1. General Information
Welcome to the School of Medical Sciences and the Faculty of Biology, Medicine and Health
Welcome to your Postgraduate Taught Programme in the School of Medical Sciences within the Faculty of Biology, Medicine and Health at the University of Manchester. The University has a worldwide reputation based on high quality teaching and research, and I am sure that your programme will provide a solid foundation for your future career success.
Within the School and the wider Faculty, our goal is to create an environment that allows you to excel and reach your full potential. Offering access to first-class facilities and strong links with regional health-service providers, our postgraduate programmes are designed to meet the diverse needs of all our students. The curriculum of our taught programmes provides the knowledge and skills you will need in your subject area and all our Masters programmes include an opportunity to carry out an independent research project on topics spanning all areas of biomedical research from molecular to experimental biology and clinical medicine. While subject areas cover a broad range, all our taught programmes have two common aims:
- To develop your skills in your chosen field of study
- To enhance your knowledge within the field you have chosen. Whether you are a graduate, professional or have a clinical background, the programmes have been tailored to meet your specific needs
As a student of the School of Medical Sciences, you will be expected to take responsibility for your degree, within a supportive environment that fosters your development and helps prepare you for your future career. This handbook will be a useful resource as you progress through your programme. It provides programme-specific information that I am sure that you will find helpful throughout your study. If however, you have questions or would like some further advice, please do not hesitate to contact the people listed in this handbook for further information and assistance.
I wish you every success as you embark upon your programme, and in your future career.
Dr Helen Jopling
Director of Education
Welcome to Physician Associate Studies
This handbook contains information on the aims, objectives, structure, content, admissions, assessment and programme management for the programme. We hope that you will find it a useful source of information, but please feel free to approach the programme organisers if you have any other queries.
The first year of the course begins with a four-month period of intensive study where you will develop your understanding of the essential basic and clinical sciences that underpin safe and effective practice. After this 16-week taught block, you will rotate through a series of medical and surgical placements, each incorporating a short period of university-based teaching.
The curriculum is built around a core content of common clinical situations that are organised according to their relative complexity. The content of each taught block is delivered using a problem-based learning (PBL) approach through the study of clinical cases/scenarios. Each case integrates elements of the taught content, so you will learn about and reflect upon the related biomedical, behavioural and population sciences appropriate to the case.
You should read the handbook in conjunction with related University documentation, for which links are provided in this Handbook. In particular, at the start of your programme, you should read the University handbook (webpages) entitled ‘Crucial Guide’, which links to all the generic information required by students at the University. You can find it at: www.studentnet.manchester.ac.uk/crucial-guide/ As clinical students you will also need to comply with additional requirements surrounding fitness to practice, standards of behaviour and dress during clinical placements, the minimum standards guide for placements, GMC/RCP standards documentation and HEE programme handbooks. Because this is rather a lot of information, we will introduce you to each component at the appropriate time.
If you have any queries or comments, or would like to contact us for advice and guidance on any issues, please do not hesitate to get in touch. You can reach us by e-mail on programmesupport.smspgt@manchester.ac.uk
On behalf of the University of Manchester and the programme team I wish you an enjoyable and successful time on the programme.
Physician Associates Programme Director
List of immediate contacts
| Assessment : | For general assessment queries |
| Student Support: | For general student queries email: |
| Curriculum & Programmes: | For teaching activity queries including simulation support |
| Clinical Placements | Questions about clinical placements should be emailed to sms.clinicaldelivery@manchester.ac.uk |
| Professional Portfolio Development | You should contact your assigned Academic Advisor |
| PA Student Representative: | At the beginning of the programme your year group will be asked to elect two students to represent you. The student rep is required to feedback to the programme director and administrator on any issues or queries that the students have. They will be required to attend 2-3 staff/student liaison meetings throughout the year. |
| eLearning Support: | See Support folder on programme homepage in Blackboard for resources that will help you to use Blackboard. For help in using a particular tool within Blackboard (e.g. assessments or discussions), use context sensitive help which appears in Blackboard as a link on the top right hand side of the page you are using.
You can also contact eLearning support at elearning@manchester.ac.uk. However, you must enter “FBMH eLearning – Physician Associate Studies” in your email subject header. This will help ensure your request reaches us quickly. |
| General IT Support: | Contact the Service Desk via the online Knowledge Base http://servicedesk.manchester.ac.uk/portal/ss and report any IT failure or submit a service request. Call the Service Desk on: 0161 306 5544 (or ext. 65544). Telephone support is available 24 hours a day, 7 days a week. |
Online Skills Training Resource
The Faculty has developed a skills training resource to support you through your postgraduate taught programme. This online material should supplement the assessed learning material and activities undertaken in your taught programme.
