of people’s lives. They work with children or adults as well as special needs groups, and are involved in the delivery of long-term treatment, management and care.” (NHS Web Site)
Within the MSC framework Audiology is grouped with Neurophysiology and Vision Sciences and elements of these areas will also form part of the first year of this programme. While the degree falls within the Neurosensory division of the MSC framework, the programme of study at University of Manchester only allows graduation with the Audiology specialism. Manchester Metropolitan University (MMU) delivers the BSc (Hons) Healthcare Science (Neurophysiology) degree and there will be some joint teaching with MMU in the 1st year of study.
The programme covers theoretical, practical and clinical aspects of audiology and related neurosensory topics. Academic components are studied throughout all three years. In years one and two, substantial practical skills training takes place in the well-equipped laboratories and clinics. Supervised clinical education and practice takes place within placement environments during each of the three years.
The general structure of the programme covers the more generic healthcare science topics and professional issues in year one, with core audiology topics in year 2 and more specialist audiology topics in year 3.
Year 1: Professional Issues; Basic Healthcare Science (including general anatomy and Physiology); Anatomy, Physiology and Pathophysiology of the neurosensory systems; Clinical measurement and treatment and Physics and Measurement. Year 1 also includes clinical placements in Audiology and learning experiences inNeurophysiology and Vision Science Disciplines.
Year 2: Professional Issues; Research Methods & Statistics; Audiological Science; Adult Audiological Assessment and Management; Hearing Aids; and clinic placement and practical skills education. Throughout semesters 1 & 2 you will undertake 2 days per week clinical placement with additional placements taking place during vacations. Further details of these are available in the clinical handbooks.
Year 3: Professional Issues; Research Project; Adult Rehabilitation; Advanced Hearing Aids; Paediatric Audiology; Tinnitus; Vestibular Assessment and Management. From January you will undertake a final 22 week clinic placement..
Accrediting and other organisations
Upon completion of the honours degree programme BSc (Hons) Healthcare Science (Audiology) graduates are eligible to apply for registration as Healthcare Science Practitioners and/or Hearing Aid Dispensers.
- NHS Healthcare Science (Audiology)
This programme is a professional qualification developed in response to the Department of Health’s ‘Modernising Scientific Careers’ (MSC) Programme. The programme is subject to accreditation by ‘Health Education England’. Graduates of the programme will be eligible to register as a Healthcare Science Practitioner in Audiology. The Programme was accredited in May 2012, with the accreditation visit taking place on 4th May 2012. This accreditation means that graduates with a BSc (Hons) Healthcare Science (Audiology) are able to work as Healthcare Science Practitioners in Audiology within the NHS.
For further details about Healthcare Science Careers see: http://www.nhscareers.nhs.uk/hcsci.shtml
For further details about audiology as a profession see: http://www.baaudiology.org/
Other relevant organisations include:
- The National School of Healthcare Science (http://www.nshcs.org.uk/)
This is the body that oversees the running of healthcare science programmes. The School implements the NHS healthcare science training programmes and quality assures the training and delivery.
- The Academy for Healthcare Science (http://www.ahcs.ac.uk/)
“The Academy of Healthcare Science is the overarching body for the whole of the Healthcare Science Profession, working alongside the specialist professional societies.
We work to ensure that Healthcare Science is recognised and respected as one of the key clinical professions in the health and care system, including working towards statutory regulation or all our staff groups to ensure protection for the patients we serve.” (AHCS Website)
- Hearing Aid Dispensers
The BSc (Hons) Healthcare Science (Audiology) programme has also been approved by the Health and Care Professions Council (HCPC) which is the statutory regulating body for a range of 15 different health professions including Hearing Aid Dispensers. This HCPC approval of the programme allows graduates with a BSc (Hons) Healthcare Science (Audiology) degree to apply for registration with the HCPC in order to work as a Hearing Aid Dispenser.
For further details see the HCPC web site: www.hcpc-uk.org
For further details about Hearing Aid Dispensers see www.bshaa.com
Associated organisations
The professional body for Audiologists in the UK is the:
British Academy of Audiology (BAA); www.baaudiology.org
The professional body for Hearing Aid Dispensers in the UK is the:
British Society of Hearing Aid Audiologists; www.bshaa.com
Career opportunities
Successful completion of this programme provides you with a BSc (Hons) Healthcare Science (Audiology) degree and a clinical qualification. This enables you to register as an audiologist and to work in the NHS and be eligible to apply for registration with the HCPC in order to work as a Hearing Aid Dispenser in the independent sector.
This programme of study will also allow for a number of other career opportunities. Previous graduates of the BSc Audiology have undertaken further programmes such as MSc in Advanced Audiology, MSc Clinical Science, or gone on to study for a PhD. Other students have entered the fast-track medicine programme, dentistry and other health related professions. Further career opportunities include research in universities or research institutes or employment in private sector audiology services and the audiology industry.
Handy-tip: The BSc Healthcare Science (Audiology) programme opens up a range of career opportunities please familiarise yourselves with the various organisations mentioned above to help you put this programme into a wider context.
People and Resources
Section 4 of this handbook provides more detail regarding student support and guidance, but here, at a glance, is a brief guide to key people. The Programme director (Dr Tim Wilding) is responsible for overseeing the running of the programme. You may approach the programme director about any academic or personal matters affecting your studies (however, see the section “Where do I get Help”).
The administration team are responsible for the day to day administration of the undergraduate degree programme and are available as a source of information and support for you while you are studying. Please contact them if you need any general information or material related to the programme or if you need to leave a message for any academic staff delivering the programme. They can be contacted on 01612758584 and are based in The Zochonis Building, Room G.15.
The Undergraduate Examinations & Assessments Administrator (Jonathon Kirk) is responsible for the administration of examinations and assessments and is also based in the Zochonis Building (Room G.15). Please contact her regarding hand-in of assignments, exams, results, extension requests or mitigating circumstances.
The Clinical Administrator (Caroline Spivey) is responsible for the administrative organisation around clinical placements for the undergraduate degree programmes in Communication and Deafness.
The Student Support Administrator (Ryan Hurst) is responsible for providing support to students or directing them to services which can offer the right kind of support for all manner of personal or academic matters affecting studies.
Facilities and Resources in the Ellen Wilkinson Building
The Undergraduate Office is in room G.15 on the ground floor of the Zochonis Building, Brunswick Street (Building 60 on the Campus Map). The undergraduate programme administrator Sadie Rose and other administrative staff are based in this office. They will try to answer your queries if possible. The office is normally open 9.00am – 5.00pm Mon-Fri during term time; opening hours may vary during vacation periods. The office may close for a short period of time at lunch time or because of training sessions and meetings.
The notice boards are in B block on the ground floor next to BG16.
The School of Health Sciences Student Hub is on the ground floor of Zochonis building, which is where central administration for the School and also the Head of School is based.
The Blackboard Virtual Learning Environment
Blackboard is an virtual learning environment is one of the most important learning resources that you will have access to and is used for a wide range of purposes including, but not limited to:
- A repository of information for students to access online. It is the policy of the audiology group to aim to provide electronic copies of all lecture notes and other material such as handbooks which are made available to the students via Blackboard. Please note, that Academic Staff use a range of teaching styles and some may provide comprehensive lecture notes whilst other might be quite minimal.
- Providing “Discussion Boards” both for students to discuss aspects of the course with each other and for specific course unit related discussions.
- Online assessment and feedback.
- Structured online learning material including online lectures.
- Provision of revision material or additional learning resources.
- Links to lecture podcasts or pre-recorded lectures.
- A wide range of other learning resources.
It is important that you familiarise yourselves with the facilities of Blackboard so that you can access the material provided. Paper copies of lecture presentations will not be given out, but will be made available in electronic format on Blackboard. Most written assignments will also be submitted through Blackboard to streamline the submission process and to run the assignments through plagiarism detection software.
Handy-tip: Familiarise yourself with the Blackboard Virtual Learning Environment – there are also iPhone and Android apps to access this system
- Blackboard Programme Space
Within Blackboard you will have access to a BSc Healthcare Science (Audiology) programme space that can be accessed by all three years studying on the programme it is this area that contains material such a Programme Handbooks, Timetables and other material that are relevant to all three years.
- Blackboard Unit Spaces
Each course unit has dedicated spaces on Blackboard that contain the much of the necessary learning material and other resources for that course unit. Please note, that the material provided on Blackboard is a learning resource, but does not replace other resources that you are expected to engage with such as library resources and electronic journal resources. The expectation is that the lectures (and associated notes) are a starting point for your learning, with supporting material provided on Blackboard, but that the majority of your learning will take place through private study using additional resources such as directed and recommended reading. The emphasis on this private study will develop more and more as you progress through the course.
Handy-tip: Familiarise yourself with the course unit spaces on Blackboard before you start a course unit so that you know where all the resources can be found.
The University of Manchester Library
The University of Manchester Library has a wide range of learning resources, not just books. These include eBooks and eJournals, access to reading lists, printing facilities, IT support Desk, battery charging stations, iPad and laptop loans, and study-skills material and workshops.
Handy-tip: Familiarise yourself the library (both the Building and web site) – a good place to start is: http://www.library.manchester.ac.uk/.
But a key resources is:
http://www.library.manchester.ac.uk/services-and-support/students/support-for-your-studies/my-learning-essentials/
Where do I go for help?
The following table lists sources of information for various matters of concern:
| Matter of concern | Where to look/who to speak to |
Academic Matters:
|
Programme Handbook Blackboard Individual Course Unit Lecturer Your Year Rep if a matter for all students Examinations Administrator Academic Advisor Programme Director |
Clinical Matters:
|
Clinical Handbook Blackboard Individual Clinical Educator on placement Clinical Team Clinical Administrator |
Personal Matters:
|
Academic Advisor (see Section 4) Individual Lecturers if lectures missed Programme Director Programme Administrator |
Administrative Matters:
|
Blackboard Undergraduate Office |
| IT Matters: | IT Services web site |
| Library Matters: | See http://www.library.manchester.ac.uk/services-and-support/students/ |
Staff Availability
Most staff operate an open door policy where you can knock on their door any time during the week and either see them then, or arrange an appointment. Some staff may however operate an office hours system and post their ‘office hours’ on their door or. These are the times each week when they are available for drop-in enquiries. You can of course arrange to see staff outside these times but we ask that you make an appointment by phone or email to be sure of finding a time convenient for everyone.
Staff Contact Details*
| Name | Position | Room | Tel | ||
| Dr. Richard Baker | Reader | B2.14 | 275-3388 | richard.baker@manchester.ac.uk | |
| Dr. Siobhan Brennan (PT) | Lecturer | B2.1A | 275-8677 | siobhan.brennan@manchester.ac.uk | |
| Debbie Cane (PT) | Lecturer | B2.13 | 275-8679 | debbie.cane@manchester.ac.uk | |
| Dr. Piers Dawes | Senior Lecturer | A3.09 | 306-1758 | piers.dawes@manchester.ac.uk | |
| Alison Edwards (PT) | Lecturer, Deputy Clinical director | B1.2 | 275-3454 | alison.edwards@manchester.ac.uk | |
| Dr Antje Heinrich | Lecturer, Recruitment officer |
B2.13 | 275-8679 | antje.heinrich@manchester.ac.uk | |
| Ryan Hurst | Student Support Officer | G15 Zochonis | 275-7332 | ryan.hurst-2@manchester.ac.uk | |
| Saira Jackson | UG Programmes Manager | G.08 Zochonis | 275-2559 | saira.jackson@manchester.ac.uk | |
| Dr. Karolina Kluk-de Kort | Senior Lecturer | B2.7 | 275-3371 | karolina.kluk@manchester.ac.uk | |
| Dr Rebecca Millman | Lecturer | B2.8 | 255-3387 | rebecca.millman@manchester.ac.uk | |
| Dr Garreth Prendergast | Lecturer, Exams officer | TBC | TBC | garreth.prendergast@manchester.ac.uk | |
| UG Programmes Administration Team | G.15 Zochonis | 275-8584 | |||
| Dr. Elizabeth Sheader | Senior Lecturer | 1.124 Stopford | 275-3881 | elizabeth.a.sheader@manchester.ac.uk | |
| Bridget Goodier (PT) | Clinical Director | B1.17 | 275-3434 | bridget. goodier@manchester.ac.uk | |
| Jonathon Kirk | Examination & Assessment | G.15 Zochonis | 306-0449 | jonathon.kirk@manchester.ac.uk | |
| Caroline Spivey | Clinical Administrator | B1.15 | 275-3370 | caroline.spivey@manchester.ac.uk | |
| Dr. Kai Uus | Reader | B2.1 | 275-8282 | kai.uus@manchester.ac.uk | |
| Keith Wilbraham | Experimental Officer | A4.12 | 275-3253 | keith.wilbraham@manchester.ac.uk | |
| Dr. Timothy Wilding | Lecturer, Programme Director | B2.10 | 275-8286 | tim.wilding@manchester.ac.uk | |
| Dr Helen Glyde (PT) | Lecturer | B2.7 | 306-1757 | helen.glyde@manchester.ac.uk | |
* Please note, this list does not include all the staff that you will come across during your studies. Throughout your studies you will come across a wide range of other academic and support staff, including clinicians and patients. PT = part-time
Code of Conduct and Behaviour
As trainee health care professionals, it is very important that you behave in a manner consistent with the ethics and values expected of your profession, especially when interacting with other professionals or patients. You will be expected to follow the Code of Professional Conduct (details in Clinical Handbook) and will be asked to read and sign this Code indicating you understand and agree to behave as a professional. In addition, some general ground rules are given in the Appendices of this handbook. Do take time to read these ground rules and keep them in mind when you are involved in your professional business, especially when on clinic placements.
Attendance expectations
As a programme that is preparing you for a professional role in as Healthcare Scientists, the expectation is that you show dedication to your learning and studies, and with that in mind there is an expectation not only of 100% attendance at all scheduled sessions, but that punctual in attending these sessions. However, we understand that illnesses or other circumstances do occur that may mean you miss, or are late for a session. All that we ask in such situations is that you notify us using the appropriate procedures. If these procedures are followed then we are able to keep records and support students who may be having difficulties.
Attendance Policy
Attendance is taken very seriously on this vocational degree programme (see above re conduct). It is a requirement that you attend all scheduled campus sessions for any individual course unit and a 80% minimum attendance requirement across the duration of each course unit is imposed. It is a requirement that you attend 100% of practical class sessions. It is a professional requirement that you attend 100% of clinical placement sessions, for further information please see your Clinical Handbook. If your attendance at a particular course unit is deemed unsatisfactory, you may not be permitted to complete the assessment and/or awarded the credits for that course unit, which would mean you would not be able to progress and you would have to leave the programme.
In order to support academic attainment and monitor wellbeing, Academic Advisors will be given regular updates of their personal student’s attendance profiles. Students who reach trigger points (detailed below) will be flagged to their Academic Advisor. The role of the Academic Advisor in attendance monitoring is a supportive one, to ensure that students are well and engaging with the programme. Academic Advisors will treat cases of poor attendance on an individual basis and agree to a range of actions. These may include regular meetings, referral to Occupational Health or revisiting guidance on the attendance requirements.
Registers and Attendance Recording
Because of the attendance requirements of this programme we pass registers around at the beginning of each session. It is your responsibility to make sure that you sign the registers so that your attendance is recorded appropriately. The registers are usually collected in after they have been signed, so if you are late you may me marked in as late, or absent if you are very late. However there is often a temptation to ‘sign in’ for a friend who isn’t going to attend, or who is going to be late – do not do this, do not ask someone to do this as such behaviour is dishonest, it also prevents us from identifying some genuine situations where students may require extra support.
If you need to leave the lecture early for a valid reason, for example to attend a medical appointment, then please inform the class tutor that you are leaving. Signing the register in indicating that you are present in class but then leaving part way through a lecture without notifying us is unacceptable.
From time to time we may take a register of those present both at the start and end of a class.
Handy-tip: Make sure you sign the register, but for yourself only. If you forget to sign the register you will be marked as absent. Do not ask the session tutor to allow you to sign it at a later date as that is not permitted. It is the student’s responsibility to ensure that their attendance is properly recorded.
Legitimate mitigating circumstances for absence and how to notify
If you are unable to attend a scheduled session for any course unit you must email the attendance team using hcs.attendance@manchester.ac.uk and copy in the unit lead for the session you are missing and your academic advisor. You must include the unit code of the session you are missing and the reason why you will not be attending. You must ensure that you notify the attendance team as early as possible BEFORE the session you are due to miss. You need to report an absence for each day that you are unable to attend unless you have provided a doctor’s note. Absences longer than two consecutive days must be reported to your academic advisor using the self-certification form. Absences expected to last longer than the self-certification period of one week need to be supported by a doctor’s note, or academic advisor signature for other authorised absence reasons. Failure to report absences in the correct way may result in your absence being recorded as unauthorised. If you are ill while on placement and so need to be absent at all from placement, please notify your Practice Educator and the Clinical Director (Bridget Goodier) as soon as possible. You must self-certify or provide a sick note just as you would at any other time during your studies.
Please note that simply notifying us of your absence does not mean that your circumstances for absenting yourself will be regarded as legitimate. Absence for reasons other than genuine illness, attending medical appointments, difficult personal circumstances or religious/cultural reasons will be recorded as unauthorised absence. These include: weekends away; holidays; social functions or sporting events; weddings; part-time jobs; catching trains, planes etc. You may choose to tell staff of your intended absence. However, we cannot authorise any such absence or grant you ‘permission’ to miss teaching sessions for such reasons. You are adult learners and, in the full knowledge that full attendance is an expectation, you may still choose to prioritise other events. As stated above, a record of your attendance will be kept routinely and any periods of absence will be kept on file for future reference. Whatever the reasons for repeated or prolonged absence, if it is deemed to be having an impact or potential impact on your studies or professional practice, then you will be offered tutorial support.
Please note that if you do not sign the register for a particular teaching session you will be marked as absent. If a register is not available, please ask the lecturer or notify the undergraduate office immediately after the lecture. It is your responsibility to sign the register.
You MUST PROVIDE SUPPORTING EVIDENCE if attendance at an exam or assessments are missed due to illness or particularly difficult circumstances. The documentary evidence (perhaps a medical certificate or letter from another professional person or third party involved) should specifically cover the date(s) of the examination(s) or assessment(s) concerned. See later in this section under ‘Mitigating circumstances affecting work and assessments’. You must notify the Exams Administrator if you miss an exam.
Handy-tip: If you are absent for any reason let us know, making sure you give the reason. You must complete a self-certification of absence form for absences of more than two consecutive days. Absences of longer than a week (7 consecutive days) require a medical certificate, or Academic Advisor’s signature for other agreed reasons. Forms are available on Blackboard.