Accessing the online skills resource
You can access Blackboard through the My Manchester portal (http://my.manchester.ac.uk). The skills training resource is available in an academic community space available to all registered PGT students in the Faculty through Blackboard.
If you cannot see these units in your Blackboard please contact your Programme Administrator.
Content
Full details of all these resources can be found in the introduction to each unit. These resources have been designed to give you formative feedback on your progress through them. If you experience any problems and would like to talk to someone please contact your Programme Director. If you have questions about referencing and how it applies to your own work, please contact your Programme Director or dissertation supervisor/module lead.
| Research Methods* | This course is spilt into 2 units that cover introductions to study design and dissertation skills. It has a number of online quizzes where you can test your knowledge. |
| Introduction to Statistics* | The course provides a valuable foundation for understanding and interpreting biostatistics. It aims to provide you with the fundamentals of quantitative analysis. |
| Presentation Skills | This short interactive unit is designed to help you to enhance your presentation skills. Regardless of whether you are presenting in public, preparing for conferences, an oral examination or more informal settings this unit will give you the tops tips to improve your delivery. The course also includes a unit on influencing effectively, alongside the presentation and poster information. |
| Qualitative Research Methods* | This unit has been designed to give you an introduction to Qualitative Research. |
* NOTE: the material in this online resource is for reference and formative learning purposes only. In some of your taught programme you may be required to undertake assessed course units for Research Methods, Qualitative Research or Statistics. If your programme involves taught units then you should refer to the Blackboard material relating to that course unit. Please contact your Programme Administrator if you are unsure which material relates to your assessed work. You will still be able to refer to the online skills resource in later years.
Mandatory Introductory Courses
All students are automatically enrolled onto the Blackboard introductory unit that provides information on Health and Safety and Academic Malpractice.
Completion instructions for each of these sections are clearly defined within the course. All assessments must be completed within a month of you starting your programme, with the academic malpractice driving test completed before the first piece of summative assessment is submitted.
You must achieve 70% in each of the Health and Safety elements and 100% in each of the Academic Malpractice Driving Test elements to pass.
Health and Safety
Before you visit the University campus, please take time to read the University’s Health and Safety Policy.
Communication with Students
Please note that only Blackboard, the University e-learning platform and your allocated student university email address will be used as official communication by University staff. It is your responsibility to ensure that you can access and read emails from this source.
Students are required to keep the University informed of any change to their personal circumstances such as change of name or address. Changes can be recorded by the student via their own personal online record. It is also essential to inform your programme team if you do not intend to return to the next session of the course, if, for example, you are moving away.
Security
If you are going to be visiting the University campus for any purpose, please note that the University of Manchester cannot be held responsible for your personal property. Please keep your belongings with you at all times. Items left unattended may be removed and destroyed or damaged without warning by University Security Services.
2. Overview of the Programme
Aims
The programme follows an accelerated graduate-entry model, incorporating many existing sector-wide standards for the rapid development of core clinical competencies and professional behaviours alongside recent innovations in medical education. The programme is extremely intensive with over 1600 hours of clinical contact time and is carefully structured to deliver well-rounded graduates in a relatively short timeframe.
Special features
The programme aims to:
• Produce highly skilled PA graduates through an integrated programme of medical education designed to meet the current requirements of The National Competence and Curriculum Framework for Physician Associate Education (DOH, 2012) in training safe and effective practitioners who are able to work to the medical model.
• Enable students to develop their knowledge and understanding of relevant principles and practical approaches in the clinical, behavioural and social sciences, including: anatomy, biochemistry, communication sciences, developmental biology, ethics and law, healthcare policy, health education, histology, immunology, pathology, microbiology, physiology, pharmacology and therapeutics, psychology, public health, epidemiology, sexual health, and medical sociology.
• Develop the intellectual skills of students in problem-solving, critical analysis, logical thinking, clinical reasoning and reflection.
• Develop a broad range of patient-centred clinical consultation skills and equip students to recognise the limitations of their scope of professional practice and individual capabilities.
• Develop the professional behaviours necessary to ensure that graduates can provide high standards of medical practice.
• Produce graduates who are well prepared for a career that will include significant amounts of continuous professional development and mandatory revalidation assessments, and
• Develop core skills in verbal, written and electronic communication.
Course collaborators
• Health Education England (HEE)
In addition, we work closely with the following institutions to develop the role of the Physician Associate as part of the North West Consortium for physician associate education:
- The General Medical Council
- The Royal College of Physicians (Faculty of Physician Associates)
- The North West Consortium Universities (UCLan, Chester and Edgehill)
- Physician Associate Schools Council
Facilities
The majority of your academic study will take place within the Stopford Building, Oxford Road in central Manchester. Facilities include: clinical skills laboratories, theatres and seminar rooms.
Extensive library facilities on site directly link to the University of Manchester Network. Each participant will receive access to University of Manchester Library services.
Structure of the Programme
The programme is non-modular and credit bearing (90 credits per academic year). Taught content is delivered in blocks of study of increasing complexity alongside two longitudinal themes of Personal and Professional Development (PPD) and Clinical Consultation Skills (CCS). Each taught block feeds seamlessly into the next and all components of the MSc are compulsory. The programme contains an element of continuous assessment throughout in addition to summative written and Objective Structured Clinical Examinations (OSCEs) at the end of each year.
The first year of the programme begins with a period of intensive study where students develop their understanding of the essential basic and clinical sciences that facilitate safe and effective practice. The curriculum is built around a core of common clinical situations that are then organised according to their relative complexity and biomedical interdependence. The content of each taught block is delivered using a problem based learning (PBL) approach through the study of interactive clinical cases/scenarios (where students actively manage their ‘virtual’ patients). Each case integrates elements of the taught content, so that students learn about and reflect upon the related biomedical, behavioural and population sciences appropriate to the case. PBL is supported by small group teaching, lectures and workshops. This structure is strong from an educational point of view because it enables students to recognise the integrated nature of clinical practice from knowledge and skills relating to basic biological and behavioural sciences, public health, epidemiology, ethics and law, through to clinical teaching and learning, clinical skills development and professionalism.
Formative assessments are provided at at appropriate points in the course and summative assessment takes place at the end of each year. Summative assessment takes the form of an OSCE examination and multiple choice papers (with a clinical reasoning component). The Consultation Skills and PPD components are continuously assessed through a portfolio element and ‘sign off’ system for core clinical/procedural skills and the successful completion of clinical placements.
The programme structure for both years is summarised in the diagrams below:
Year One:
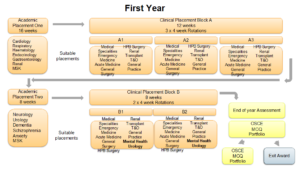
Figure 1: Year 1 Programme Structure.
Year Two:
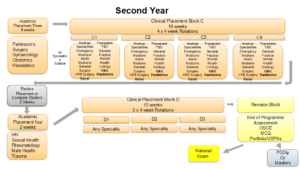
Figure 2: Year Two Programme Structure.
MSc Components
Students registered on the MSc Programme also undertake a 30-credit ‘quality and evidence’ project in the second year of study, supported by a 30-credit preparatory unit in the first year of study that requires you to write a series of reflections and a proposal document.
Preparation for project work runs concurrently with clinical studies in both years of the programme and data collection for the research component (if students are undertaking a relevant project) begins in the final year. The nature of projects offered will reflect research interests of staff, NHS providers and other partner organisations. Students are encouraged to attend relevant seminars and will receive support with academic writing and presentation skills. Progress through each key stage of the project is monitored by the supervisor and Academic Lead for Assessment. Students are offered support by their project supervisor in the form of group tutorials and one-to-one supervision. Assessment of the project will usually be in the format of a report-based dissertation or systematic review (70%) and an oral presentation (30%). Submission in another format (for example, by publication or installation) may be permitted by prior approval by Academic Lead for Assessment.
Students are encouraged to attend relevant seminars and will receive support with academic writing and presentation skills. Progress through each key stage of the project is monitored by the supervisor and Academic Lead for Assessment. Students are offered support by their project supervisor in the form of group tutorials and one-to-one supervision. Submission in another format (for example, by publication or installation) may be permitted by prior approval by Academic Lead for Assessment. Assessment of other units will follow the assessment activities set out in the relevant unit specifications.
- Thesis/Report/Dissertation (Year two) – Candidates produce a written report of the project, audit or systematic review equivalent to 4000 words
- Oral Presentation (Year two) – Candidates deliver an oral presentation based around their project and the related findings/outcomes, equivalent to a 15 minute presentation.
- Reflective Account of Practice (Year one) – Candidates produce a reflective account of practice based on their experiences across the programme describing their development as a clinician, educator and researcher. Candidates will also produce a proposal document. Equivalent to 4000 words
Academic Timetable and Assignment Timeline
Please see resources on Blackboard and those distributed by the Lead Employer for further details.