Procedure for managing unsatisfactory attendance
The expectation is that students will attend 100% of timetabled activity. As stated above, students may not be allowed to sit assessments if their attendance falls below 80% in any course unit. A ten credit course unit normally has twelve lectures as a minimum (this differs between course units). The 80% attendance rule means that only two (of twelve) timetabled lectures/tutorials can normally be missed. Non-attendance at any two timetabled sessions within any course unit for any reason (including authorised absence owing to illness or other reasons) is of concern. Students missing any two timetabled sessions within any course unit may be required to meet with their academic advisor to discuss the implications of the absence, and for support.
If a student fails to attend four or more timetabled sessions (regardless of which units) on four or more dates within a semester (without notifying via the specified channels of communication their legitimate mitigating circumstances as stated above), or, in the case of a unit which runs the whole year, on four or more dates across both semesters, the formal warning procedure will be instigated as follows:
- First Warning: a warning letter is sent to the student, outlining our concerns regarding their attendance and requesting that the student make contact with her/his Academic Advisor in order to address any issues which may be affecting attendance. This letter is intended to support the student to improve their attendance record. If attendance is improved, no further letter will be issued. The Student Progress Committee will be informed.
- Second Warning: if unsatisfactory attendance persists, a second warning letter is sent to the student. This letter warns the student that, due to persistent poor attendance, their attendance for individual course units will henceforth be scrutinised. If attendance is deemed satisfactory, no action will be taken. The Student Progress Committee will be informed.
- If attendance in any single course unit falls below the required level, then the student’s case will be referred to the programme Student Progress Committee. It is the decision of the Student Progress Committee as to whether the student will be permitted to sit the assessment for any unit for which attendance is unsatisfactory.
Patterns of repeated absence, high-levels of absence, frequent poor punctuality, or extended periods of absence will be investigated and could result in referral to progress committee, occupational health, or other support mechanisms to ensure continuing fitness to study and attend clinical placement. It should be reiterated that persistent non-attendance may result in the student not being permitted to take the assessments for the course unit in question, which may ultimately signify exclusion of the student from the programme, as passing of all course units is mandatory in order to progress.
Clinical placement attendance
All clinical placements are a compulsory part of the course and must be attended. University (see above) and Clinic Placement non-attendance procedures must be followed in the event of valid reasons for non-attendance occurring (health/special circumstances). Every effort will be made to arrange additional placement opportunity to make up for significant lost placement time for students who have not been able to achieve satisfactory clinic placement attendance for valid reasons (mitigation). In such cases special arrangement may apply, and course progression could be delayed.
It should be noted that it may not always be possible to arrange clinical placements during normal placement periods for any student depending upon capacity. Students returning from interruption, or those who have special requirements (health/disability/caring responsibilities) may need a bespoke placement plan which requires different placement patterns to enable them to meet the course clinical placement learning outcomes. In some cases course progression could be delayed in ay special arrangement apply.
Handy-tip: If you are absent from Clinic placement for any reason you must notify the University following the absence notification procedures stated above AND notify your clinical placement team by following their absence procedures.
Late arrival for teaching sessions
Punctuality and ability to organise your own schedule are important aspects of professional behaviour. It is expected that all students will be present at each scheduled teaching session (lecture, practical, tutorial, academic-advisor meeting) BEFORE THE START of that session. Staff have been instructed to take in registers at the beginning of the session so that we can monitor lateness. Staff may set their own rules regarding late entry to classes, please follow any rules that they inform you of. We understand that many students commute and rely on public transport which can cause lateness if there are unexpected delays. We recommend students plan their journeys carefully to allow for delays to ensure punctuality. It is better to plan to arrive early to avoid the risk of being late. Students arriving early can make use of the wide range of on-campus facilities available. Repeated patterns of lateness will be investigated so that appropriate support can be provided. Students repeatedly arriving late may be referred to progress committee.
Late arrival and non-attendance to practical laboratory based sessions
The tutor teaching the practical class has the right to refuse admission to latecomers. This is because students need to be present at the instructional part at start of practical classes. In the event of non-attendance for any reasons, it is the student’s responsibility to obtain permission to attend at alternative appropriate time (different group). Students repeatedly arriving late, or not attending, practical classes may be referred to progress committee.
Students who fail to attend their allocated practical session without prior arrangement and/or do not provide mitigating circumstances may be subject to a 10% reduction in their marks for this course unit.
Late arrival to clinical placement
Punctuality and ability to organise your own schedule are important aspects of professional behaviour. It is expected that all students will be present at each scheduled clinical placement day, or session, BEFORE THE START of that session. Late arrival at clinical placement without a valid reason is unacceptable. Students repeatedly arriving late to, or not attending, clinical placement may be referred to progress committee.
Handy-tip: Arrive at least 5 minutes before each scheduled session so that you are prepared for a prompt start.
University Policies
In addition to the information laid out in this handbook (and the Clinical Handbook), there are various University Policies regarding various different aspects of student conduct (e.g. appropriate use of IT systems), Student disciplinary procedures, work and attendance etc. These policies can be found on the University web site at:
http://www.regulations.manchester.ac.uk/
Information from some of these University Policies is presented in this handbook, but please make sure that you are familiar with the range policies that are available at this site.
Teaching and Learning – A partnership
The BSc Healthcare Science (Audiology) is an intensive and rigorous programme designed to help you to develop into dedicated and motivated Healthcare Science professionals in the field of Audiology. As University Staff we are here to provide the teaching and educational resources for this development, both academically and clinically. However, it is important to view the programme as a partnership and remember that the staff are here to help. If there are any aspects that you don’t understand – chances are that others in the group also don’t – so please ask us.
To help make things clearer for you in terms of what is expected, each teaching session will have “intended learning outcomes” (ILOs) which should indicate the knowledge and understanding that you should have gained by the end of the session and after the appropriate reading. These ILOs should also help drive your revision for the various assessments.
Remember also, lectures and tutorials are only the beginning, reading lists are provided to support the lecture material. Some of this will be directed reading which may be specific chapters or papers to support the lectures, or it may be background, or more in-depth reading. It is important that lecture material is backed up by your own study – remember a 10 credit unit (100 hours study) may only consist of 12 hours of lectures; the rest will usually be private study of some sort.
Similar expectations are held regarding the practical sessions. These provide the basic skills that you will use and develop in the clinics, and are generally assessed by assignments and OSCEs (objective structured clinical examinations). While, the practical sessions teach the skills, it is only by extensive practice that you will become ‘fluent’ in carrying out the various tasks to the level expected in the assessment (and that expected by clinical placement teams). Failure to successfully demonstrate the necessary practical skills and knowledge may result in you not being able to continue on the BSc Healthcare Science (Audiology) programme.
Handy-tip: Make the most of your learning opportunities – don’t just think, how long will this session take – engage in your learning.
Student Charter
The University of Manchester’s Student Charter was established in 2012. One of the University’s three core goals is “To provide a superb higher education and learning experience to outstanding students, irrespective of their backgrounds, and to produce graduates distinguished by their intellectual capabilities, employability, leadership qualities, and their ability and ambition to contribute to society”. Our Student Charter, developed jointly by the University and the Students’ Union, is an important part of how we establish and maintain clear mutual expectations for the experience of all students: undergraduate, postgraduate taught and postgraduate research. It sets out what we can expect from each other as partners in a learning community. It can be read in full at the following link:
http://www.studentnet.manchester.ac.uk/enhancing-my-experience/charter/
SECTION 2 PROGRAMME OVERVIEW
The structure of undergraduate degrees and the credit rating system; course unit coding; the programme specification; summary of course units; summary of topics across all years.
The Academic Year
The academic year is divided into two Semesters: September to January and February to June. Semester 1 always starts with ‘Week 0’ or ‘Welcome Week’. Both semesters then have 12 weeks of teaching. At the end of each semester is an exam period lasting two or three weeks: Semester 1 exams are in January; Semester 2 exams are May-June. In addition, there is a resit exam period of two weeks in August-September each year.
Semester dates for the academic year 2020/21
| University welcome and induction programme | 21 September 2020 |
| School and programme induction activities | 28 September 2020 |
| Semester 1 teaching starts | 5 October 2020 |
| Christmas break starts | 21 December 2020 |
| Christmas break ends | 11 January 2021 |
| Revision period | 11- 17 January 2021 |
| Semester 1 exams | 18- 29 January 2021 |
| Semester 1 ends | 31 January 2021 |
| Break | 1- 7 February 2021 |
| Semester 2 starts | 8 February 2021 |
| Easter break starts | 29 March 2021 |
| Easter break ends | 12 April 2021 |
| Semester 2 exams | 19 May – 9 June 2021 |
| Semester 2 ends | 11 June 2021 |
The examination periods for 2020/21 are:
Semester 1: 18-29 January 2021
Semester 2: 17 May- 11 June 2021
Resits: 23 August- 3 September 2021
It is important that you make sure you are available for all exam periods, including the summer resit exam period, it is especially important that you do not book holidays during these periods.
Handy-tip: Make the most of your learning opportunities – don’t just think, how long will this session take – engage in your learning.
The FHEQ Credit Rating System
Every course unit of a degree is assigned a number of credits according to the Framework for Higher Education Qualification (FHEQ) system. A normal workload in one year for a full-time Honours student involves the completion of course units totalling 120 credits; 10 credits represent a nominal student workload of approximately one hundred hours. The workload may include teaching contact time, group, practical and clinical work, independent study, directed reading, assignment or presentation preparation, revision and examinations, as appropriate. Not only does the credit rating of a course unit tell you how much work you are expected to do in completing it, it also tells you the weighting of the course unit in the calculation of your year average or degree classification. Course units are weighted in exact proportion to their credit rating so that, for example, course units of 20 credits are weighted twice as heavily as course units of 10 credits.[1]
BSc Healthcare Science (Audiology) programme specification
(The following pages provide what is called the programme specification – this is a requirement for all programme handbooks and gives in-depth details of how the programme is structured)
Levels of study
In addition to credits, every course unit of a degree is assigned a level: 4, 5 or 6, reflecting the standard of work required. Level 6 corresponds to the standard normally found in the final year of a full-time undergraduate degree. These levels are those described by the Framework for Higher Education Qualification (FHEQ). Previously these were described as levels 1, 2 and 3. These FHEQ descriptors are also used in certain parts of the programme documentation.
Levels and credit ratings for each course unit are shown in the programme specification and in the individual course unit descriptions in Appendix 1 (and those provided online for subsequent years). You are awarded the credits for a given course unit on satisfactory completion of that unit (including attendance at lectures, practicals and clinics and any element of assessment). Level of study and expectations of student involvement are shown in the table below:
| Year | FHEQ Level | Credits | Expectations at this level |
| 1 | 4 | 120 | High achieving students with exceptional level of vocational commitment, prepared to work hard academically to establish a grounding in theory and basic clinical skills to set themselves up for future application to clinical practice; learning independent study: reading outside the scope of lecture notes. |
| 2 | 5 | 120 | Now equipped with the foundation to consider application of theory to clinical practice, and able to carry out the full range of clinical skills appropriate for their placements; well versed in independent study with a good understanding of the research bases for clinical practice; ready to read more widely on clinically-related subjects. |
| 3 | 6 | 120 | Thoroughly independent learners developing clinical autonomy and an ability to reflect upon and question the theory-practice link. Now equipped to critically evaluate the literature, identify gaps in the research and propose new areas of research. Ultimately graduate Audiologists: independent healthcare professionals, committed to lifelong learning by the process of Continued Professional Development and/or research. |
Credit requirements – BSc Healthcare Science (Audiology)
To obtain the clinical qualification in Healthcare Science (Audiology), and be eligible for registration as a Healthcare Science Practitioner in Audiology, or to apply for registration with the HCPC for the Hearing Aid Dispenser role, you must achieve the minimum number of academic and clinical credits as specified below:
| Degree | Min. credits (total) | Min. level 6 credits |
| BSc (Hons) Healthcare Science (Audiology) | 360 | 120 |
Exit Awards
For students who either fail to satisfy the requirements to proceed to a subsequent year, or who wish to withdraw from the programme before completion of the four years of study, the requirements for the different exit and award points are specified below. Please note that these are exit awards for students who have obtained the appropriate number of credits to enable them to exit at the end of the particular year. Thus, for example, if a student registered on the BSc (Hons) Healthcare Science (Audiology) decides that, having completed the 2nd year of study wishes not to carry on with their studies then they will be able to exit with a DipHE Healthcare Science Studies. Similarly, for example, a student who fails to complete the 2nd year will be eligible for a Cert HE in Healthcare Science Studies (if they have successfully completed the 1st year of studies).
| Name of Award | Min. UK credits for the award | Min. ECTS credits | Min. UK credits at the level of qualification | MinECTS | FHEQ level |
| BSc (Hons) Healthcare Science (Audiology) * | 360 | 180 | 120 | 90 | 6 |
| BSc (Ord) Healthcare Science | 300 | 150 | 60 | 30 | 6 |
| DipHE Healthcare Science | 240 | 120 | 90 | 45 | 5 |
| CertHE Healthcare Science | 120 | 60 | 90 | 45 | 4 |
Please note: achieving the required number of credits for an Honours or Ordinary degree is NOT the same as fulfilling the requirements for the honours degree in Healthcare Science (Audiology) with eligibility for registration as an Healthcare Science Practitioner or Hearing Aid Dispenser. You will be required to pass all specified academic and clinical elements of the degree (after resit arrangements have applied) in order to achieve eligibility for professional registration.
*Only the BSc (Hons) Healthcare Science (Audiology) is accredited for clinical practice as a Healthcare Science Practitioner.
*Only the BSc (Hons) Healthcare Science (Audiology) allows application to the HCPC for registration as a Hearing Aid Dispenser.
Course Unit Coding
Each course unit is given a separate code which contains letters followed by a series of numbers. The letters refer to the Faculty or Department with academic responsibility for that course unit. The first number indicates the year and the fourth number the semester in which the unit is taught:
1 = Semester 1
2 = Semester 2
0 = Semesters 1 and 2.
Examples:
HCDI 11501- a FHEQ Level 4 course unit, taught in semester 1 of year 1.
HCDI 21000- a FHEQ Level 5 course unit, taught in semesters 1 and 2 of year 2.
1. Background
The BSc (Hons) Healthcare Science (Audiology) is a 3 year undergraduate degree programme that has been developed in response to the Department of Health’s “Modernising Scientific Careers” (MSC) programme. This degree programme replaces BSc (Hons) Audiology which was the previous entry level pre-registration practitioner level training route for work in the NHS.
The DoH MSC programme presents 5 healthcare science divisions of which Neurosensory Sciences covers the Audiology specialism. In addition to Audiology, the Neurosensory Science division also covers Neurophysiology and Opthalmic and Vision Sciences.
| UCAS Code | Award | Programme Title | Duration | Mode of study |
| B610 | BSc (Hons) | Healthcare Science (Audiology) | 3 Years | Full Time |
| BSc | Healthcare Science * | 3 Years | Full Time | |
| DipHE | Healthcare Science * | 2 Years | Full Time | |
| CertHE | Healthcare Science * | 1 Years | Full Time |
* exit awards only – these awards do not allow professional registration as Healthcare Science (Audiology) practitioners or with the HCPC for the Hearing Aid Dispenser Role.
School |
Health Sciences |
Faculty |
Biology, Medicine and Health |
Awarding Institution |
University of Manchester |
Programme Accreditation |
Medical Education England (Healthcare Science Programme Board) – approved 2012). The BSc (Hons) Healthcare Science (Audiology) has been approved as a training route for registration as a “Hearing Aid Dispenser” |
| Relevant QAA benchmark(s) | Under development within the Health Care Professions group of benchmarks, but development of the BSc Healthcare Science (Audiology) has been guided by the benchmark statement: Health care programmes – Audiology |
Credit Framework
| Name of Award | Min. credit for the award | ECTS | Min. credits at the level of qualification | Min. ECTS credits at the level of qualification | FHEQ level |
| BSc (Hons) Healthcare Science (Audiology) | 360 | 180 | 120 | 60 | 6 |
| BSc (Ord) Healthcare Science | 300 | 150 | 60 | 30 | 6 |
| DipHE Healthcare Science | 240 | 120 | 90 | 45 | 5 |
| CertHE Healthcare Science | 120 | 60 | 90 | 45 | 4 |
2. Aims of the programme
The programme aims to:
| 01 | provide an appropriate educational and work-based learning experience in healthcare science (Neurosensory Science), and specifically Audiology |
| 02 | provide students with a broad knowledge and understanding of generic Healthcare Science and Neurosensory Science theory and principles |
| 03 | provide students with a broad, yet in-depth understanding of basic scientific aspects relating to the hearing and balance systems |
| 04 | provide appropriate learning opportunities for students to gain a comprehensive knowledge of hearing and balance and their disorders in adults and children, as required by the course’s accrediting body |
| 05 | provide students with a knowledge and understanding of how appropriate assessment and management strategies can reduce disability resulting from hearing or balance problems |
| 06 | provide a strong theoretical background that can be translated into thoughtful, reflective and quality practice |
| 07 | organise, monitor and evaluate a wide range of appropriate clinical experience within audiology, including skills in clinical interpretation and interpersonal skills in client management |
| 08 | provide students with understanding and ability to identify clients who need to be referred to rehabilitation and other services |
| 09 | provide a variety of learning experiences, to equip students with appropriate transferable skills |
| 10 | enable students to evaluate research critically and to provide them with the opportunity to develop basic skills in research |
| 11 | promote a commitment to professional development and lifelong learning |
3. Intended learning outcomes of the programme
| Should be able to show: | A. Knowledge & Understanding of/in: |
| A1 | Demonstrate knowledge of the learning resource facilities available to support their learning on the course and in future professional life, and how to make use of these facilities. |
| A2 | Demonstrate knowledge and understanding of basic scientific principles appropriate to developing careers as Healthcare Science (including basic physical and mathematical principles and principles of evidence based practice) |
| A3 | Demonstrate knowledge the underpinning areas appropriate to neurosensory sciences (including neurophysiology, vision science, audiology and more general aspects of healthcare science and public health). |
| A4 | Demonstrate knowledge and understanding of instrumentation, assessment tools and procedures available to assess the function of neurosensory systems. |
| A5 | Demonstrate in-depth knowledge and understanding of instrumentation, assessment tools and procedures available to assess the function of auditory and vestibular systems. |
| A6 | Demonstrate knowledge and understanding of a range of rehabilitation and management strategies appropriate for different neurosensory disorders. |
| A7 | Demonstrate in-depth knowledge and understanding of a range of rehabilitation and management strategies appropriate for auditory and vestibular disorders (including principles of communication and rehabilitation theory and practice, counselling , goal-setting and assessment of outcome) |
| A8 | Demonstrate knowledge of a range research principles and methodologies and understanding of the importance of research in Healthcare Science and the processes by which research is carried out. |
| A9 | Demonstrate a critical understanding of the role of Healthcare Scientists within the NHS and other sectors of healthcare provision (including NHS codes of practice and ethics, and the legislative framework for disability; the key quality assurance and service guidelines in audiology and related services supporting clients with hearing loss [including Hearing Aid Dispensers]). |
| Learning & Teaching Processes (to allow students to achieve intended learning outcomes) | Assessment (of intended learning outcomes) | |
| Lectures (A1-A9) | Formative assessments (A1-A9) | |
| Tutorials (A1-A9) | PADP (A1) | |
| Demonstrations (A1-A9) | → | Written exams (A1-A9) |
| Small group instruction (A1-A9) | Written Assignments (A1-A9) | |
| Practicals (A1-A9) | Presentations (A1, A2, A4-A9), | |
| Online Study (A1-A9) | IRCP/PPLA (A1-A8) | |
| Directed Reading (A1-A9) | Online assessments (A1-A9) | |
| EBL/PBL (A1-A9) | Research project/proposal (A1-A9) | |
| Clinical Practice Placements (NHS and other) (A1-A9) |
***
IRCP = Individual Record of Clinical Practice (National Online Logbook used in Audiology)
PPLA = Personal Portfolio of Learning and Application (Electronic Portfolio of Evidence). This includes formal records/evidence of DOPS and CBDs.
DOPS = Direct Observation of Practical Skills
Mini-Cex = Mini Clinical Examination (often referred to as OSCEs – Objective Structured Clinical Examinations)
CBD = formal case-based discussion.
| Should be able to show: | B. Intellectual Skills to: |
| B1. | Collect information on factual topics from a range of sources, and present it clearly and accurately expressed (orally or in writing) |
| B2. | Process, organise and begin to evaluate information on complex topics and present it in a logical argument, clearly and accurately expressed |
| B3. | Acquire and evaluate information from a range of sources; show understanding of the theoretical, statistical and methodological issues involved; present a clear discussion of the topic, justifying the chosen position by reference to the evidence considered. |
| B4. | Integrate knowledge acquired in different environments and apply it to decision making in clinical practice |
| B5. | Critically evaluate the research literature in order to understand and apply the research evidence base in Healthcare Science and Audiology |
| B6. | Reflect on their own learning and interaction styles and use this self-awareness to maximise their approach to learning and professional performance |
| B7. | Collect information on factual topics from a range of sources, and present it clearly and accurately expressed (orally or in writing) |
| Learning & Teaching Processes | Assessment*** | |
| Lectures (B1-B7) | Formative assessments (B1-B7) | |
| Tutorials (B1-B7) | → | PADP (B1, B2, B6, B7) |
| Demonstrations (B1-B7) | Written exams (B1-B7) | |
| Small group instruction (B1-B7) | Written Assignments (B1-B7) | |
| Practicals (B1-B7) | Presentations (B1-B7), | |
| Online Study (B1-B7) | IRCP & PPLA (B1-B7) | |
| Directed Reading (B1-B7) | Online assessments (B1-B7) | |
| EBL/PBL (B1-B7) | Research project/proposal (B1-B7) | |
| Clinical Practice Placements (NHS and other) (B1-B7) |
***
IRCP = Individual Record of Clinical Practice (National Online Logbook used in Audiology)
PPLA = Personal Portfolio of Learning and Application (Electronic Portfolio of Evidence). This includes formal records/evidence of DOPS and CBDs.
DOPS = Direct Observation of Practical Skills
Mini-Cex = Mini Clinical Examination (often referred to as OSCEs – Objective Structured Clinical Examinations)
CBD = formal case-based discussion.
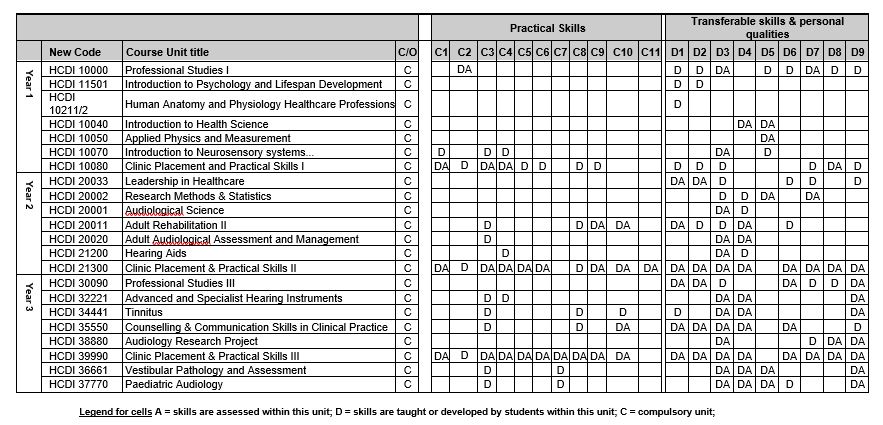
| Should be able to show: | C. Practical Skills to: |
| C1. | take an observational role in neurosensory clinics (Neurophysiology, Vision Science and Audiology) |
| C2. | basic mandatory training requirements of clinical placements (inc. Infection control, manual handling, basic life support etc). |
| C3. | demonstrate skills in a range of audiological assessment procedures |
| C4. | demonstrate skills in hearing aid prescription, fitting and verification |
| C5. | take a supervised role in appropriate adult audiology clinics |
| C6. | undertake directed clinical practice in a variety of adult audiology, paediatric audiology and rehabilitation clinics |
| C7. | undertake adult and paediatric audio-vestibular and rehabilitation clinics with supervision |
| C8. | use basic knowledge of counselling skills to enhance clinical communication and decision-making |
| C9. | apply basic rehabilitative techniques in clinical practice |
| C10. | set goals and use outcome measures in rehabilitation |
| C11. | carry out appropriate audiometric calibration |
| See Clinical Handbook for more detailed breakdown of clinical objectives. Expected skills are also listed in more detail in the QAA subject benchmark statement for Audiology and the HCPC Standards of Proficiency for Hearing Aid Dispensers. It is expected that the above skills will be developed to a threshold level of expertise in that graduates will be able to practise as Healthcare Scientists and/or Hearing Aid Dispensers. |
| Learning & Teaching Processes | Assessment*** | |
| Practical and clinical Demonstrations (C1) | Formative Assessment (C1-C10) | |
| Online and Video presentations (C1-10) | Mini-Cex, practicals assessments (C2, C3, C4, C10) | |
| Practical classes, included directed practice(C1, C2,C3, C10), | IRCP, and Professional Development Portfolio, PPLA, Mini-Cex, DOPS, CBD (C1 – C10) | |
| Clinical placements and tutorials (C1 – C10) | → |
***
IRCP = Individual Record of Clinical Practice (National Online Logbook used in Audiology)
PPLA = Personal Portfolio of Learning and Application (Electronic Portfolio of Evidence). This includes formal records/evidence of DOPS and CBDs.
DOPS = Direct Observation of Practical Skills
Mini-Cex = Mini Clinical Examination (often referred to as OSCEs – Objective Structured Clinical Examinations)
CBD = formal case-based discussion.
| Should be able to show: | D. Transferable Skills and Personal Qualities to: |
| D1. | Develop and maintain effective working relationships, including effective functioning in a multi-disciplinary team. |
| D2. | Show awareness of their personal and interactional attributes and modify them as necessary in a professional environment. |
| D3. | Gather and evaluate information from a wide range of sources. |
| D4. | Make use of current research by evaluating it and applying it in clinical practice. |
| D5. | Understand, manipulate, analyse and present basic numerical and statistical information. |
| D6. | Demonstrate effective communication skills in oral or written interaction with a range of service users, carers and colleagues, either individually or in groups. |
| D7. | Make effective use of information and communication technology. |
| D8. | Prioritise their workload and manage their time effectively. |
| D9. | Continue to engage in self-directed learning that will promote professional development. |
| Learning & Teaching Processes | Assessment*** | |
| Clinical placements in the NHS (D1-D9) | Ongoing assessment by NHS clinical educators’ reports (D1-D9) | |
| Laboratory Practicals, and Clinical Tutorials (D1-D9) | IRCP & PPLA(D1, D2, D3, D4, D5, D6, D7, D8, D9) | |
| Online and other case studies (D1, D2, D3, D6, D8) | Practical Assignments (D1, D2, D3, D4, D5, D6, D7, D8, D9) | |
| Research proposal (D1, D2, D3, D4, D5, D6, D7, D8, D9) | Research portfolio (D1, D2, D3, D4, D5, D6, D7, D8, D9) | |
| PADP, PSDP, Clinical Portfolio (D1-D9) | Formative assessment (D1, D2, D3, D4, D5, D6, D7, D8, D9) |
***
IRCP = Individual Record of Clinical Practice (National Online Logbook used in Audiology)
PPLA = Personal Portfolio of Learning and Application (Electronic Portfolio of Evidence). This includes formal records/evidence of DOPS and CBDs.
DOPS = Direct Observation of Practical Skills
Mini-Cex = Mini Clinical Examination (often referred to as OSCEs – Objective Structured Clinical Examinations)
CBD = formal case-based discussion.
4. Structure of the programme
Year one course units
| Code | Course Unit title | Tutor | UK Credit Rating* | |
| Year 1 | HCDI 10000 | Professional Studies I | Bridget Goodier | 20 |
| HCDI 11601 | Psychology for Health and Lifespan Development | Rebecca Millman | 10 | |
| HCDI 10211 | Human Anatomy and Physiology for Healthcare Professionals I | Liz Sheader | 10 | |
|
HCDI 10212 |
Human Anatomy and Physiology for Healthcare Professionals II | Niall McLoughlin | 10 | |
| HCDI 10040 | Introduction to Healthcare Science | Debbie Cane | 10 | |
| HCDI 10050 | Applied Physics and Measurement | Richard Baker | 20 | |
| HCDI 10070 | Introduction to Neurosensory systems and their assessment and management | Tim Wilding | 20 | |
| HCDI 10080 | Clinical Placement and Practical Skills I | Bridget Goodier | 20 | |
| TOTAL CREDITS | 120 | |||
‘Generic Healthcare Science’ units
‘Neurosensory’ – theme specific units
Audiology specific units
*Some course units, especially those involving competency based assessments, may have both mark-based and pass/fail assessments. In such units an overall pass mark of 40% AND a pass in all the other components is necessary to be successfully awarded the credits for this unit. In such units an overall mark of 40% or more may be achieved, but the unit still failed if the pass/fail assessment components have not been successfully completed.
The course unit specifications will be available on Blackboard
Year two course units
| Code | Course Unit title | Tutor | UK Credit Rating* | |
| Year 2 | HCDI 20032 | Leadership in Healthcare | Kai Uus | 10 |
| HCDI 20002 | Research Methods & Statistics | Richard Baker | 10 | |
| HCDI 20001 | Audiological Science | Richard Baker | 20 | |
| HCDI 20020 | Adult Audiological Assessment and Management | Tim Wilding | 30 | |
| HCDI 21200 | Hearing Aids | Helen Glyde | 30 | |
| HCDI 21300 | Clinical Placement and Practical Skills II | Alison Edwards | 20 | |
| TOTAL CREDITS | 120 | |||
Leadership units
‘Generic Healthcare Science’ units
‘Neurosensory’ – theme specific units
Audiology specific units (may also contain ‘Neurosensory’ – theme specific content)
*Some course units, especially those involving competency based assessments, may have both mark-based and pass/fail assessments. In such units an overall pass mark of 40% AND a pass in all the other components is necessary to be successfully awarded the credits for this unit. In such units an overall mark of 40% or more may be achieved, but the unit still failed if the pass/fail assessment components have not been successfully completed.
The course unit specifications will be available on Blackboard
Year three course units
| Code | Course Unit title | Tutor | UK Credit Rating* | |
| Year 3 | HCDI 30090 | Professional Studies III | Siobhan Brennan | 10 |
| HCDI 32221 | Advanced Hearing Instruments and Contemporary Trends in Rehabilitation. | Alison Edwards & Helen Glyde | 10 | |
| HCDI 34441 | Tinnitus | Karolina Kluk-de Kort | 10 | |
| HCDI 35550 | Counselling & Communication Skills in Clinical Practice | Sheila Fidler | 20 | |
| HCDI 38880 | Audiology Research Project | Rebecca Millman | 30 | |
| *HCDI 39990 | Clinical Placement and Practical Skills III | Alison Edwards | 20 | |
| HCDI 36661 | Vestibular Pathology and Assessment | Debbie Cane | 10 | |
| HCDI 37770 | Paediatric Audiology | Kai Uus | 10 | |
| TOTAL CREDITS | 120 |
‘Generic Healthcare Science’ units
‘Neurosensory’ – theme specific units
Audiology specific units
*Some course units, especially those involving competency based assessments, may have both mark-based and pass/fail assessments. In such units an overall pass mark of 40% AND a pass in all the other components is necessary to be successfully awarded the credits for this unit. In such units an overall mark of 40% or more may be achieved, but the unit still failed if the pass/fail assessment components have not been successfully completed.
The course unit specifications will be available on Blackboard
5. Curriculum progression: intended learning outcomes for each year
| Year | Intended learning outcomes |
|
Year 1 (certificate of higher education) [FHEQ Level 4] |
The course units that you will study during the 1st year of your course will a generic study theme and a Neurosensory Sciences divisional theme. The former will cover topics such as study skills, what it means to be a Healthcare Science Practitioner, healthcare provision and disability, whole body anatomy and physiology, and introductions to psychology and development. The divisional theme covers more specific aspects of Neurosensory sciences relating to Audiology, Neurophysiology and Opthalmic/Vision Science. These topics include more detailed anatomy, physiology and pathophysiology of these neurosensory systems and how they are assessed, and also the basic mathematical and physical principles and measurement techniques relevant to these topics. |
|
Year 2 (diploma in higher education) [FHEQ Level 5] |
In your second year of study you will continue to develop generic skills relevant to professional practice as Healthcare Science practitioners and in particular those centred on patient centred approaches to healthcare. In addition you will also study aspects of research design and statistics to enable you to both critically evaluate research studies and to design and produce your own research portfolio in the third year. You will also study a range of physiological measurement techniques and instrumentation, which while centred on audiological assessment will be applicable to a wider range of neurosensory situations. Two-thirds of your 2nd year of study will specialise directly on audiology with emphasis on the adult auditory system, adult assessment management and rehabilitation including detailed study of modern hearing aids and how they are used. This year will also include an 18 week placement within an audiology clinic where you will develop you skills in adult auditory assessment and management. |
|
Year 3 [FHEQ Level 6] |
In your third year of study you will concentrate on more specialist aspect of audiology including areas such as tinnitus and a wider range of more specialist hearing instruments (and an optional unit on either Paediatric Audiology or Vestibular Assessment and Management). You will also use the research skills that you obtained in year 2 to put together a research portfolio on a topic of your own choosing. This year will also include a 22 week placement within an audiology clinic where you continue to develop your audiological skills with increased emphasis on coherent patient management strategies. |
6. Student induction, support and development (in order to deliver the year learning outcomes)
|
Academic support is provided by academic staff who provide tutorials to support their teaching in specific course units. In addition, each student is allocated an Academic Advisor who monitors learning and progress, initiating contact with students of all levels of achievement following exam board and agreeing with students personalised action plans for learning to help them attain their goals academically. A student’s Academic Advisor acts as personal tutor too, providing support and guidance regarding personal issues that might affect the student’s work. Examples of student support mechanisms in place include: Welcome Week
Academic Advisors
Student Support Staff
Academic Support (including support on clinic placements)
Other Support Mechanisms
|
7. Curriculum map of course units against intended learning outcomes of the programme
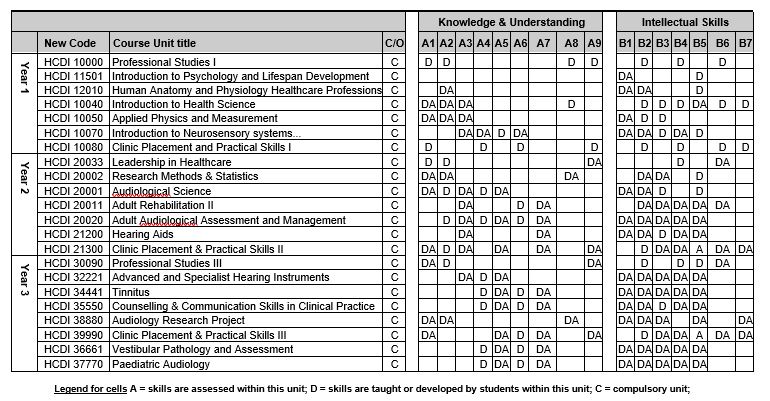
8. Criteria for admission
Qualifications
A-Level (inc. GCSE) Qualifications
| GCE A level | Grades ABB including one of the following: Biology, Chemistry, Physics, Maths, Psychology or Applied Science. |
| GCE AS level | Two AS levels at minimum of grade B accepted in place of one full A level. These AS subjects must be different from any A level awards. If the applicant does not have a full A level in a science subject then both AS levels must be chosen from Biology, Chemistry, Physics, Maths or Psychology. |
| GCE A level Double Award | Accepted in place of two full A Levels grades BB required. |
| GCSE | Minimum grade C in six subjects, including English Language. Grade B is required in Mathematics and a science (Biology, Chemistry, Physics or Science). Psychology is not accepted as the sole science subject at GCSE level. |
| Key Skills | The University warmly welcomes applications from students studying the Key Skills qualification. However, as the opportunities to take these modules are not open to all applicants, currently this is not an essential requirement of the University. |
| Subjects excluded | General Studies (not accepted as part of offer) |
Baccalaureate (inc. Irish Leaving Certificate) Qualifications
| International Baccalaureate | 33-34 points overall including 6, 5, 5 points at higher level. A science subject must be studied at higher level. |
| European Baccalaureate | Acceptable on its own or in combination with other qualifications. Applications from students studying for this qualification are welcome and all such applicants will be considered on an individual basis. Contact the University for further information. |
| Irish Leaving Certificate | ABBBB or AABBC including two of the following subjects; Biology, Chemistry, Physics, Maths, Psychology |
| Scottish Advanced Higher | Grades ABB including one of the following subjects: Biology, Chemistry, Physics, Mathematics and Psychology. |
| Scottish Higher | Grades AABBB including two of the following subjects: Biology, Chemistry, Physics, Mathematics and Psychology. |
| Subjects excluded | General Studies |
| English Language Requirement (e.g. IELTS, TOEFL) | Applicants for whom English is not a first language should appreciate that a particularly high standard of spoken and written English is necessary to cope with both academic and clinical work. Therefore as a minimum, the School requires IELTS 7.5 overall (with a minimum of 7.0 in each component). |
| BTEC | Extended Diploma: minimum of 70 credits awarded at Distinction, 100 at Merit and the remaining 10 credits at Pass or above |
| Access to HE (number & level of credits, subject area). |
Applications are considered on an individual basis, e.g. additional educational achievements, life experience and skills. Please contact the University for further information. Normal requirements for diploma applicants are 60 (10 hour) credits with 45 at Level 3 and the remainder at Level 2. We recommend that potential applicants choose either the Health or Science pathway with a minimum of 15 credits in a science subject. We require 15 credits at Distinction in science and 30 credits at Merit Applicants who do not have a Grade B at GCSE, or equivalent, in Mathematics should contact the University for further advice. |
| Other Qualifications Not Listed (e.g. Early Years BTEC qualifications.) | Applications from UK and EU students offering qualifications other than those listed above are welcomed. Please contact the University for further advice. For funding reasons we are unfortunately unable to accept applications from non-EU citizens. |
| Relevant Work Experience | It is not possible for all audiology service providers to offer work experience for applicants, therefore this is not a requirement. However some practical experience of working in Audiology related environments would be beneficial, e.g. the private sector, charitable organisations, lip-reading classes, Tinnitus support groups etc. |
Admissions Process: All applications are processed via UCAS.