Course Unit Outlines
The programme is non-modular and consists of a single 60 credit unit studied in each academic year.
Students registered on the MSc Programme also undertake a 30-credit research or ‘quality and evidence’ project in the second year of study, supported by a 30-credit preparatory unit in the first year of study that requires reflection and write-up of existing study.
Please see the programme specification on Blackboard for more detail on the aims and objectives that relate to each year of study.
Personal and Professional Development (PPD)
Successful Physician Associates should be continuously developing their role as a “professional”. You must work with other members of the multidisciplinary team in a way that values and promotes equality, respect diversity and helps provide more effective and integrated services. Working in a high pressured and continuously evolving environments means that Physician Associates must develop resilience, be continuously updating their knowledge and understand how they can work within their own individual competencies.
PPD often raises issues which students find challenging, and you will therefore each have a designated academic advisor who will provide appropriate support and guidance to help with the process of PPD. Additionally workshops will be delivered throughout the programme related to professionalism issues to help develop and challenge your ideas of PPD. You must also attend a mandatory introductory lecture to PPD during your first semester and practical guidelines will be published onto the blackboard system about how to reflect on experiences and develop yourself as a professional.
It is of the utmost importance that all entries published on your Showbie account are completed honestly and with integrity, whilst maintaining anonymity of anyone involved. Students must not plagiarise of fabricate material. Failure to meet these standards will result in disciplinary action and could result in exclusion for the programme
PPD Portfolio
Keeping a PPD portfolio is important in your development as a healthcare professional. As a student you will provide evidence of your development keeping a reflective diary of meaningful encounters. These will be in the format of either a case history, or a reflection. You will be expected to have a minimum of 12 case histories and 12 reflections uploaded onto your showbie PPD Portfolio per each year. Each case history should be linked to an individual presentation (see “case history advice” document on blackboard).You should have at least one reflection linked to one of the seven competencies (see “reflective practice” document on blackboard) each year. The seven competencies are:
- Make the care of your patient your first concern
- Knowledge skills and performance
- Ensures a high level of patient safety and quality of care:
- Communication, partnership and teamwork
- Confidentiality
- Consent
- Maintaining trust
In order to satisfactorily complete the PPD component of the programme you must also be deemed to have undertaken a range of other tasks or activities for progression and completion of the course; these will be described in more detail as the programme progresses but include:
- Completed placement forms (forms signed by your placement supervisors that conform you have attended and completed clinical placements)
- Completed Procedural Skills Assessment (UPSA) forms. A portfolio of UPSA forms which must be completed in order to complete the programme.
PPD Essay
You will submit a summative PPD reflective essay each year. The PPD essay will be on a specific theme
3. Teaching, Learning and Assessment
Teaching and Learning
The programme structure has been designed using established educational theory around a social-constructivist model and practices to enhance student experience and learning.
The University of Manchester virtual learning environment (Blackboard) guides participants through module content, assessment submission and programme information.
The programme structure has been designed using established educational theory around a social-constructivist model and practices to enhance student experience and learning.
The University of Manchester virtual learning environment (Blackboard) guides participants through module content, assessment submission and programme information.
The programme uses blended teaching methods that are aligned with intended learning outcomes and assessment. A range of teaching methods is used including problem-based learning, lectures, online activities, e-learning case work, small group tutorials, workshops, clinical simulation, interactive forums, themed case discussions, clinical debriefs and practical sessions with real and simulated patients.
Students are taught in relatively small groups (between 10 and 35 students per group for most activities and around 65 for lectures) to encourage maximum opportunities for clinical learning.
Examinations and Assessment
Examinations are important for you to find out how you are progressing through the programme and necessary for the programme to make sure that you have reached the required level of competence and are safe to move on to the next stage or to be recommended for professional registration. However, we do not want to make the examinations so complicated and arduous that you spend all your time revising for them rather than concentrating on learning how to be a good PA, or revising only to ‘pass and forget’ the information.
We want examinations that reliably measure your knowledge and ability and are fair in judging whether you should pass. All this has been taken into account in deciding on the examination system for the PA Programme. We have based the assessments on the best evidence available from research.
Responsibility for Assessment
The Programme Committee has overall responsibility for PA Programme examinations and assessments. Members include the Academic Lead for Assessment, Head of the PA Programme, the Academic Leads responsible for each major assessment (End of Year Tests, OSCEs and PPD Portfolio).