9. Progression and assessment regulations
|
The Progression and Assessment regulations will follow the University regulations for Taught Degree Programmes that are applicable at Undergraduate Level except where professional body require specific aspects to differ. These exceptions are in-line with those that were applied to the BSc (Hons) Audiology Programme. These exceptions are detailed below. Assessment and Progression
Compensation Because of professional requirements stipulated by the Department of Health: “No condonement/compensation of modules and no aggregation of marks are permitted. Students must pass all modules to be eligible for the award of the MSC accredited degree. This approach is required irrespective of the HEI’s own academic regulations.” From: Delivering BSc [Hons] Degree Programmes in Healthcare Science for the new Modernising Scientific Careers Healthcare Science Practitioner Training Programme (PTP) – Guidelines for Higher Education Institutions and their NHS/Health Service Partners. January 2012 Reassessment
Carrying forward failed credit
Repeating the Year
Exit Awards
Degree Classification
|
10. Summary of Topics in all Years
Joint Teaching
You will no doubt discover that certain course units will be jointly taught to students studying on different programmes. Sometimes this is simply because a subject area that you need to study is already being taught elsewhere in the university and so it makes sense to double up. However, in particular subject areas, a deliberate decision has been made to teach you together with students on the BSc Speech and Language Therapy programme. It is intended that such inter-professional learning will benefit all students, as you learn to appreciate different perspectives and to understand the need for health, education and social care professionals to work in close collaboration. For the 1st year unit, HCDI10070 Introduction to Neurosensory Systems and their assessment and management, you will also share teaching with BSc Healthcare Science (Neurophysiology) students from Manchester Metropolitan University (MMU). In addition, for some course units at level 5 you will be taught jointly with Masters and Diploma students studying postgraduate Audiology. In this case, while the content of these units may be identical, course unit tutors will be very clear about the different levels expected of student work. Where units are joint taught, the distinction between BSc and MSc level is made in: (a) the intended learning outcomes for the course unit, (b) the pass-mark for the assessments (40% for BSc, 50% for MSc), (c) the level/depth of knowledge/understanding required to achieve this pass mark, and (d) the use of different assessments in order to achieve this differentiation.
Course Units, Practical Skills Classes and Clinics
Course Units will be running concurrently with your practical skills training and (to some extent) with your clinical placements; you will need to discuss your level of knowledge with your clinical tutor and placement supervisor and be prepared to undertake independent reading to support your clinical experience.
Professional and Clinical Components
This aspect runs throughout the three years and covers a wide diversity of subjects which are relevant to the practical work and professional role of the audiologist. Professional Studies in the first year aims to introduce you to a professional culture and ethos, and to provide you with the skills to enable studying and a lifelong approach to learning. In the second year you will take a unit called Leadership in Health that aims to help students to develop as leaders in their chosen professions. In addition to these you will cover basic and more advanced clinical skills and issues, from case history taking to the provision of services to non-English speaking clients; government and NHS policy; work in different areas of healthcare science and audiology and different health, social and educational teams; applications and interviews procedure. Interdisciplinary working and working in an educational context are important aspects throughout the degree but receive particular emphasis in Professional Studies. Sections of the topic are taught by the University tutors and visiting lecturers drawn from the fields of Audiology, Speech and Language Therapy and other related professions. Professional Studies is an essential supplement to clinical practice and is vital to ensure that students have an adequate understanding and knowledge of the overall role and responsibilities of healthcare workers.
Research
From year 1 you will be encouraged to take an informed and critical approach to reading about research, which will equip you for a professional commitment to evidence-based practice. We aim to give you adequate knowledge of research methods and statistics to enable you to evaluate published clinical research, to design a research project and to support you in undertaking and using clinical research in your future professional role.
Transferable Skills
Throughout the course, you will be provided with the opportunity to develop skills which will help you during your degree programme and also in future work environments and in lifelong learning. These skills are developed through familiarity with Information Systems (word-processing, computer statistical packages, spreadsheets, email, the internet, and computerised library resources), the use of the library, participation in Study Skills and Professional Skills Development Programmes and the opportunity for presentations in seminars (working individually and in groups). Professional preparation is a major component of this vocational course, addressed specifically through Professional Studies course units and clinical placements.
Year 1
During the first year, you will follow course units which aim to provide an understanding of human anatomy and physiology, development across the lifespan, and the basics of healthcare science including elements of physics and mathematics relevant to your studies. You will begin to address some of the assessment and equipment skills needed to be a healthcare scientist, and will be introduced to different ways of approaching disabilities, and specifically hearing loss. You will have clinical placements spread throughout the year with both observational and participatory involvement. Your understanding of research and evidence-based health care begins with an introduction to critical appraisal in your independent reading. The Professional Studies unit introduces you to the professional ethos and scope of the course. Much of the first year is taken side-by-side with students studying for the BSc Speech and Language Therapy, Nursing Programmes and BSc Healthcare Science (neurophysiology), the majority of whom will also progress to posts in the NHS.
Year 2
In the second year the course moves towards a more detailed study of the components of audiology. As well as continuing with developing your practical skills. You will take course units in a range of audiology specific topics that will give you the academic background and knowledge to prepare you for your placements. The 2nd year of study includes a large (18-week) component of practical and clinical skills education of which a large component is in clinical placements involving participation with adults with hearing loss. During this placement you will start to put your practical skills and academic knowledge into practice in the assessment and management of adult with hearing losses and start to develop your reflective logbook and start to gain the clinical competencies necessary to complete your Clinical Practice Logbook. Your understanding of normal and impaired auditory function will be extended through the course unit on hearing science, and your research understanding will be strengthened by the research methods course unit.
Year 3
During this year, you will continue to develop as healthcare science professionals, gaining more in-depth academic knowledge and understanding of a range of audiology topics (including optional Paediatric of Vestibular assessment and management) .You will be placed in two six-month clinical training posts in NHS audiology departments. The 3rd year of study includes a further large clinical placement block (22 weeks). You will spend time continuing to developing a reflective logbook record of your clinical practicum and you will complete elements of your Clinical Practice Logbook. During this third year you will also bring together the research skills you have learned throughout the programme to complete a substantial research project.
Handy-tip: As you progress through the programme you will revisit areas that you have studied in previous years. Your learning will become more in-depth and more applied – it is important that you keep all your notes from previous years and that you don’t ‘forget what you have learnt once you have passed a module. Subsequent exams and assignments will frequently assume knowledge and understanding from earlier course units.
SECTION 3 ASSESSMENT AND REGULATIONS
External examiners; general information on examinations; resit examinations; tips on answering examination questions; anonymous marking; submission of assignments; special circumstances; interruption of studies and withdrawal; degree regulations; assessment regulations; compensation arrangements; resit regulations; degree classification; assessment criteria; plagiarism; summary of assessments; Accreditation for Prior Learning (APL).
The results of all assessment on the degree programme are considered by the Board of Examiners which receives all marks, applies resit and compensation regulations and makes recommendations to School and Faculty regarding pass lists, resits, progression to the following year and degree classification. The Faculty ensures that appropriate procedures have been followed, that standards are comparable across degrees within the Faculty. Final year pass lists are shared with the appropriate professional bodies for this programme.
General Information on Examinations
Examinations take place at the end of Semester 1 (January examination period) and at the end of Semester 2 (May-June examination period) of each academic year. Information on the dates and times of the January and May/June examination periods is provided directly to students by the Central University Examinations Office. Individual timetables are sent to you via the Student Portal. You are responsible for checking the timetables and for alerting the programme team of any apparent problems. Examination results are published online via the student portal. Students who fail exams in January will also receive letters informing them of any resits. For the end of year exams, results are posted on the student portal and you will also receive the results by post. NO EXAMINATION RESULTS WILL BE GIVEN BY PHONE. After each examination period there will be an opportunity to discuss your results in with your Academic Advisor at the start of the following Semester.
Resit Examinations
If you fail to satisfy the examiners in any examination you may be allowed to take a resit examination. However, resit examinations are not a right, and are allowed at the discretion of the Board of Examiners. Resit examinations for Years 1 and 2 take place in the late August to early September exam period following the January and May/June examinations. You will receive information on these examinations in July and all students should arrange summer holidays/jobs to take the August/September resit examination dates into account. For centrally timetabled examinations there will be a resit fee which is paid at a flat rate regardless of how many resits you have. Failure to present for resit examinations may prevent you from continuing on the course.
The Summer Resit examination period is 23rd August to 3rd September 2021. It is your responsibility to make sure you are available should you be required to undertake a resit. Failure to do so may result in a mark of zero being awarded with subsequent implications regarding either continuation on the programme or eligibility for professional registration.
Handy-tip: Make sure you are available during resit exam periods – do not book holidays during this period on the assumption that you will pass everything.
Accreditation of Prior Learning
Accreditation of Prior Learning (APL) may be awarded to students whose previous academic or experiential learning is considered to be particularly relevant for a given course unit. APL may mean that a student is exempt course units and their assessment. The maximum allowance for APL in any one year is 30 credits. Further details can be found in the individual Course Unit Outlines in Appendices 1-3.
Formative assessment
This type of assessment is intended to help with your development or ‘formation’ as a student. You are often given qualitative feedback (comments) as well as quantitative feedback (numerical marks) for your work which tells you what you need to do to improve your marks for next time. Formative assessment usually takes the form of an assignment such as an essay, poster or presentation (rarely would a formative assessment be in written exam format) and you can normally expect the feedback from formative assessment in time to help you with summative assessment of the same or other related units.
Summative assessment
This type of assessment, sometimes referred to as ‘examined’ assessment, contributes to your end-of-year overall mark. Some of your year 2 marks and all the year 3 marks contribute to your degree classification (see later). Summative assessment may take various forms (e.g. essay, poster, presentation assignment or written exams). In the case of summative assignments, hand-in dates will usually be around the end of semester (although may vary depending on course unit). In the case of summative exams, these will normally take place in one of the two allocated exam periods towards the end of each semester.
External Examiners
In all University assessments, External Examiners play a vital role. They are responsible for maintaining academic standards and ensuring that candidates are marked fairly. The External Examiner is invited to comment on the appropriateness of assignment topics and examination questions and reads a selection of scripts from each examination and from assessed coursework.
For the session 2020/21 the External Examiners involved in moderating the BSc Healthcare Science (Audiology) course are:
Dr Jo White — QMU (Edinburgh University)
Dr Paul Radomskij- University College London
Dr Srikanth Chundu – Anglia Ruskin University
(1st year Anatomy and Physiology is externally examined by the external examiners for the courses which the unit is joint taught with)
External Examiners’ reports relating to this programme will be shared with student representatives at the Staff Student Liaison Committee (SSLC), where details of any actions carried out by the programme team in response to the External Examiners’ comments will be discussed. Students should contact their student representatives if they require any further information about External Examiners’ reports or the process for considering them. (Please note that these external examiners reports give details of the programme as a whole and do not relate to the work of individual students.)
Please note that it is inappropriate for students to make direct contact with External Examiners under any circumstances, in particular with regards to a student’s individual performance in assessments. Other appropriate mechanisms are available for students, including the University’s appeals or complaints procedures and the UMSU Advice Centre. In cases where a student does contact an External Examiner directly, External Examiners have been requested not to respond to direct queries. Instead, External Examiners should report the matter to their School contact who will then contact the student to remind them of the other methods available for students. If students have any queries concerning this, they should contact the Programme Director.
Some tips on answering examination questions
Here are some pointers to answering examination questions – they relate to any kind of question, seen or unseen:
1. Make sure you address the question(s) asked. This may seem obvious, but every year we get examples of students writing answers to questions that were not asked. It is of no use simply writing about what you know on a topic, if it does not address the question asked.
2. Make an initial plan of your answer. If you write with reference to your plan, it will give the answer added structure and coherence.
3. Make sure your answer contains all the appropriate facts with salient issues emphasised. If the salient issues are derived from published sources, then cite the sources in the text (i.e. author and year). Accurate citation helps to: (i) engender a sense of scholarship in your answer and (ii) maximise marks obtained. We do not expect an appended list of full references. Of course, citations must be accurate, and primary sources (e.g. journal articles) are better than multiple citing of a secondary source (e.g. a text book).
4. Unverified web resources (e.g. Wikipedia etc.) are not appropriate reference sources; they may however point you to other useful references (e.g. books, journal articles etc).
5. Make sure you spend an appropriate amount of time on each question. Don’t fall into the trap of spending extra time on one or two questions, to the detriment of others.
6. Make use of diagrams/graphs where appropriate – but make sure they are referenced from the text and are reasonably accurate/labelled.
7. Write legibly. We cannot give marks if we cannot read what has been written.
Handy-tip: Use the resources available to help prepare yourself for examinations and assessments, and if in doubt – ask.
Anonymous Marking
The University of Manchester implements a policy of anonymous marking, where appropriate, in order that marking of student work be carried out as objectively as possible. This means that prior knowledge of a student or expectations of their level of work will not influence marking. In all formal University examinations you conceal your identity by sticking down the fold-over corner of the answer book. Similarly for coursework students’ anonymity is maintained where possible and the majority of course work is submitted via Blackboard. Should course work be submitted in paper format then you should make use of the ‘coursework cover sheet’ available from the office, which has the same concealment procedure. In the case of both paper and electronically submitted coursework, please make sure you have not included your name on the assignment, but do add your student ID number on each page as a header or footer in case sheets become separated. First marking and internal moderation of marks as well as external moderation of marks are carried out anonymously and only when marking is complete are the top corners opened by an administrative secretary, to allow transfer of marks to the mark sheet and work to be handed back to students.
The Exam Boards also operate anonymously, with results being presented by student ID number. Where there is evidence of mitigating circumstances to consider, this will be presented by the Exams administrator who has access to the relevant information but without your name being revealed to the exam board. The Special Circumstances committee meets prior to the main exam board.
Written Assignments and Submission of Assignments
In order to be fair to all students, assignments should be submitted by the time and date arranged by the tutor concerned and organised by the examadministrator. Details of hand in dates will be displayed on the white board outside the undergraduate office and will be emailed to students.
You will be asked to submit assignments online via Blackboard and instructions will be provided by email. There is no need to submit a paper copy in this instance or complete a coversheet. You must include your student ID in the header (so it appears on every page) of your assignment and not your name, to ensure marking is anonymous. The submission title for all assignments should be your student ID. Failure to provide your student ID on your assignment will result in your assignment being marked per the marking guidelines, but your mark will not be released and you will need to make an appointment to see the Examinations Officer for your mark. The Turnitin software package is used to help markers detect plagiarism.
Handy-tip: When preparing and submitting assignments your student ID number must be on each page of the assignment and the submitted file name must be the student ID number.
You may also be asked to submit paper printed, or other format, hard copies of assignments. Hand in sessions are organised to fit around your timetable and usually take place in meeting room 1 or 2 in Ellen Wilkinson building. All hard copy work must be submitted during the allocated time slot and will not be accepted early. As mentioned above, assignments are submitted under an anonymous cover sheet which can be obtained from the undergraduate office.
For paper submissions it is ESSENTIAL that coversheets are completed in full for EVERY paper submission, ensuring that each receipted section details your student number and the ‘unit code’ of the course unit.
PLEASE DO NOT write your name on pieces of coursework. Submissions are assessed anonymously. To ensure you work is identifiable please remember to detail your student number and the unit code in a ‘header’ on each page of your assignment and fully complete a ‘Submission Coversheet.’
The below link contains more information on the submission of work for summative assignments:
http://www.tlso.manchester.ac.uk/map/teachinglearningassessment/assessment/sectionb-thepracticeofassessment/policyonsubmissionofworkforsummativeassessment/
Extension requests
Applications for extensions to any submission date must be made with supporting evidence and in good time. Extension request forms can be downloaded from Blackboard and should be submitted to the person who has set the assignment. Extensions will only be granted for good reason and should be agreed in writing prior to the submission deadline.
Handy-tip: Extension requests must be submitted with appropriate evidence and approved before the assignment deadline.
If an assignment is submitted after the original time and date arranged by the tutor or is submitted after the time and date re-negotiated with the tutor and agreed in writing following the consideration of submitted written evidence, a sliding scale of marking penalties will be applied as explained below.
Penalties for late submission
Penalties apply to work submitted late.
Any work that has been submitted after a deadline has passed is classed as late except in cases where an extension has already been agreed. There are no discretionary periods or periods of grace. A student who submits work at 1 second past a deadline or later will therefore be subject to a penalty for late submission.
Students who submit referral (resit) assignments after the deadline will automatically be subject to a mark of zero.
Handy-tip: The sliding scale mark penalties apply to first attempts only. Students who submit referral (resit) assignments after the deadline will be automatically subject to a mark of zero. There is no sliding scale in operation for resits/referrals.
Work that is submitted more than 9 calendar days late
Work submitted more than 9, but less than 10, calendar days late will be marked and feedback given but a penalty will be applied that results in the mark being reduced to zero.
Work submitted 10 or more calendar days late will be considered as non-submission (mark of zero automatically awarded). In such cases the normal rules for failing an assignment apply.
Penalties for work submitted up to 9 calendar days late:
No calculations are made for part-days. Any work submitted at any time within the first 24 hours following the published submission deadline will receive a penalty of 10% of the maximum amount of marks available. Any work submitted at any time between 24 hours and up to 48 hours late will receive a deduction of 20% of the marks available, and so on, at the rate of an additional 10% of available marks deducted per 24 hours, until the assignment is submitted or no marks remain.
For example, a piece of work which would have been awarded 65%, if submitted on time, would be reduced as follows:
| Number of Days Late | Mark Awarded |
| 1 | 55% |
| 2 | 45% |
| 3 | 35% |
| 4 | 25% |
| 5 | 15% |
| 6 | 5% |
| 7 | 0% |
The number of days late indicated in the table means all work submitted up to that number of days late. 1-day late work therefore refers to all work submitted within the first 24-hours after the deadline, 2-days is within 48-hours after and so on. This means that we are extremely strict concerning deadlines, 3pm on a certain date means exactly that. Submitting at 3.01pm on the deadline day (with 3pm deadline) constitutes a late submission and a reduction of 10% in the mark is indicated.
Students whose assignment mark falls below a pass as a result of a late penalty will not be asked to resubmit the assignment; instead, the original assignment will be used in lieu of a referral, and all normal resit/referral procedures will apply.
Handy-tip: Plan your work so that you submit all assignments in plenty of time – one second late will incur a penalty. If you submit the day before you can still resubmit an amended version before the deadline. There is no sliding scale for resit/referral submissions. Submitting a resit assignment one second late could result in failure of the course unit and exclusion from the programme unless another resit opportunity is permitted (no more than one resit attempt per assessment is allowed in year 2/3).
Referencing
The use of correct referencing is important for all submitted work and marks may be deducted for poor referencing style. Guidance on how to correctly reference is given during course induction and within the professional studies module. A reference list is not a bibliography. Remember that in scientific writing referencing is highly important as it enables the reader to know the source of the knowledge and thus confirm its scientific validity.
You must use APA referencing style for all submitted assessments unless otherwise stated. APA is a variant of Harvard author-date style referencing.
It is also important to note that websites and lecture notes are, in almost all cases, inappropriate references. You must search for, and cite, the source of knowledge which can usually be found in peer reviewed scientific journal articles. Remember that citing a text book can be appropriate in some cases, but in most cases it is better to find, read, and cite the primary source of the knowledge and not the secondary source (the book) where you might have first read it.
Exceeding the word limit
Word limits for assignments are set for a good reason. You must clearly and honestly state the word count for your work at the end of all assignments you submit. You should state the word count just before the reference list that appears at the end of the work. You should also state the word count at end of all assignment subsections that have a word limit set. The word count must include the entirety of the main body of text (or each subsection with a limit) including any in text citations. The reference list at the end is the only part of an assignment that is never included in the word count. Having a word limit for an assignment is akin to everyone having the same length of time to sit a written exam (in special circumstanced for specific disabilities extra time might be allowed). You will be penalised by a reduction in your mark if your assignment exceeds the word limit according to the following sliding scale:
| Number of words above the stated limit | Percentage points deducted |
| > 0% ≤ 5% | 5 |
| > 5% ≤ 10% | 10 |
| > 10% ≤ 15% | 15 |
| Continued in increasing steps of 5% | Continued increasing in steps of 5 |
| ≥ 40% | A mark of zero is awarded |
It is important to note that any deliberate attempt to conceal the fact that your work is over word limit by understating the word count within the work is an offense of academic and professional malpractice which may result punitive action.
A reduction of 5 percentage points will be applied if the word limit is exceeded by just 1 word. It is therefore imperative that you are able to properly and correctly obtain the word count for each assignment you submit. Further guidance on exactly how to obtain the correct word count using Microsoft Word is available in the blackboard programme space. The above word limit regulations apply to all assignments unless otherwise stated by the module tutor setting the work.
Handy-tip: Word limits are set for a reason – make sure you know what the exact word limit is for your assignment and don’t exceed it. If you are unsure how we count the words look at the online tutorial on Blackboard.
Format (font size/style)
Your work should be submitted using the following formatting unless stated otherwise:
- Double line spacing
- 12 point Arial Font
- Harvard Referencing, Harvard style in text citations
- Reference list at end of work, Harvard style reference list
- Word count included at the end of the main body of text before the reference list
Further guidance on exactly how to apply the correct formatting using Microsoft Word is available in the blackboard programme space. The above regulations apply to all assignments unless otherwise stated by the module tutor setting the work.
Plagiarism
Plagiarism is presenting the ideas, work or words of other people without proper, clear and unambiguous acknowledgement. It is a serious and growing problem in higher education, especially with regard to the authenticity of assessed coursework. Software is now available to detect plagiarism and is used widely. If your work is discovered to contain serious elements of plagiarism, it may have serious consequences for your future study. In order to avoid plagiarism in your own writings, refer to appendices of this handbook. The issue of plagiarism will also be fully explored in the year 1 Professional Studies Unit.
Handy-tip: Make sure you are well aware of what plagiarism is before you start writing assignments and if you have any doubt ask your academic advisor for guidance.
Exam Resources
For further resources to help you prepare for exams and other assessments see:
http://www.exams.manchester.ac.uk/
Mitigating Circumstances
Evidence for personal and medical mitigating circumstances is considered by a Special Circumstances Committee immediately prior to each Exam Board. The Committee will look at evidence for the semester, including both teaching and examination periods. It will not be able to consider any circumstances without a written submission from you accompanied by the appropriate form obtainable from Blackboard. The committee will consider all written submissions and will make recommendations on them where there is evidence that they have been serious enough to have an effect on one or more elements of assessment. In considering each case, the committee refers to guidelines which are widely used across the university.
If examinations or assessments are missed due to illness or particularly difficult circumstances you MUST PROVIDE SUPPORTING EVIDENCE. The certificate should specifically cover the date(s) of the examination(s) or assessment(s) concerned. It is your responsibility to ensure a ‘Mitigating Circumstances Form’ is submitted to the Undergraduate Office to accompany any supporting evidence (e.g. Medical Certificate). Deadlines for the forms to be submitted are set before each assessment (exam) period. To be accepted circumstances impacting assessment must normally be declared prior to, and not after, the published deadlines for each assessment period. If a circumstance arises (begins) during an assessment period then it must be declared within one working day of the end of that assessment period. Retrospective circumstances (those made after the assessment period, or published deadlines) cannot normally be accepted without a credible and compelling reason why they were not submitted at the right time when they occurred.
The Special Circumstances Committee recommends to the Board of Examiners if a first sit opportunity should be granted. Please note that first sits are granted at the discretion of the Board of Examiners and are only applied if you fail an assessment – you cannot retake assessments you have passed. Please see your Academic Advisor for further advice and information about mitigating circumstances.
Guidance on mitigating circumstances can be found at
http://documents.manchester.ac.uk/DocuInfo.aspx?DocID=23886
Guidance relating to missing examinations can be found at:
http://www.studentnet.manchester.ac.uk/crucial-guide/academic-life/exams/missing-examinations/
The policy can be found at:
Handy-tip: If you think your performance in any assessment is likely to be affected by medical or personal circumstances that were not known to you at the start of your studies then consider submitting a mitigating circumstances form before the appropriate deadline – if in doubt talk to your Academic Advisor.
Mitigating circumstances versus Extension Requests
It is important that students understand the difference between these two procedures (and the associated forms).
- Extension Requests – The extension request procedure is designed to allow (in exceptional circumstances) students to be granted extra time to complete course work should significant medical or personal circumstances occur that would prevent a student from submitting and assignment by the specified deadline. If an extension is granted then the issue is considered as having been addressed appropriately and no further mitigation relating to the particular circumstances will be considered.
- Mitigating Circumstances – Should unforeseen changes medical or personal circumstances occur that lead to a significant impact on the quality of a students’ work, or their ability to sit an exam then the mitigating circumstances process is designed to take this into account and such mitigation is considered, along with supporting evidence, prior to the examination board.
Please note that it is rarely appropriate to submit both mitigating circumstances and an extension request that relate to the same issue as granting an extension is usually considered as sufficient to address the issue. If you are in any doubt then please discuss with your academic advisor.
Handy-tip: Extension requests are for situations where, for some medical or personal circumstances you can’t meet a set deadline. Mitigating circumstances are for situations where the assessment will be completed but there are circumstances that mean that your performance may be below your best. It is rarely appropriate to submit both as any extension is put in place to enable you to fulfil the assessment requirements to the best of your ability.
Interruption and currency of award
The programme is full time and the length of the programme is three years. Very occasionally it may be deemed necessary (on very serious personal or health grounds) to for a student to interrupt their studies for up to a year (any single interruption is normally for a maximum of one year). Any such interruption (and return from interruption), must have the full support of Health Education Northwest as the placement provider. It is important to recognise that this is a professional healthcare training programme and as such knowledge and practice needs to be considered current we need to ensure that you are able to meet the full set of programme learning outcomes (and thus demonstrate eligibility to register with the RCCP, AHCS or HCPC upon graduation).. To this end, it may be necessary for students returning from interruptions to undertake additional work in order to regain or update their knowledge and skills and to re-enter the programme of study at the most appropriate point. In cases of prolonged absence this may require retaking a full year of study which may result in associated tuition fees being payable.
If you are considering interrupting your studies (i.e. taking a year out from the course for medical/personal reasons) or withdrawing from the programme, you are advised to discuss the situation with your Academic Advisor, School Student Support Administrator or the Programme Director. Interruption must be agreed by the Board of Examiners. The Board of Examiners may also require you to interrupt your studies in order to complete academic/clinical requirements before progressing into the following year of the programme. If you do decide to withdraw from the course, then formal notice should be given in writing to the Programme Director. Please note that interruption of studies will only be allowed subject to significant medical or personal circumstances.
Guidance on interruptions can be found at:
www.tlso.manchester.ac.uk/map/teachinglearningassessment/learning/interruptionstotaughtprogrammes/
Credit and Undergraduate Awards Regulations
The full University of Manchester regulations for undergraduate degrees can be found at the link given below, but some important features specific to the BSc (Hons) Healthcare Science (Audiology) are given below.
University of Manchester regulations for undergraduate degrees:
http://documents.manchester.ac.uk/DocuInfo.aspx?DocID=13147
Eligibility for professional registration will be contingent upon award of an Honours Degree in Healthcare Science (Audiology) which must include the credits accrued from ALL course units specified in appendices 1-3.
Handy-tip: Understand that ALL course units need to be passed to allow professional registration.
Assessment Regulations
- The degree is offered under the aegis of the School of Health and the Faculty of Biology and Medicine and Health.
- The marking scheme is numerical, using the range 0 – 100%; the pass mark is set at 40% (see marking criteria). It should be noted, however that some assessments may require a higher pass mark or be marked as pass/fail, especially when the assessment relates to areas of professional competence.
- The marks for each subject are determined by the examiners, including the external examiner in that subject.
- In a case where a candidate’s marks fall just below a borderline, the Examinations Board may, at their discretion, take into account relevant attendance records, notified medical or personal circumstances and course work (other than examined course work) to inform their decisions.
Handy-tip: Make sure you familiarise yourself with the assessments taking place for each course unit and how they fit into the overall progression regulations of the degree.
Compensation Arrangements
Because of professional requirements stipulated by the National School of Healthcare Science:
“No condonment/compensation of modules and no aggregation of marks are permitted. Students must pass all modules to be eligible for the award of the MSC accredited degree. This approach is required irrespective of the HEI’s own academic regulations.”
From: Delivering BSc [Hons] Degree Programmes in Healthcare Science for the new Modernising Scientific Careers Healthcare Science Practitioner Training Programme (PTP) – Guidelines for Higher Education Institutions and their NHS/Health Service Partners. January 2012
Handy-tip: No compensation is allowed between course units in this programme. This means that every course unit must be passed in order to progress and graduate.
Assessment and Resit Regulations
The University’s progression principles are based on the principle that 120 academic credits must be passed before progression to subsequent academic years. For this programme, because of Professional Body requirements compensation of failed course units is not allowed[2]. Any student not obtaining pass marks for the full 120 academic credits (after all appropriate reassessment opportunities) will be deemed to have failed that year of study and be exited from the programme. Specific assessment regulations for this programme are presented below.
- The pass-mark for academic units, where a mark is allocated is 40%. Some units may be classed as pass/fail in which case a ‘pass’ mark must be achieved. Each unit must be passed in order for credits to be awarded for that unit.
- Certain course units may have multiple assessment components; the overall unit mark is normally calculated as a weighted average of the different assessments. Where assessment components within a unit are pass/fail, each of these components must be passed.
- Assessments normally take place in the January and May/June examination periods, but assessments may be arranged outside of these periods.
- Following each assessment period an Examination Board is held that reviews assessment marks and makes decisions regarding progression to subsequent year, resits opportunities, exclusion from the programme and award of degree classifications.
- A student must pass a minimum of 40 credits at first attempt at each level in order to eligible for progression to subsequent year (after appropriate reassessment if necessary). If a student fails to pass this minimum number of credits then they will be excluded on grounds of academic failure (i.e. if they fail more than 80 credits at first attempt.
- Students that have passed 40 credits or more, but have not passed the required 120 credits may, at the discretion of the examination board, be allowed opportunities to be reassessed on the failed units (these reassessments are commonly referred to as resits, or referred assessments, also see 11-13 below). In making a decision to allow resits an examination board take into consideration the overall profile of marks (e.g. whether marks are generally in the 30-40 range compared to those being below 20-30%) and/or student attendance and engagement in the programme.
- Resits normally take place in the August/September of the year in which the examinations were first taken – students are advised that it is their responsibility to make sure that they are available for the whole of this resit period should reassessment be required.
- The general principle is that only one attempt at reassessment of failed course units will normally be allowed.
- Unit marks for resit assessments are capped to ensure that student do not gain an advantage by being allowed to resit assessments. If a unit is passed at resit, but the original mark was 29% or below, the unit mark will be capped at 30%. If the original unit mark was between 30 and 39% and is passed at resit then the original mark will be awarded for that unit.
- In calculating year average and degree classifications the original marks (and/or capped marks as per 9 above) will be used to calculate weighted averages according to the number of credits assigned to each course unit.
- In the first year of study (level 4) a student failing resit assessments may be allowed to carry up to 20 credits into the subsequent year of study for a 2nd resit attempt. Students failing more than 20 credits at resit assessment would normally exit the programme on the grounds of academic failure.
- In the second year, (level 5) students may be permitted to resit course units, up to a maximum of 80 credits, with one resit opportunity for each failed assessment task (at the discretion of the Examinations Board). One resit attempt of all OSCE stations may be permitted (at the discretion of exam board). A second resit attempt of up to two OSCE stations may be permitted (again at the discretion of exam board), failure of more than two OSCE stations at the first resit attempt would normally result in failure of the academic year. All resits must be passed in the August/September resit period to allow progression to the third year of study, resits of 2nd year units cannot be carried into the 3rd year of study. Students failing any of these resits will normally not be allowed to continue on the programme.
- In the third year (level 6), at the discretion of the Examination Board, a student may be permitted to resit course units, up to a maximum of 40 credits, with one resit opportunity for each assessment task, in order to allow the award of a degree in BSc (Hons) Healthcare Science (Audiology). Please note that clinical placement based assessment tasks that require further placement time cannot be resat after the end of the allocated placement time; this is because, unless special circumstances apply, no additional placement time is permitted.
- If a student fails level 6 units (after due consideration to point 13) and a minimum of 300 academic credits have been accrued, the award of BSc (Ord) in Healthcare Science may be considered by the Board of Examiners – such an award will not lead to eligibility for registration as a Healthcare Science Practitioner.
- For some course units, an alternative resit format may be given. In this case, rather than taking standard unseen resit examinations, for example, students may be asked to submit answers to all questions on the failed examination paper as an assignment.
- In any of the above regulations the Examinations Board take into consideration any appropriately evidenced mitigating circumstances provided by the student according to the University Guidance on Mitigating Circumstances.
Handy-tip: After the first year of study only one resit attempt at each assessment is allowed (unless there are appropriate mitigating circumstances). Any resit opportunities are allowed at the discretion of the examination board, and failure of any course unit at resit may lead to exclusion from the programme – please make sure you understand the resit regulations and the implications of any assessment failure – if in doubt talk to your Academic Advisor.
Degree classification
- All marks will be weighted in proportion to the credit rating of the course units taken. A Year 2 and Year 3 average mark will be calculated from the weighted course unit marks within each year respectively.
- For the award of BSc (Hons) in Healthcare Science (Audiology), 360 credits (including a minimum of 120 at level 6) must be accumulated by the end of year 3.
- The final mark for degree classification consideration will be a year 2 and year 3 weighted mark (also see 1 above). The weighting applied will be 0.33/0.67 (33% of the mark from year 2 and 67% from year 3). All course unit marks from year 2 and year 3 form part of the degree classification mark.
Handy-tip: A 20 credit unit in year 2 counts for approximately 17% of the year 2 mark (20 of 120 units that have a mark); this counts for approximately 6% of the overall degree classification mark (0.33/0.67 year 2/3 ratio). A 20 credit unit in year 3 counts for approximately 17% of the year 3 mark (20 of the 120 units that have a mark). This counts for approximately 12% of the overall degree classification mark.
Rules for all students
- The Board of Examiners will adopt the following procedures in relation to final degree classification:
Class I an average of 70% or more
Class II(i) an average of 60% or more
Class II(ii) an average of 50% or more
Class III an average of 40% or more
- In borderline cases (i.e. where the average mark falls in the ranges 68%‑69%; 58%‑59%; 48%‑49%; 38%‑39%), a student may be considered for the next higher class of degree by the following method:
A student who obtains an overall mark in the boundary zone for that class and obtains at least two-thirds of the credits for the final year with a mark not less than 40.0% will obtain that class if at least two thirds of the credits for the final year (80 credits) are in or above the range required for that class.
Please note that the final degree classification mark is calculated to one decimal place. A student with degree classification mark of 69.9% will be awarded a Class II(i) degree unless their marks meet the boundary condition to allow award of a Class I degree (80 credits in the final year with a mark higher than 70%).
The Board of Examiners will also consider any mitigating circumstances brought to their attention that may have affected the performance of the student. It is therefore essential that students bring any such matters to the notice of examiners by the appropriate deadline. You will be notified of these deadlines prior to each examination period.