Each assessment is the responsibility of this multidisciplinary group, which sets the examination, ensures the quality of the process and evaluates the results.
Assessment for the PA Programme is by a combination of written and practical examinations, taking place (in general) at the end of each year. The examinations are designed to test skills and knowledge that you will have acquired throughout the programme. The programme reserves the right to change any assessment method but will give students full information on such changes.
If you need any advice about examinations, you should contact the Academic Lead for Assessment, Dr Sunil Aggarwal sunil.aggarwal@manchester.ac.uk
Formative versus Summative Assessments
A summative assessment is one that you must pass in order to carry on to the next stage or complete the Programme. Summative assessments are also called ‘high stakes’ assessments for this reason.
A formative assessment is one that gives you feedback on how you are progressing and what you need to work on. We aim for all our summative examinations to have a formative element as well (hence the breakdown of marks in the OSCEs).
Student Identity Card, Calculators and Dictionaries
You must bring your University Student Identity Card to all examinations, including all OSCEs. Failure to do so may result in you not being allowed to sit the examination. No other form of identification will suffice, including hospital identification. You may bring a calculator to examinations but it must not be capable of storing text. You cannot bring a dictionary. Please see University Guidance for further details:
Possession and Use of Mobile Phones/Radio Transmitters/Receivers
There is a strict policy on the possession of electronic equipment, including mobile phones, radio transmitters/receivers (music players, PDAs, mobile phones and pagers) during examinations. No PA student is allowed to have such a device in their possession during examinations. To do so may lead to a charge of trying to cheat. Merely switching the device off is not acceptable. Do not bring any of the above to examinations. The penalty for having such a device during an examination may be a mark of zero.
Examination Information/Timetables/Results
Assessment timetables and results release dates will be published on Blackboard during the academic year. Timetables for examinations are normally released the month before the examination and individual time-slot allocations (e.g., for OSCEs) are provided in the week before the assessment. Most examinations take place in January. Please ensure you check your University email account, Blackboard and announcements daily for updates and further information on assessments and results. Individual results will be sent to your University email account on the results release date.
Sickness/Absence & Examinations
If you are ill, or cannot attend due to significant personal circumstances, on the day of an examination, you must notify the the School immediately on programmesupport.smspgt@manchester.ac.uk
Please see: Mitigating Circumstances and the MB ChB Examinations and Assessments Policy for “Students with a Temporary Injury or Illness That may be Contagious to Others”
PPD Assessment
There are three areas of PPD assessment:
- PPD Essay- Submission of a summative PPD essay in both year 1 and 2
- Completion of case histories and reflections – formative in year 1; summative in year 2.
- Completion of required placement forms and UPSAs
You will be required to submit a summative PPD Essay each year. The deadline for the essay will be in either November or December, and the title of the essay will be released at least eight weeks before the deadline.
Students who fail the first submission of their PPD essay will be required to re-submit. Failure to pass on the second attempt will result in exclusion from the PA Programme.
Each year you should write and upload a minimum of 12 case histories to your electronic portfolio, each linked to an individual patient presentation; and 12 reflections, with each individual competency linked to one reflection. All case histories and reflections should be of a reasonable quality. This is formative for year 1.
Towards the end of year two, students should have a minimum of 24 case histories, each linked to an individual patient presentation; and 24 reflections, with each individual competency linked to two reflection. This is summative, and failure to achieve this by a specified deadline in year 2 (normally during December) to a reasonable quality will result in a fail and re-submission will be required. Failure to achieve these requirements after a re-submission will result in exclusion from the Programme.
Reassessments
The opportunity to re-sit an examination is not a right. Examiners may refuse a student a re-sit opportunity, for example, should a student have failed to meet the minimum work and attendance requirements.
Marks will be capped in line with the degree regulations for all reassessments.
Failure to satisfy the examiners at re-sit normally results in exclusion from the PA Programme.
End of Year Reassessment
Re-sit examinations for Year 1 and Year 2 are normally held in January-February (OSCE and MCQ).
Any student who needs to re-sit an examination is encouraged to make an appointment to see the Academic Lead for Assessment (Dr Sunil Aggarwal) to clarify the reasons for initial failure and to seek study skills support. Help is best sought immediately after the results are published and will be offered for those components of the examination that led to the failure to satisfy the examiners.
PPD Portfolio Reassessment
Students will be required to maintain a satisfactory PPD portfolio throughout the Programme including any reassessment period. Any reassessment of the PPD portfolio must meet the requirements specified for the relevant period of study. Specific requirements for the PPD portfolio are identified separately in the Handbook.