Course Unit Assessments
Throughout the BSc Healthcare Science (Audiology) programme a range of assessments are used that include verbal presentations, literature reviews, and formal unseen written examinations consisting of online MCQ assessments (including other similar question types such as ‘extended matching questions’ etc), computational questions, short answer questions and essays. The assessment methods employed by each unit will vary and be tailored to match the material delivered and stated ILOs for each unit. The assessments will test students’ abilities to gather information from a wide range of sources, evaluate and critically analyse information, make considered judgments about that information and synthesize material into logical and coherent pieces of work.
Details of the specific assessment types for each course unit can be found in section 2 of this handbook and in appendices 1-3 and indicative assessment marking criteria can be found in the previous few pages of this handbook. For further details of specific unit assessments please also see the Clinical Handbook, Research Project Handbook and other unit specific information that may be provided by unit tutors.
Marking Criteria
For each assessment a marking criteria is applied to help ensure consistency of marking. Appendix 16 gives a detailed breakdown of the generic marking criteria that covers the majority of examination and written assignment based assessments. This marking criteria is provided to help you understand the differences across your three years of study, and also to help you understand how assessments are differentiated across the full range of marks.
Whilst the marking criteria in Appendix 9 are quite comprehensive, some assessments will have their own criteria and you will be made aware of these in the appropriate units. This is especially relevant in clinical and professional competency type assessments that may be pass/fail rather than graded 0-100.
Handy-tip: The marking criteria and any guidance given by lecturers or course unit leads are designed to help you – please make use of this information to guide your assessment preparation.
Assessment Feedback
After each assessment you should be given feedback on your performance, both in terms of what you did wrong, but also how you can improve. For written assignments this will be in the form of comments and feedback on Blackboard. For unseen exams individual feedback sheets are made available to students. You can also approach the course unit lead if you require further feedback.
It is vitally important that you read and understand any feedback given as this will help you spot any weakness in your performance or assessment preparation – for example you may have written an assignment where the feedback comments about poor structure – if this is the case go back and re-read the assignment and the feedback together and try to identify how you could improve.
Handy-tip: Make sure you read the feedback on each assessment carefully – it is designed to help you improve. This is especially important if you have to resit the assessment.
General Feedback on your Performance
As well as formal feedback on summative assessment there is a huge range of different ways you are given feedback. Below are just a few of them:
- Questions asked in lectures or other teaching sessions – if you don’t know the answer, be honest and say so, but then ask yourself why you don’t know. If the question is about something from a previous year, make a note and go back to that material and revise it. If a lecturer says ‘you should know this’ or something similar – that is because that is the case, they are not trying to embarrass you.
- Guidance given in practical and other teaching session – if you are carrying practical tasks or group work and a staff member prompts you or corrects errors – that is a form of feedback. Make use of that and make a written or mental note not of what you were doing wrong and how to address it.
- Discussion of formative exam questions – most lecturers will give example exam questions, formative quizzes or online quizzes – use these to monito your performance and use any subsequent discussions to highlight your own areas for improvement.
- Academic Advisor meetings – academic advisors are there to help you they will give you feedback on your overall performance – engage in discussion with them about how you can improve.
- Meetings with Lecturers – If you are struggling with any aspect of a course unit – chances are you won’t be alone. If this is the case then arrange an appointment with the lecturer to go over the material – of if several of you are struggling then please ask the lecturer to go over it the following week.
- Other feedback mechanisms – most feedback given to students isn’t labelled as such – any time you are given information that is provided to help you improve – that is feedback, please make use of it.
Handy-tip: Make sure that you make use of any feedback given – make notes and learn from your mistakes.
Group work and Group Assignments
Working together is a crucial part of professional life as a Healthcare Scientist and as such you have a range of group work activities and some group assignments. In such situations planning and working together is crucial – make sure you plan in advance the range of meetings you need. You will need to be prepared to spend time on campus outside lectures so that you can meet with other students. A mature and planned approach to such work will help improve any work produced.
SECTION 4 STUDENT SUPPORT, GUIDANCE AN REPRESENTATION
Tutorial policy; subject tutorials; project tutorials; PADPs: programme evaluation; student representation; programme committees, complaints and appeals.
Programme Committee & Student Progress Committee
The Programme Committee (PC) and its sub-committee, the Student Progress Committee (SPC), are responsible for monitoring the work and attendance records for each student, for progression and development of the course and for the co-ordination of course administration.
Programme development is also overseen by the National School of Healthcare Science who prescribe the curriculum and accredit the programme (as do the RCCP and HCPC). The programme is subject to accreditation by the NSHCS every 4 years (reaccreditation was granted Summer 2016). In addition, all academic programmes are subject to annual reviews internal to the University, and to Periodic (6-yearly) internal reviews (which involve input from an external subject specialist plus academics from other Faculties.
Personal, Academic and Clinical tutorials
- At the start of the course, you will be assigned an Academic Advisor who will normally remain the same person throughout the three years of the course. You may ask to change your Academic Advisor at any time if there is good reason. You should raise this request with the Programme Director and you would then be assigned to another advisor at the discretion of the Student Progress Committee (i.e. it is not possible for you to specify the alternative advisor). The role of the Academic Advisors is to give general guidance on academic and non-academic problems and s/he is often the person to ask for a reference when required.
- It is expected that advisees meet their advisor at least once per semester. In year 1 your Academic Advisor will arrange a meeting with you during the beginning of first semester. This will normally be a group meeting with all their advisees from your year group. They will inform you of the best way to contact them to arrange subsequent meetings.
- In each year you will be required to attend clinical tutorials. These are designed to prepare you for your clinical placements as well as provide an opportunity for you to reflect on your experiences post placement. It is the responsibility of the University Clinical Tutors to receive and to read reports from Placement Supervisors when they arrive. If you have a query about any of these reports you should therefore see your clinical tutor.
Handy-tip: Make sure you make the best use of your Academic Advisor and Clinical Tutors – they are there to help you. If they ask for your to meet with them please make sure you attend the appointments.
Subject tutorials
Subject tutors responsible for delivering the course units may arrange timetabled academic tutorials for you to pursue in more depth aspects of subject specific knowledge. You may be expected to prepare a piece of work for these tutorials, or to present a précis of a key paper. The content and timing of tutorials will be specified by the tutor at the beginning of the semester.
Academic Feedback
Feedback on academic progress is given by various means, the most obvious of which is the summative feedback provided by assignment/exam marks. When written assignments are given back they will be accompanied by feedback sheets which give a breakdown of the key issues concerning the marking of the assignment. If the assignment was submitted on Blackboard, feedback will usually be given online. You will also receive an individual feedback form for all examinations. Individual or group feedback may also be given by Course Unit Tutors or by Academic Advisors – this may take the form of verbal, as well as written, feedback. Students can request such feedback from Unit Tutors or Academic Advisors (see also previous section).
Project tutorials
In third year you will be assigned a project supervisor. It is our aim to ensure that you are properly supported during your studies and that both you and your supervisors are aware of the amount of supervision which is appropriate. The following guidelines for project tutorials have therefore been drawn up and apply to students and supervisors (see project handbook for further details):
- You are entitled to a maximum of 5 hours contact time with the tutor during year 3.
- It is your responsibility to ask for and arrange project tutorials at appropriate times with the tutor, to prepare appropriately for tutorials and to submit work at the agreed times.
- The tutor will keep a record of the time spent in tutorials and a record of the discussion which occurred during the supervision.
- It is the responsibility of the tutor to ensure that s/he is reasonably available for you or let you know when s/he will be available.
- It is the responsibility of the tutor to read and give back work submitted for comments within three weeks: tutors are expected to read through all project sections in first draft, provided that the student meets the agreed submission deadlines.
- Any work handed in after the final specified deadline will not be read.
Handy-tip: The 3rd year project is a 30 credit unit and the emphasis is very much on the students own work – begin planning your work early (start of year 3) but it would help you immensely if you started thinking about it towards the end of year 2.
Other tutorials
You can reasonably expect to be able to see a lecturer individually for discussion of, say, a specific academic or clinical enquiry or a personal problem. Staff workloads, however, limit the availability of tutors. Most staff operate an open door policy where you can knock on their door any time during the week and either see them then, or arrange an appointment. Some staff may however operate an office hours system and post their ‘office hours’ on their door or. These are the times each week when they are available for drop-in enquiries. You can of course arrange to see staff outside these times but we ask that you make an appointment by phone or email to be sure of finding a time convenient for everyone.
Staff are always willing to see students with personal emergencies, such as ill-health, but they may not always be in their rooms. In that case you should leave a telephone number where you can be contacted with the Undergraduate Office or with the staff via e-mail.
The University Of Manchester Library
The University of Manchester Library http://www.library.manchester.ac.uk/ provides you with the resources and support you need throughout your Healthcare Science (Audiology) degree programme. The Main Library houses all of the essential text books whilst the Alan Gilbert Learning Commons provides a 24/7 learning environment in addition to study skills workshops. The Library also has an extensive collection of eBooks, databases and journals available online.
The My Library tab in My Manchester (http://my.manchester.ac.uk) has quick links to all of the Library’s resources and services available to students.
Getting Started
You will need your student card to access all library sites around campus. Many of our services and resources also require you to confirm that you are a registered student. This authentication can be your student card, the ID number on the card, your Library PIN, the central username and password you use to log on, or a combination of these.
There is a library guide for Speech and Language Therapy and Healthcare Science (Audiology) students giving all of the latest information on resources and learning and research services available. This is a good starting point if you are looking for any library resources or information related to your course.
Each course module in Blackboard includes an online reading list, so you can quickly check availability and directly access e-books, digitised chapters and e-journals or articles.
The Main Library
The Main Library holds the principal collection of books and journals for Audiology. Textbooks are located on Floor 2 of the Blue Area, together with books in other related subjects. Audiology journals held in print are on Floor 1 of the Green Area in the Clinical Sciences sequence; further relevant periodicals are shelved in other areas of the Main Library. The library search facility will let you know what items are available and where to find them, including eBooks and online journals.
The Main Library offers group study rooms, individual study space options and computer clusters. Wi-Fi is available throughout the building and a cafe lounge can be found on the ground floor. The Library has long opening hours and extends these during exam periods. Please check Locations and Opening Hours for full details on opening hours and facilities.
http://www.library.manchester.ac.uk/locations-and-opening-hours/
My Learning Essentials
http://www.library.manchester.ac.uk/academicsupport/mylearningessentials/This is an online set of Study-Skills resources aimed at helping students adapt to studying at University. A range of resources and exercises are available in areas such as: writing skills, organising your work; communicating; finding information; evaluating your sources and preparing for your career.
The Alan Gilbert Learning Commons
The Alan Gilbert Learning Commons is a state-of-the-art learning environment with 24/7 opening hours throughout term-time. The Learning Commons has flexible open learning spaces with multimedia facilities, computer clusters and 30 bookable group study rooms with whiteboards and media screens.
http://www.library.manchester.ac.uk/locations-and-opening-hours/learning-commons/
There is a series of training workshops covering a variety of academic and transferable skills hosted in the training room at the Learning Commons. These workshops include training on revision/study skills, note-taking and other topics and have been developed by Learning Commons staff in partnership with other teams across the University. Full details of training sessions are available in the My Learning Essentials Calendar.
Handy-tip: The library and learning commons have a huge range of physical and online resources – have a look at those listed above and make sure your bookmark them on your computer – especially the ‘MyLearningEssentials’
Student Support Administrator
The Student Support Administrator (Ryan Hurst) provides advice and guidance to students and staff in the school. He offers assistance which complements and underpins the support provided by academic departments and can work with you to explore what options are available to you within the School and the wider University.
Ryan can talk through with you issues such as interrupting your studies and progression, the submission of details of mitigating circumstances, work and attendance problems and any personal concerns that are affecting your ability to study and engage fully with your course. It is important to point out that Student Support is not a counselling service; it is a practical problem solving service.
Ryan is based in the Undergraduate Office in the Zochonis Building or, alternatively you can call Ryan on 0161 275 7332 or email
Other services to contact for support include:Student Support and Advice
The Student Support and Advice is a student-centred service open to all Undergraduates and Postgraduates, from all departments across the whole University. The service provides confidential advice on any academic matter, from information regarding course transfers, for example, to referrals for study skills courses, or guidance in appeals procedures or advice on complex issues where a student’s work is being affected in any way.
Support and Advice website: http://www.studentsupport.manchester.ac.uk/
Counselling Service
The counselling service is available for all students. It is free and consists of a team of professional counsellors. The service provides confidential counselling for anyone who wants help with personal problems affecting their work or well-being.
The service is open 9.00am to 4.00pm Monday to Friday all year round except public holidays.
Disability Advisory and Support Service
The University has a Disability Advisory and Support Service (DASS), whose aim is to assist students, both prospective and current, to identify their needs whilst studying at the University. They then enable students to actually access the practical support.
In addition, the School has a Disability Support Officer, Ryan Hurst, who co-ordinates support arrangements for all students. Ryan is available to discuss support needs with individual students His contact details are 0161 275 7332; email: ryan.hurst-2@manchester.ac.uk
Handy-tip: If you are registered with DASS please make sure that you engage with them and attend appropriate appointments.
If you have disclosed a disability or long term health condition in your original UCAS application, you will have been contacted DASS and asked to attend for a full assessment of your study support needs. However, if you would like to disclose a disability at a later stage in your degree programme, you can do so by talking to any member of the teaching staff (usually your personal tutor or the Programme Director, School Student Support Administrator) or by going directly to DASS. The earlier in the academic year you can do this, the better, so that any necessary support can be put in place as early as possible. You may, for example, need special conditions and/or extra time in exams or special consideration may be given in marking of your written assignments.
DASS and Adjustments – once you have been assessed by DASS they will recommend to the school what are called ‘reasonable adjustments’. Depending on your disability such adjustments may include: extra time in exams, provision of a note-taker; automatic extensions for assignment deadlines. Please note that it is important that you are aware of such adjustments and that you discuss these with your academic advisor as some may have unforeseen circumstances. For example automatic one-week extensions to all assignments may mean that you end up simply delaying all your work rather than using the extension as and when it is needed.
Occupational Health
Occupational Health is a specialised area of medicine concerned with the way in which an individual’s health can affect his or her ability to do a job and to study and conversely how the work environment can affect an individual’s health. Their aim is to promote the physical, mental and social well-being of students and to reduce the incidence of ill-health arising from exposure to work place hazards.
In order to proceed onto placements all students must complete the appropriate health checks and inoculations – this process occurs over a period of time during the first year and you must attend the appointments when they are scheduled – failure to do so may result in you being unable to complete your clinical placements.
Handy-tip: It is important that you attend ALL occupational health appointments as and when they are scheduled – this is a requirements of the course in order to ensure that you are able to attend clinical placements.
Students’ Union Advice Centre
The Students Union has advisers who can help with any matter ranging from finances to housing and beyond. On the South Campus, the Advice Centre is on the first floor in the Student Union Building, and is open Monday to Friday, 10.00am to 4.00pm, term time and vacation (closed on the last Wednesday of each month). There is no need to make an appointment
Student Union advice service website: https://manchesterstudentsunion.com/adviceservice
Call us them on: 0161 275 2952
Email them at: advice.su@manchester.ac.uk
University Careers Service
The University Careers Service can help you to find part-time work during your time at the University, to prepare your CV and applications for full time work after graduation, and to research job opportunities. In addition the Service runs several job fairs across Manchester throughout the year.
Personal and Academic Development Programme (PADP)
From the beginning of your course, and as part of the Professional Studies course unit, you will be encouraged to develop a Personal and Academic Development Programme (sometimes called a Personal and Academic Development Profile). Working with a PADP involves using the framework provided to:
- reflect on your aims, needs, existing and developing skills
- plan your choice and timing of course units
- note down reflections, questions, concerns in relation to the above
This then forms a basis for discussion with your Personal Tutor. This process will take place at key moments during your study so that you can look both back on what you have already done and forwards to the next stage of your programme. In later years of the course profiling concentrates on clinical and professional skills. You will be asked to complete a Professional Skills Development Profile (PSDP) and a Clinical Reflective Logbook which records clinical experience and performance and your reflections on your clinical needs and development.
Student Representation and Feedback Mechanisms
There are a variety of ways in which students are able to provide feedback on different aspects of BSc Healthcare Science (Audiology) Programme. These vary from informal feedback by individual students to staff to the formal University Complaints and Appeals Procedures. These different pathways are designed to enable students themselves to have the opportunity to feed into the ongoing development of the Programme and in doing so to enhance the satisfaction of their own student experience and those of future years.
Student feedback is incorporated into the running of the degree programme. It should be noted that effective communication with students with their views taken into account as stakeholders in the whole process is key to the maintenance of standards and enhancement of academic quality.
Each cohort or year group is invited to elect a student representative. These representatives are to be responsible for keeping in close contact with the students within their year and discussing any problems that arise with the appropriate tutor(s) or lecturer(s). At the beginning of each academic year any student interested in becoming a student representative will be asked to submit a 150 word manifesto to Ryan Hurst, Student Rep Co-ordinator detailing why they would like to be nominated. If there are more than two volunteers the year group will be asked to elect their chosen representative. The names of the student representatives for each year will then be given to the Programme Director. These names will also be circulated to staff and students.
- Informal Feedback to Staff
Informal feedback regarding a particular course unit can be made at any time to individual staff member delivering the course unit, or to the Course Unit coordinator. Such feedback is often helpful in terms of delivery style etc.
- Feedback to Academic Advisor
Both informal and formal feedback can be made via your Academic Advisor, either at scheduled tutorials or by appointment. Records of such feedback are normally made unless anonymity is requested.
- Feedback via Year Representatives to Staff
Feedback to members of staff can be made at any time via your year rep. This is particularly appropriate if concerns a number of students or the student with the concern wishes to remain anonymous.
- Feedback to Programme Director (directly or via year representative)
If a student wishes to raise an issue and they feel unable to approach their Academic Advisor (for whatever reason) then they can approach the Programme Director directly (usually by appointment). The Programme Director will then either try to address the issue informally, or take it to the Programme Committee or Student Progress Committee.
- Feedback via Year Representative to the Programme Committee or Staff-Student Liaison Committee (SSLC)
SSLC meetings are held twice per (usually February and April/May). Prior to these meeting, the student reps. solicit items to be raised from members of their year cohort. These items are presented to the meeting by the reps. The meeting usually consists of the student reps. and deputies (or their nominees), plus the Programme Director, Clinical Director, Undergraduate Examinations administrator and the School Student Support/Quality Assurance Administrator. The minutes of this meeting are then fed into the Programme Committee meeting. Following the Programme Committee, the minutes of the SSLC along with documentation of any actions deemed appropriate by the Programme Committee are published on Blackboard and any major changes to the programme resulting from these actions are documented in an amendment to the Programme Handbook or the following year’s handbook as appropriate.