Quality Control
We work very hard to ensure that examinations are fair for everybody. To help us do this, we employ rigorous quality control measures.
Some examples of our quality control are as follows.
Design of Questions
- The MCQ and SBA Exam questions for the End of Year tests are derived from our own database and may be provided in some cases by our course collaborators or from the Physician Associate Schools Council question bank. We are committed to the highest standards of quality assurance and spend a considerable amount of time creating and reviewing new questions each year. Please note that we do not release past papers.
- Following each assessment, the performance of each question is analysed carefully.
- OSCE questions are chosen from question banks. New questions are added every year by teams of trained doctors, health professionals and other academic staff, following detailed guidance.
- We use blueprints to ensure that our assessments appropriately assess the intended learning outcomes of the curriculum.
Review of Questions
- Written assessments and OSCEs are reviewed by a panel of experts to ensure they are fair and appropriate.
- They are also reviewed by external examiners. These are experienced academic staff from other universities. They help to ensure that our examinations are set at the right level and conform to Curriculum Framework standards and guidance (see External Examiners).
Pass Mark
It is very difficult to set examination papers and inevitably some questions will be more difficult than others. We use well-established measures to correct for this and ensure fairness for all students. We use appropriate systems to set the pass mark for individual assessments to ensure that only safe, competent students pass. We follow the same systems used in other medical schools in the UK and around the world.
Marking the Assessments
- All OSCEs are marked using trained and suitably qualified examiners. All new OSCE examiners must undergo specific training before taking part in their first OSCE. Experienced examiners undergo regular refresher training. In addition, a briefing is given to examiners before each OSCE cycle.
- The End of Year MCQ tests are performed electronically in a secure server. For the OSCEs examiners record their marks electronically using iPads. All OSCEs are marked using trained and suitably qualified examiners.
- During the OSCE itself, senior internal and external examiners monitor the performance of examiners to ensure they are following the guidance given and marking fairly and appropriately.
- The End of Year Tests and OSCEs are processed using automated systems. Quality control processes ensure reliability of the data collection and processing.
Reviewing the Assessments
- After each assessment, we perform a detailed statistical analysis. This includes a comparison of the performance of different examiners at different streams to ensure that marking was fair to all groups of students.
- After each OSCE, we ask examiners for feedback about individual questions. External examiners send detailed reports. We also carefully read all letters and emails sent by students. In the light of all these comments, we amend our questions or assessment procedures to ensure we continue to set the highest possible standards.
Assessments Overview
In the examinations, you will be tested on behavioural and social sciences, and biosciences including anatomy, physiology, microbiology, pharmacology, biochemistry, pathology, immunology and genetics. All of these topics that you have studied in PBL cases and in practical classes (e.g. physiology, pharmacology, anatomy and consultation skills) will appear in the examinations.
The assessments are:
- End of Year Tests – knowledge-based examinations consisting of single best answer questions.
- Objective Structured Clinical Examinations (OSCEs) to assess your clinical skills
- PPD Portfolio – which is a summative assessment.
It is your responsibility to make yourself aware of the dates, times and details of examinations.
Examination details will be posted on Blackboard and will be sent to you by individual email to your University of Manchester student email account as an announcement. No member of academic staff, the Programme Office or the University Examinations Office will give any information about examinations over the telephone or by email.
END OF YEAR TEST
The End of Year Test is a multiple choice question paper consisting of approximately 100 questions (Year 1) and 150 questions (Year 2), which requires the selection of a single best answer from five possibilities. Two hours are allowed for the paper in Year 1 and three hours in Year 2. Negative marking is not used; an incorrect answer will simply be awarded a mark of zero. It is therefore in your interest to answer every question on the examination paper. Extensive research demonstrates that students who have engaged with their studies score better than ‘chance’ if they attempt a question even if they do are not 100% sure of the answer.
The paper contains questions which sample the core knowledge that you have acquired during your studies and will be oriented by the ILOs of that year. The Year 2 End of Year test questions will be guided by the ILOs of both years of the programme.
Setting the Pass Mark
It is very difficult to set examination papers and inevitably some questions will be more difficult than others. We use well-established measures to correct for this and ensure fairness for all students.
The pass mark is determined using the Angoff method, which has been used in many universities for more than 30 years. A mark below the pass mark determined using the Angoff method will be classified as unsatisfactory. Angoff standard setting is cross-checked using the Cohen method which may be adopted for any assessment by resolution of the examination board.
OSCE
The OSCEs test your emerging abilities in the skills and applied knowledge that underpin clinical practice. Your skills and knowledge will build throughout the two years, preparing you to successfully perform as a PA at the end of the programme.