- Course Unit Feedback Questionnaires
The usual mechanism for students to provide feedback on individual course unit content and/or delivery is via the electronic course unit questionnaires. These are standard, anonymous, University-wide questionnaires used for all course units. The results of these are given back to course unit tutors and presented to the Programme Committee. For any course unit scoring poorly (i.e. less than zero on a scale of -2 to 2) the Programme Committee will require submission of an action plan by the course unit tutor to address the issues raised. It is these questionnaires that form the main assessment of students’ satisfaction in the teaching and learning process at School, Faculty and University level. In addition to the questionnaire, a qualitative feedback is also used where students can make suggestions on how to improve the course unit – these are fed back via the School Level to the course unit lead.
- Instant online anonymous student to teacher feedback
In the 2019/20 academic year the Healthcare Science (Audiology) programme was part of a trial in which programmes used a new anonymous instant feedback system which was called “Feedback Now”. This system allowed students to give anonymous feedback (positive or negative) about their learning experiences at any time, online, throughout the year rather than waiting until the end of semester Course Unit Evaluations. The programme team will continue to trial and use new feedback mechanisms to allow instant student to teacher feedback.
- Placement Evaluations
After each placement students are asked to fill in a placement evaluation form. This can be either downloaded off Blackboard (Year 1 and 2) or completed through an on-line survey (Yr 3). Completion of the form remains anonymous but student responses are analysed by University staff and a summary of the results are then feedback to placement teams so that they can monitor and develop strategies to continue to enhance placement learning. Students are also encouraged to provide a more reflective account of their placement experiences in their Personal Portfolio of Learning and Application. Although this feedback is not anonymous it is only read by clinical tutors and is not shared directly with placement teams but any reoccurring themes will be discussed with placement coordinators.
- Peer Mentoring
Peer mentoring is a student-to-student support programme where higher year students provide support to lower year students. The scheme is student owned and student lead and is designed so that students feel well supported particularly during their first year of study. Lower year students will have the opportunity to discuss any concerns or worries they have with higher year students and when appropriate this may be passed onto the staff co-ordinator or future peer mentors in order to improve first year support mechanisms. One example of where the peer mentoring scheme has enhanced the first year experience has been a guided tour around all the relevant discipline areas in the library.
- Students as Partners
Students as Partners supports and facilitates student-led activities and has worked with programme staff in providing an independent evaluation of student experiences, particularly in regard to new initiatives.
- Student Union Representatives
In addition to course unit representatives, Student Representatives are elected by the University of Manchester Student Union (UMSU) at both School and Faculty level. The Faculty representative sits on the Faculty Undergraduate Teaching and Learning Committee and represents the views of students at this level.
Handy-tip: University Degree programmes are designed to provide students with learning opportunities – this is a partnership with students and to help improve the student experience it is important that students engage, not just in the learning process, but also in the development of the programme – your engagement and feedback is an important part of the programme development and may change come about as a result of student comments. It is important to recognise though that not all suggests can be acted on but we will endeavour to explain the reason in such situations.
Complaints and Appeals
Given the variety of staff/student interactions that form part of any degree programme, it is inevitable that some disagreements will arise and that complaints may be made. In the vast majority of cases complaints and disagreements are resolved by positive discussions, usually with the subject tutor, personal tutor and/or the Programme Director. It is in the interests of all parties that these discussions are conducted in a spirit of reconciliation. In the unlikely event that such discussions are not effective in resolving the issues, written formal appeals and complaints by students can be made, and should be addressed to Sally Bray, Head of Academic Services, Faculty of Biology, Medicine & Health, Simon Building.
Academic Appeals
If you wish to appeal against the decision of an Exam Board, including exclusion from the course; you are advised to contact your personal tutor or the Programme Director first, to try to resolve the issue at a local level. However, if you decide to make a formal appeal you should submit the request in writing with supporting evidence to the Head of Academic Services within twenty working days of notification of the result or decision.
An appeal may be made only on grounds alleging:
- that there exists or existed circumstances affecting the student’s performance of which, for good reason, the Board of Examiners or Special Circumstances Committee may not have been made aware when the decision was taken and which might have had a material effect on the decision [Note: if students wish to appeal on such grounds, they must give adequate reasons why this information was not made available prior to the decision being made.];
- that there had been a material administrative error or procedural irregularity in the assessment process or in putting into effect the regulations for the programme of study of such a nature as to cause significant doubt whether the decision might have been different if the error or irregularity had not occurred;
- that there is evidence of prejudice or bias or lack of proper assessment on the part of one or more of the examiners;
- that the supervision or training of the student in respect of research for a dissertation or thesis or equivalent work was unsatisfactory to the point that his or her performance was seriously affected.
An appeal which questions the academic or professional judgement of those charged with the responsibility for assessing a student’s academic performance or professional competence shall not be permitted.
The full appeal policy can be found at the following site:
http://documents.manchester.ac.uk/DocuInfo.aspx?DocID=1872
Transfers and Withdrawals from the Programme
Whilst we hope that all students will continue to enjoy their study on this programme, we understand that occasionally students decide that a particular programme of study is not for them. In such cases we strongly advise that students meet with their Academic Advisor or the Programme Director prior to withdrawal in order that the best options for the student can be considered. Whilst we obviously don’t want to lose students, we will fully support those who decide that the programme is not for them and we will help them in any applications to transfer to other programmes. For example, students may decide that they want transfer to other Healthcare Science specialisms (e.g. Neurophysiology or Vision Science) which are not offered at the University of Manchester. Such requests to transfer would be fully supported by us, but would ultimately depend on the institution that the student is applying to transfer too. Such transfers would be dealt with on a case-by-case.
For students wishing to withdraw completely from their study, again we would strongly recommend that they discuss their options with their Academic Advisor or the Programme Director prior to making a decision.
For any student who wants to transfer or withdraw, we would require a signed letter for our records and we would also ask the student to complete an exit questionnaire which asks about students’ experiences and their reasons for withdrawal. This latter is important to us as it helps us identify any issues that students have with the Programme.
Handy-tip: If you decide that the Healthcare Science (Audiology) programme isn’t for you then please talk to your academic advisor and/or the programme director – we want what is best for you, and if you decide that you want to leave the programme we will support you in that decision.
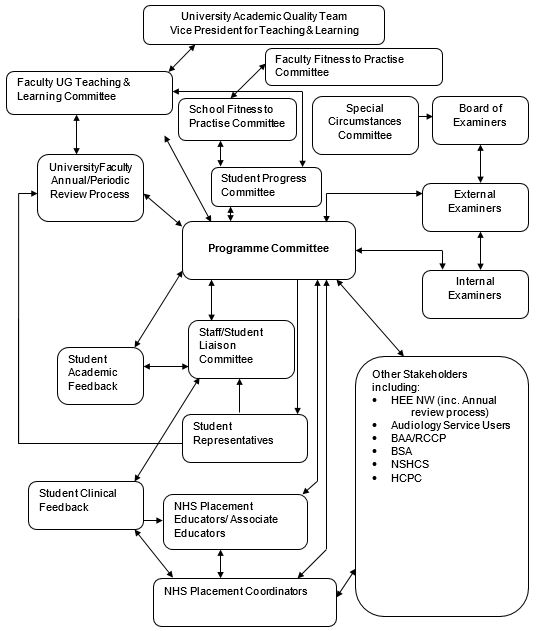
Useful Internal Links
The following links provide a variety of useful information to help you through your studies.
- Student Portal – access your email, calendars, blackboard, library services and more at:
https://www.portal.manchester.ac.uk/ - Student Services Centre –A-Z of services – essential advice, information and guidance for students at The University of Manchester:
http://www.studentnet.manchester.ac.uk/crucial-guide/
The following links relate to specific University Policies and Procedures. Please note that these must be consulted alongside information in this handbook as this programme may differs from University Policies where professional body accreditation requires it to do so.
- University of Manchester student-related policies and documents:
http://www.regulations.manchester.ac.uk/ - Academic Appeals:
http://www.regulations.manchester.ac.uk/basic-guide-academic-appeals/ - Work & Attendance Policy:
http://www.regulations.manchester.ac.uk/policy-on-recording-and-monitoring-attendance/ - See also:
http://www.regulations.manchester.ac.uk/regulation-xx/ - Conduct & Discipline of Students Regulation XVII Sept 2014:
http://documents.manchester.ac.uk/DocuInfo.aspx?DocID=6530 - Dignity at Work and Study Procedures for Students:
http://documents.manchester.ac.uk/DocuInfo.aspx?DocID=22733 - Health and Safety Policy:
http://documents.manchester.ac.uk/DocuInfo.aspx?DocID=654
The following links provide information that is particularly relevant to your health and wellbeing and how these aspects fit into your studies on a vocational clinical programme.
- Occupational Health Services for Students:
http://www.studentnet.manchester.ac.uk/occupational-health/ - Student Mental Health Policy:
http://documents.manchester.ac.uk/DocuInfo.aspx?DocID=1892 - Fitness to Practice:
http://documents.manchester.ac.uk/display.aspx?DocID=50549
The following links provide information relevant to your personal development and related issues
- Careers Service:
http://www.careers.manchester.ac.uk/ - Personal Development Planning:
http://www.tlso.manchester.ac.uk/personaldevelopmentplanning/ - Adults Returning to Education Guide:
http://www.manchester.ac.uk/undergraduate/maturestudents/guide/ - Students’ Union:
http://manchesterstudentsunion.com/
The following section gives useful links to external sources of information that are relevant to your studies
- Student finance information:
https://www.gov.uk/student-finance - Student Loans Company:
http://www.slc.co.uk - British Academy of Audiology:
http://www.baaudiology.org/ - British Society of Audiology
http://www.thebsa.org.uk/ - The National School of Healthcare Science
https://www.nshcs.hee.nhs.uk/ - The Registration Council for Clinical Physiologists
https://www.rccp.co.uk/ - Health and Care Professions Council (HCPC):
http://www.hcpc-uk.org.uk/ https://www.hcpc-uk.org/ - Health Education England (North West)
https://hee.nhs.uk/hee-your-area/north-west https://www.hee.nhs.uk/about/how-we-work/your-area/north-west
Appendices
Appendix 1 BSc Healthcare Science (Audiology) Assessment/Examination marking criteria
Examples of feedback words and phrases used according to marking range, and overall range descriptor guidance.
| Range | Feedback descriptors |
| 0-9 |
Profoundly inadequate Highly Deficient |
| 10-19 |
Severely inadequate Very Deficient Incomplete |
| 20-29 |
Inadequate Deficient Some attempt Confused |
| 30-39 |
Insufficient Partial Some awareness |
| 40-49 |
Sufficient Adequate Basic |
| 50-59 |
Good Clear Fair Competent Reasonable Coherent |
| 60-69 |
Very Good Sound Effective |
| 70-79 |
Excellent Detailed Compelling Lucid |
| 80-89 |
Outstanding Sophisticated Innovative Insightful Ambitious Perceptive Advanced |
| 90-100 |
Exceptional Authoritative Very Advanced |
* Note, however, that when qualifying comments on structure, phrasing, vocabulary, etc., the word ‘poor’ can be a descriptive and helpful tool. However, the word ‘poor’ should not be used in isolation.
| Level four 90 – 100% | Level five 90 – 100% | Level six 90 – 100% |
Content
Structure
Style
|
Content
Structure
Style
|
Content
Structure
Style
|
| Level four 80 – 90 % | Level five 80 -90 % | Level six 80 –90 % |
Content
Structure
Style
|
Content
Structure
Style
|
Content
Structure
Style
|
| Level four 70 – 80 % | Level five 70 – 80 % | Level six 70 – 80 % |
Content
Structure
Style
|
Content
Structure
Style
|
Content
Structure
Style
|
| Level four 60 – 69 % | Level five 60 – 69 % | Level six 60 – 69 % |
Content
Structure
Style
|
Content
Structure
Style
|
Content
Structure
Style
|
| Level four 50 – 59 % | Level five 50 – 59 % | Level six 50 – 59 % |
Content
Structure
Style
|
Content
Structure
Style
|
Content
Structure
Style
|
| Level four 40 – 49 % | Level five 40 – 49 % | Level six 40 – 49 % |
Content
Structure
Style
|
Content
Structure
Style
|
Content
Structure
Style
|
| Level four Fail 33 – 39% | Level five Fail 33 – 39% | Level six Fail 33 – 39% |
Content
Structure
Style
|
Content
Structure
Style
|
Content
Structure
Style
|
| Level four Fail 0 – 32% | Level five Fail 0 – 32% | Level six Fail 0 – 32% |
Content
Structure
Style
|
Content
Structure
Style
|
Content
Structure
Style
|
Appendix 2 Conduct and Discipline of Students (Regulation XVII)
Students must also refer to the HCPC standards of conduct, performance and ethics, available at http://www.hpc-uk.org/standards/standards-of-conduct-performance-and-ethics/
The conduct regulation can be found here: http://documents.manchester.ac.uk/display.aspx?DocID=6530
Appendix 3 Professional behaviour and conduct
Ground rules on Professional Behaviour and Conduct
Certain behaviours are accepted as appropriate for professionals and you should learn to incorporate these into your performance and demeanour, particularly when attending clinic placements. As a student, you represent the Programme, the School and the University. Your communication with patients and other professionals may be through personal contact, writing or telephone etc. The importance of developing professional skills and behaviour as well as scientific and technical skills cannot be over emphasised. As a student, you may work with patients who differ in many respects. You will enjoy working with some age groups more than others and like some individuals more than others. You should treat all patients with respect, integrity and compassion and without any form of prejudice. You must make objective clinical judgements.
You may initially be nervous in the clinic, especially in the first semester, but through a combination of your demeanour (e.g. dress appropriately, establish rapport with patient etc) and clinic performance, you must make the patient believe that you will provide a comprehensive quality clinical service. It is important for you to present yourself as a person confident in your skills (without attempting to exceed your area of knowledge). The better prepared you are for each clinic session, the easier it will be for you to appear confident, even when you are a little nervous. This includes reviewing and practising unfamiliar techniques and setting up and testing equipment in advance. You will also become more confident when discussing test procedures, results and recommendations as your training advances. It may be necessary for you to research information about certain disorders or diseases mentioned in the referral letter before you commence your clinic session. There will be certain categories of patients and test procedures that you will not be expected to undertake until you are more advanced in your training.
Confidentiality
You may be involved in issues of client confidentiality early in the course. You are required to respect patient confidentiality and you must understand the importance of not revealing, without prior authorisation, any professional or personal information about the patient you have seen (or observed) in the clinic. In practice, this means that you should avoid discussing patient details in public places, avoid identifying the patient unless necessary, and avoid leaving case notes and other confidential information in public places. You should not remove case notes from the clinic without permission.
Dress Code
Individuals are typically judged on their appearances. The way you look may inspire confidence or trust. The manner in which you dress and even wear your hair may detract or enhance your clinic sessions. You do not need to buy expensive clothes but you must appear professional. Use common sense. While on placement, both male and female students should avoid wearing jeans, tee-shirts, sport shorts, or provocative clothing. You should consider modesty and comfort in situations where there is frequent kneeling and bending. It is traditional practice for male students to wear a shirt and tie with smart trousers. Female students may also wear smart trousers as well as skirts and dresses. White lab coats are not worn in the department but may be provided at other clinics. Tidiness of hair and beard is requested, and if the hair is sufficiently long to fall over the face when examining a patient, there should be some arrangement to prevent it from doing so. These comments may also apply to certain items of jewellery. You will be excluded from clinic sessions if your supervisor feels that your appearance is unsatisfactory.
(SEE ALSO: Appendix 2 Conduct and Discipline of Students (Regulation XVII), Appendix 4 Religious Events and Festivals,Appendix 5 Communication & Dress Code for Healthcare Science (Audiology) Students,Appendix 6: Drugs and Alcohol Policy)
Appendix 4 Religious Events and Festivals
We recognise that there may be occasions when students are unable to attend The University or clinical placement due to the observance of religious events. You are required at the beginning of each academic year to notify the Programme Director AND the Director of Clinical Education for the Audiology programmes, in writing of any date/s on which you intend to be absent from the University due to the observance of religious events falling within the academic year. These dates will be noted and kept on your file. You must notify the University of any absences due to religious events in the same way as for any other absences.
Clinic Placements
Due to the scheduling of placements and the demands made on our partner placement providers, it may not always be possible to arrange clinical placement experience to compensate for absences during your allocated clinical placement period. Any dates of necessary absence which coincide with clinical placements should be highlighted and must be reported to the Clinical Director at the start of the academic year.
You should be aware that poor attendance (less than 80%) across the year may affect your progress through the programme.
Should formal examinations fall on significant religious dates, the School will try to make alternative arrangements for those students who would be effected. This will, where possible, be undertaken in co-operation with representatives from relevant religious communities. If a student has any issues surrounding prayer times they should contact the School, or if on placement their line manager, they will discuss the matter with the student to establish if suitable arrangements can be made.
Appendix 5 Communication & Dress Code for Healthcare Science (Audiology) Students
The University of Manchester
All health and social care professionals are bound by the guidance and rules of conduct set out by the Department of Health and the relevant regulatory or representative body, e.g. the General Dental Council (GDC), General Medical Council (GMC), Nursing and Midwifery Council (NMC), Royal Pharmaceutical Society of Great Britain and Pharmaceutical Society of Northern Ireland, the Health Professions Council (HCPC), the British Psychological Society (BPS) and the General Social Care Council (GSCC). These in turn define the standards for health and social care education in the UK in settings in which a student is interacting with patients, clients or service users.
Communication, both verbal and non-verbal, including dress code, is an important element in ensuring that these standards are maintained.
Communication
The General Medical Council document “Good Medical Practice” 1 defines the basic components of effective communication as:
- listening to patients, clients and service users, asking for and respecting their views about their health, and responding to their concerns and preferences;
- sharing with patients, clients and service users, in a way they can understand, the information they want or need to know about their condition, its likely progression, and the treatment options available to them, including associated risks and uncertainties;
- responding to the questions of patients, clients and service users, and keeping them informed about the progress of their care;
- making sure that patients, clients and service users are informed about how information is shared within teams and among those who will be providing their care.
All health and social care students should adhere to these principles in communication and other skills training, discussion and assessment. The GMC document also stresses the importance of ensuring, wherever practical, that arrangements are made to meet the language and communication needs of patients, clients and service users.
Dress
It has been shown that non-verbal communication is at least as important as verbal communication, so how a student or health and social care professional appears to patients, clients, service users, relatives, professionals or colleagues may communicate as much as what is said. Extremes of dress compromise communication channels between health and social care students and other patients and professionals, regardless of either party’s gender, or cultural or ethnic background. Styles of dress or articles of clothing that introduce barriers to communication or that compromise, or could potentially compromise, hygiene must be avoided.
Styles of dress should inspire confidence and add to, not detract from, effective and sensitive communication. In general, students should be clean and smartly dressed. Thus the following are not permitted in settings in which a student is interacting with patients, clients or service users:
- T-shirts with slogans;
- Visible body art or nail varnish or extensions2;
- Extremes of hair styles3;
- Body and face jewellery (except small stud earrings and wedding rings)4;
- Wrist bands/string5;
- Revealing clothing;
- Open-toed sandals (all footwear should be low-heeled and well-fitting round the ankles)6;
- Trainers7;
- Clothing that covers most of the face8. Peaked caps, hoods, and the Niqab are examples of unacceptable clothing in this context. Clothing like the Hijab that only obscures the hair and the top of the head is, however, acceptable. This applies not only in clinical settings but also in educational elements of the programme where communication skills are relevant, such as some types of group work and role-play exercises. The University also reserves the right to check the identity of students who wear clothing that covers most of the face (as defined above) on key occasions such as examinations;
- Strong odours, perfumes or aftershaves9.
For cross-infection reasons, NHS Trusts may not permit healthcare workers (including students) to wear wristwatches and ties other than bow ties.
The following are examples of good practice:
- Wearing approved clothing;
- Wearing identification badges or University/Trust identity passes10;
- Tying back of hair if it interferes with, or adds risk, to a clinical interaction11.
When on NHS premises such as a hospital Trust or a Primary Care Trust, a community setting such as a GP practice, or in the homes of patients, clients and service users, students should dress according to both the University’s and the appropriate local guidelines and regulations.
References
1‘Good Medical Practice’, GMC 2006, paras 22 and 23
2‘Standards for Student Dentists and Student Dental Care Professionals’, University of Manchester School of Dentistry, 2006, pages 3-4 (internal document)
3‘Standards for Student Dentists and Student Dental Care Professionals’, University of Manchester School of Dentistry, 2006, page 4 (internal document)
4‘Standards for Student Dentists and Student Dental Care Professionals’, University of Manchester School of Dentistry, 2006, page 3 (internal document)
5‘Standards for Student Dentists and Student Dental Care Professionals’, University of Manchester School of Dentistry, 2006, page 3 (internal document)
6‘Health and Safety Policy and Clinical Code of Practice’, Central Manchester and
Manchester Children’s University Hospitals NHS Trust Dental Division, 2005, page 17
7‘Standards for Student Dentists and Student Dental Care Professionals’, University of Manchester School of Dentistry, 2006, page 4 (internal document)
8‘Standards for Student Dentists and Student Dental Care Professionals’, University of Manchester School of Dentistry, 2006, page 3-4 (internal document)
9‘Standards for Student Dentists and Student Dental Care Professionals’, University of Manchester School of Dentistry, 2006, page 4 (internal document)
10‘Uniform and Dress Code for Doctors: Guidance from the Central Consultants and Specialists Committee’, BMA, 2007
11‘Uniform and Dress Code for Doctors: Guidance from the Central Consultants and Specialists Committee’, BMA, 2007
Other Sources of Information
‘Tomorrow’s Doctors’, GMC, 2003
‘Medical Students: Professional Behaviour and Fitness to Practise’, GMC/MSC, 2007
Appendix 6: Drugs and Alcohol Policy
Faculty of Biology, Medicine & Health
Misuse of Non-Prescription Drugs and Alcohol: Student Policy and Procedures
The policy can be found here: http://documents.manchester.ac.uk/display.aspx?DocID=29039
Appendix 7 Forms to be Signed by students
The following appendix contains detail of forms that are signed by students at the beginning of the year. These signed forms are then kept in the students’ files for our records.
Forms completed prior to registration:
- Pre-Acceptance Health Screening Questionnaire
For students that have been made a conditional / unconditional offer of a place to study at The University of Manchester we need to be aware of any disabilities or health conditions which could be relevant to your proposed course of training and future employment. Where considered appropriate we can then advise your chosen School of the need to consider any reasonable adjustments or additional support needs both in your own and future patients/pupils interests.
Forms completed during registration process:
- Audiology Clinical Placements: North West Area
Statement of understanding that the mandatory Clinical placements which form part of the Audiology degree programme could take place within any of the North West (including Stoke-on-Trent and Wrexham) clinical placement teams (as attached details) and that clinical placement allocation could be assigned within any of these North West Placement teams
- Disclosure and Barring Service (DBS) and Health Check
This form is completed by new 1st year students prior to registration. Its purpose is to indicate that students acknowledge that although students are being allowed to register, their place on the course is contingent on satisfactory DBS clearance and Health Checks.
- School of Health Sciences Plagiarism Form
This form is for all students and must accompany any submitted assignment. It states that the student has “received, read, understood and agree to abide by the departments statement on plagiarism.”
- Code of professional conduct and fitness to practise for healthcare students
This document provides the basic ground-rules for your behaviour as trainee health-care scientists including aspects such as personal behaviour, behaviour towards others, learning, barriers to learning or professional practice, duty of care, duty of report and confidentiality.
- Service User / Practical Subject Consent
This document is a declaration of acknowledgement that as a student on this programme you will be required to undertake a range of practical and clinical procedures and that you also agree to be a subject for fellow students and staff to carry out procedures on you.
Forms Completed in Subsequent Years:
- Health & Security Status Update
This form is for returning students to sign a declaration that there has been no change in physical and mental health, and security status.
Appendix 8 Guidance on Social Networking for Healthcare and Social Care Students
What is the purpose of this document?
This document provides advice and guidance for healthcare and social care students about the benefits and potential dangers of social networking and suggests ways in which their personal and professional interests, and those of others, can be protected while in the online environment.
What are social networking sites used for?
Social networking is a popular online activity: millions of people of all ages and backgrounds use social networking sites every day. Online social networking sites, such as Facebook,
Twitter, MySpace and Bebo, are used:
To keep in touch with friends, both in words and through sharing music, video and other types of files (YouTube is also used for sharing videos, and Flickr for sharing images, online).
For educational and professional benefit, through sharing information about the latest developments in treatments and practice, problem-solving, encouraging participation, and community building.
To forge new relationships based on common interests.
To make their views and opinions known.
To take part in discussions on virtually any subject.
People often interact with social networking sites over long periods of time and, occasionally, excessive activity of this nature may have detrimental effects on their work or study.
What is the social networking environment?
It is important to remember that social networking sites are public and therefore, in theory, accessible to anybody. In many cases, ownership of the material posted on them belongs to the site, not the person who posted it, and so sites such as Facebook are free to use it in any way they see fit. Material posted online remains there permanently, if not as part of an active page then as part of easily-accessible ‘cached’, i.e. historical, versions of it.
Who visits social networking sites, and why?
Anybody can visit social networking sites and gain access to the information that is uploaded to them. These people include:
Your intended audience, i.e. your friends, colleagues and others, to share information and to keep in touch.
Potential employers, who are, increasingly, using social networking sites to gather information about people who have applied for positions within their organisations.
Criminals, including sexual predators who could use information about you to compromise your safety or wellbeing, and fraudsters, who could steal information about you and impersonate you online, to your potential cost.
The police, as part of investigations into illegal activities.
Professional healthcare and social care bodies such as the General Dental Council, General Medical Council, General Pharmaceutical Council, General Social Care Council, Health & Care Professions Council, and Nursing & Midwifery Council, who may access information directly or be asked to investigate material referred on to them by other people.
Patients, clients and other service users, who may be looking for healthcare or social care information in general, or for your views and comments in particular. Your professional relationship with your patients, and your career, could be compromised at any time by indiscriminate posting of details about patients or inappropriate information about yourself.
What precautions should be taken when social networking?
The same ethics, morals and penalties apply to online social networking as to any other activity. This is particularly true for healthcare students and professionals, who are expected by the University of Manchester, their professional bodies, and by the public generally, to meet the same standards of behaviour both in and out of their professional settings. Healthcare and social care students from Schools in the Faculty of Biology, Medicine & Health should therefore conduct themselves appropriately online, and take reasonable precautions to ensure that the information they upload cannot be used in a way that could place them, or others, at a disadvantage, either personally or professionally, now or at any time in the future.
The following pointers may be helpful:
Do everything that you can to limit access to your posts to those for whom they are intended. Change security settings if possible to restrict unwanted access.
Consider the language and terminology that you use when you are online and make sure that it is appropriate.
Avoid posting personal information such as phone numbers or personal addresses, of you or anybody else, since these may fall into the hands of criminals.
Use your common sense. If you feel that a post, a picture, or a video that you are about to upload might have repercussions for you later, or might not be in good taste (e.g. it relates to sexual activity or inappropriate behaviour, or it expresses inappropriate views), then simply do not post it. Once it is online it is there for good.
Make sure you are thinking clearly before you go online. If, for any reason such as the effects of medication, stress or inebriation, your judgement might temporarily be impaired, you may be tempted to post something that you otherwise would not.
Do not post material that might be considered offensive and/or derogatory, that could cause somebody else to feel bullied, harassed, or that could harm somebody’s reputation. If you have a grievance about an individual related to your programme, follow it up through the recognised channels in the School, Faculty and/or the wider University.
Avoid posting confidential information about patients, clients and service users that could violate professional codes of conduct.
It is imperative that if you post anything about somebody else, including any images of them, it is done with their knowledge and consent. It might seem inoffensive to post images of friends, relatives, staff or other colleagues, but it might easily cause offence that you had not intended or could not have foreseen.
Try to make sure that the people to whom you give access to your information use it sensibly, and also that they themselves do not upload potentially incriminating material about you, which can be just as damaging.
Avoid joining any groups that could be seen as discriminatory or judgemental in nature.
Are there any related policies and guidance in the University?
The University’s Conduct and Discipline of Students (Regulation XVII) document states that a student may be liable to disciplinary action in respect of conduct which, amongst others: “involves violent, indecent, disorderly, threatening or offensive behaviour or language (whether expressed orally or in writing, including electronically) whilst on University premises or engaged in any University activity” and “involves distributing or publishing a poster, notice, sign or any publication which is offensive, intimidating, threatening, indecent or illegal, including the broadcasting and electronic distribution of such material”.
Regulation XVII also states that:
“the conduct covered (above) shall constitute misconduct if it took place on University property or premises, or elsewhere if the student was involved in a University activity, was representing the University, was present at that place by virtue of his or her status as a student of the University or if the conduct raises questions about the fitness of the student on a programme leading directly to a professional qualification or calling to be admitted to and practise that profession or calling.”
The University of Manchester’s Dignity at Work and Study Policies and Procedures give information about the nature and consequences of acts of misconduct while social networking, such as discrimination, bullying and harassment1, and the penalties that they may incur.
These policies should be read in conjunction with this guidance. The University’s Dignity at
Work Procedure for Students states:
“Any cases of harassment, discrimination and bullying will be taken very seriously by the University and, where necessary the appropriate procedure will be used to investigate complaints. Similar arrangements will be used in dealing with complaints made by members of staff or by visitors to the University.”
“Cases of proven harassment, discrimination or bullying may be treated as a disciplinary offence where it is not possible to reach a compromise or resolution. Some cases of harassment, discrimination or bullying if proven could result in dismissal for staff members or expulsion for students.”
In addition, the University’s Crucial Guide states that:
“The University expects its members to treat one another with respect. There are established procedures to use if you are dissatisfied with any aspect of the University’s facilities and services, and you are encouraged to use these procedures to bring such matters to the University’s attention. Inappropriate or defamatory comments about either the University or its members in any media (print, broadcast, electronic) contravene the University’s regulations and offenders may be liable to disciplinary action.”
What do the Professional Bodies say?
Professional body codes and guidance also explore the potential consequences of social networking activity:
General Dental Council: “Standards for Dental Professionals”
Paragraph 3.2, ‘Protect the confidentiality of patients’ information’:
1 Harassment is unwanted conduct that may create the effect (intentionally or unintentionally) of violating a person’s dignity or creating an intimidating, hostile, degrading, humiliating or offensive environment which interferes with an individual’s learning, working or social environment or induces stress, anxiety or sickness on the part of the harassed person.
Discrimination takes place when an individual or a group of people is treated less favourably than others because of their race,
gender, gender reassignment, marital status, status as a civil partner, disability, age, religion or belief, sexual orientation or other factors unrelated to their ability or potential.
Bullying can be defined as repeated or persistent actions, criticism or personal abuse, either in public or private, which (intentionally or unintentionally) humiliates, denigrates, undermines, intimidates or injures the recipient. It should, in particular, be borne in mind that much bullying occurs in the context of a power imbalance between victims and alleged perpetrators.
“(You must) prevent information from being accidentally revealed and prevent unauthorised access by keeping information secure at all times”.
Paragraph 6.3, ‘Be trustworthy’:
“(You must) maintain appropriate standards of personal behaviour in all walks of life so that patients have confidence in you and the public have confidence in the dental profession”.
General Medical Council: “Good Medical Practice‟
Paragraphs 56 to 58, ‘Being honest and trustworthy’
“Probity means being honest and trustworthy, and acting with integrity: this is at the heart of medical professionalism”.
“You must make sure that your conduct at all times justifies your patients’ trust in you and the public’s trust in the profession”.
“You must inform the GMC without delay if, anywhere in the world, you have accepted a caution, been charged with or found guilty of a criminal offence, or if another professional body has made a finding against your registration as a result of fitness to practise procedures”.
Nursing and Midwifery Council: “Guidance on professional conduct for nursing and midwifery students‟
“Good character is important as nurses and midwives must be honest and trustworthy. Good character is based on a person’s conduct, behaviour and attitude. It also takes account of any convictions and cautions that are not considered to be compatible with professional registration and that might bring the profession into disrepute”.
What conclusions can be drawn from all of this?
If the way you conduct yourself online breaks laws, or goes against the codes of practice set down by your professional healthcare or social care body, then you risk the same penalties as you would in any other setting. These include referral to the Faculty Fitness to Practise Committee and potential damage to your career, fines, and even imprisonment.
================================================================================================
Acknowledgement:
The Faculty wishes to acknowledge the work of Mrs Dianne Burns, School of Nursing, Midwifery and Social Work, whose document “Social Networking Sites and Student Issues” informed the content of this guidance.
Version 2, 9 June 2010
Appendix 9 Procedure for a Committee on Fitness to Practise
The Faculty of Biology, Medicine and Health Fitness to Practice Procedure is available online here:
http://documents.manchester.ac.uk/display.aspx?DocID=50549
SCHOOL OF HEALTH SCIENCES
Appendix 10 Health and Safety Policy
The School’s primary functions are research, teaching and engagement with the wider public through its social responsibility agenda. The School is keen to ensure that that these aims are achieved, so far as is reasonably practicable, with no adverse effect on the health and safety of anyone inside or outside the University.
It is the aim of the School to comply with the University’s general health and safety policy statement;
http://www.campus.manchester.ac.uk/healthandsafety/policy.htm
and to provide and maintain safe and healthy working conditions, equipment and systems of work for all staff, students, visitors and others.
The School will manage risks to staff, students, visitors and others through the process of hazard identification, risk assessment and management as far as is reasonably practical.
The allocation of duties for safety matters and the particular arrangements for implementing the policy are set out in this document.
The School will comply with any applicable legislation and seek to foster an approach for continuous improvement. We will engage in planning for safety within our operational plans should specific needs arise.
We will ensure effective communication across the School for health and safety matters and seek to involve staff and student representatives.
We will endeavour to make available adequate resources and to ensure we have competent staff who are fully trained in the specific health and safety areas designated to them.
We will ensure we have the necessary staff available for providing competent specialist advice to all staff and students as necessary.
Head of School
Appendix 11 Facilities for BSc Healthcare Science (Audiology) and BSc/MSc/Dip Audiology Students
The Laboratory is located on the 4th floor of A Block in room A4.12, and students may request access to equipment, from the Laboratory staff. There are several laboratory working rooms, where students carry out practical workshops and practical examinations. There are also rooms set up with equipment for developing practical skills on the Ground Floor of B Block (see below); these rooms are available from 9am to 5pm and students are strongly encouraged to make use of them early in the course. Laboratory staff are Keith Wilbraham and Alice Crutchley.
BG.20: Audiometric booths
4 x GSI Pello audiometers
1 xTympstar Protympanometer
A4.7:Is a general purpose teaching room and has no specific equipment. Equipment will be put in A4.7 to run practical classes and will change frequently. When there are inpending OSCEs or other practical tests suitable equipment may be put in A4..7 to enable practice.
BG.16: Vestibular and Evoked responses
Students will not access this room without supervision.
A4.11: Speech tests (parrot, FAAF etc)
Maintaining tidiness in the audiometry practical room (BG20) A key aspect of clinical professionalism is taking responsibility for leaving rooms and equipment clean and tidy, ready for the next user. This includes reporting faulty equipment and reporting the need for replenishment to the appropriate person. At the University of Manchester we expect the highest standards from all audiology students, undergraduate and postgraduate, in this respect. We do not expect any materials or equipment to go missing from these rooms, and we will take a very severe view of any such losses.
BG 20 has four audiometry booths, associated equipment, and a cupboard to keep material such as earplugs and insert earphone tips.
All students have the responsibility of ensuring the rooms and the equipment are kept in good order.
Audiometry room (BG 20)
- Ensure the audiometers are calibrated (stage A check) on a weekly basis.
- Ensure the booths and audiometers (and tympanometers whenever they are stationed in BG 20) are properly set up.
- Ensure there are adequate number of audiometry and masking charts.
- Ensure a good supply of: sterilizing wipes, ear-plugs, insert earphone tips, tympanometer tips, otoscope tips, batteries for otoscopes etc. The check-list should be consulted on at least a weekly basis to make sure that everything that is supposed to be in the cupboard is there.
- Ensure equipment such as tuning forks are stored in the cupboard in a tidy manner.
- Ensure general tidiness of the room.
. Groups should directly approach Keith Wilbraham or Alice Crutchley
for replenishment of supplies or any other issue that need to be brought into their attention.
- With many healthcare courses such as this one, the curriculum and the number of clinical hours are specified by external Professional Bodies and as such the FHEQ credit rating may not necessarily correspond with the number of hours associated with a unit, especially those involving clinical placement. ↑
- The normal University regulations allow compensation of up to 40 credits where unit marks are between 30 and 39% – Professional body requirements means that this is not applicable for this programme. ↑