What do the OSCEs consist of?
There are 10 stations in Year 1 and 12 in Year 2 OSCEs. They will test your competence in clinical, bioscience, and communication skills and applied knowledge that underpin the execution of these skills. The skills will be taught in practical classes, in consultation and communication sessions whilst the knowledge is drawn from across the years. The overall list of skills appropriate for each year will be published during the semester in which the OSCE takes place. The skills to be tested in the OSCE assessments will be chosen from these lists.
How are the OSCEs graded?
Each station is marked in 3 sections: [1] the sub-domain ratings, [2] your global score and [3] typed free-text feedback from the examiner.
The sub-domain rating scales are selected to match the station content. The sub-domain rating scales are there to provide you with formative feedback. They are also used to calculate the pass mark for each station.
The global rating is the examiner’s expert judgement of your overall performance on the station. The global score is not simply derived by aggregating the domain ratings but instead reflects how skillfully and competently you performed the station overall – it allows examiners to take into account aspects of your performance not captured by the sub-domains, and how you integrated the various components. The global rating is a 5-point scale:
- Clear Fail
- Borderline
- Satisfactory
- Good
- Excellent
Using both the sum of the marks obtained in the sub-domain rating scales and the mark obtained in the global rating the pass mark is calculated by Borderline regression method. You must not fail more than 4 of the stations.
After the OSCEs you will receive feedback, which will include your subdomain score for each station, your pass/fail mark for each station and written feedback where available.
Year 1 Students who fail will re-sit the OSCE in January/February and will progress to Year 2 provided all other components have been completed satisfactorily.
Students will re-sit the Year 2 OSCE at the end of February.
Students who fail their re-sit opportunity are automatically excluded from the Programme unless acceptable mitigating circumstances are submitted for consideration and are approved by the Mitigating Circumstances Panel.
Preparing for each OSCE
As the OSCE assesses skills and attitudes, the best way to prepare is to carry out as much practical work as you can on the wards, in outpatient clinics and in the community. Practise your skills in the following areas:
- taking and presenting histories
- interviewing patients
- performing physical examinations
- performing simple procedures (e.g. recording blood pressure or venepuncture
- explaining procedures or results to patients
- interpreting investigations or results (e.g. radiographs, ECGs).
It is not sufficient just to rehearse in the skills lab; you must obtain as much real clinical experience as possible.
Below is some practical advice that you may find helpful. Please read it carefully before each OSCE:
In the OSCE the stations are structured. For many stations, examiners are given specific questions to ask and have to mark according to specific points. It is important therefore that you:
- read the instructions carefully
- answer any questions that you are asked
- if you don’t understand what is required of you, you should ask the examiner to clarify the question
Each station is marked individually. A poor performance at one of the stations will not have a great impact on your overall mark, but you must not fail more than 4 stations. It is important therefore that you:
- try not to be preoccupied with your performance on an earlier station
- focus only on the station that you are actually doing
The End of Year OSCEs are official summative examinations: examiners are not allowed to give you feedback or comment on your performance in these examinations as this could potentially unsettle you and impair your performance at other stations. Do not therefore:
- ask the examiner for feedback
- feel disappointed when you do not receive feedback
If you finish a station early it does not necessarily mean that you have achieved full marks. For example in a physical examination station, it is possible that the reason you finished early is that you missed out an important part of the examination. Take a few moments to reflect on what you have done – there may be still time to do the part you have missed out.
Try not to pre-empt another station by trying to overhear what is being said by another student. It may be wrong!
If you have any concerns about inappropriate behaviour by an examiner during the examination, e.g. using their mobile phone whilst examining, unacceptable attitude, not paying attention, or if any necessary equipment is missing etc. you must bring this to the attention of the site organiser as soon as the OSCE is completed. Alternatively, please send an email to the Lead for Assessment within 24 hours listing full details. These will be reviewed carefully by the Curriculum Development Committee and action will be taken by the Examination Board if appropriate. We will not take action in response to anonymous comments as this can lead to unfairness.
Postgraduate Taught Degree Regulations for Students
Postgraduate Taught degrees at the University of Manchester are based on the National Framework for Higher Education Qualifications (FHEQ). This framework requires students to achieve credit at masters’ level in order to get an award. For a standard postgraduate taught Masters programme this will normally mean passing 180 credits. A standard postgraduate diploma will normally have 120 credits and a postgraduate certificate 60 credits. The way in which you study these credits will be defined later in the programme handbook and the programme specification.
The University sets standards relating to your performance on every unit but also on your progression through the programme. The programme and course unit specifications will set out the requirements for passing the credit on individual units.
Important Note: The Physician Associate programme is structured differently to many other postgraduate programmes and you will enrol on a single a single 60-credit unit in each year of the course for the PGDip (the element of the course required to gain professional registration). There are also are a number of exemptions from University regulations to meet professional body requirements. This is especially so in the area of assessment where the programme differs significantly. The programme does not permit compensation rules to be applied to any assessment
Please find below the link to the degree regulations:
The following guidance should be read in conjunction with the regulations policy document.
Criteria for Awards
The award of postgraduate degrees is normally based upon credit accumulation using a pass mark of 50%. However, the programme employs a system of standard setting that leads to a variable pass mark for some components, this will mean that the pass mark may be lower or higher than the standard 50% threshold. Guidance on standard setting will be provided separately and the regulations below are provided for information at this stage.
Award Postgraduate Diploma (exit award)
To obtain a Postgraduate Diploma award, students must have accrued 120 credits (as specified by the programme) including any provision made for compensated or referred units. Please note that award of a Postgraduate Diploma in Physician Associate Studies is subject to exemptions from standard degree regulations due to professional body requirements.
Award Postgraduate Certificate (exit award)
To obtain a Postgraduate Certificate (exit award) students must have accrued 60 credits (as specified by the programme) including any provision made for compensated or referred units.
The award of Postgraduate Certificate degree is based upon credit accumulation using a pass mark of 40% for which there is no classification other than pass/fail.
Exit awards are available for students who do not satisfy the criteria for the programme they are registered on or who need to exit the programme early due to unforeseen circumstances.
Turnitin and Plagiarism
Plagiarism and Other Forms of Academic Malpractice
Academic malpractice is any activity - intentional or otherwise - that is likely to undermine the integrity essential to scholarship and research. It includes plagiarism, collusion, fabrication or falsification of results, and anything else that could result in unearned or undeserved credit for those committing it. Academic malpractice can result from a deliberate act of cheating or may be committed unintentionally. Whether intended or not, all incidents of academic malpractice will be treated seriously by the University.
The Faculty of Biology Medicine and Health have designed a learning module to raise your awareness of academic malpractice and how it can occur in general writing during your studies. This resource can be accessed via Blackboard - SMS Introductory Course and must be completed before you submit your first piece of academic writing for assessment.
The University provides workshops and online training via My Learning Essentials
Please refer to the University of Manchester guidance to students on plagiarism and other forms of academic malpractice
The full guidance document can be viewed here: http://documents.manchester.ac.uk/display.aspx?DocID=2870
Academic Malpractice: Procedure for the Handling of Cases can be found at: http://documents.manchester.ac.uk/DocuInfo.aspx?DocID=639
Turnitin
The University uses electronic systems for the purposes of detecting plagiarism and other forms of academic malpractice and for marking. Such systems include TurnitinUK, the plagiarism detection service used by the University.
As part of the formative and/or summative assessment process, you may be asked to submit electronic versions of your work to TurnitinUK and/or other electronic systems used by the University (this requirement may be in addition to a requirement to submit a paper copy of your work). If you are asked to do this, you must do so within the required timescales.
The School also reserves the right to submit work handed in by you for formative or summative assessment to TurnitinUK and/or other electronic systems used by the University.
Please note that when work is submitted to the relevant electronic systems, it may be copied and then stored in a database to allow appropriate checks to be made.
Mitigating Circumstances and Short Extensions to coursework
Short Extensions to coursework
- Short term illness or injury
- Acute stress from personal or financial issues
Mitigating Circumstances
Mitigating circumstances are personal or medical circumstances which are unforeseeable and unpreventable that could have a significant adverse effect on your academic performance. You should only submit a mitigating circumstances application if you consider it serious enough, and the timing critical, to have affected your performance in your assessed work and examinations.
Request for mitigation must be submitted via the online form, in advance of your assessment submission deadline or exam. Requests for mitigation submitted after the assessment or exam (except those requests made as a result of circumstances that have arisen during the course of that assessment period) will not be considered without a credible and compelling explanation as to why the circumstances were not known before the beginning of the assessment period or why you were unable to complete or submit an application prior to the assessment or exam. Please note that not informing the University of circumstances due to personal feelings of embarrassment and pride, or having concerns over the confidential treatment of requests for mitigation, are not considered to be credible and compelling explanations
All mitigating circumstances applications must be supported by independent third party evidence. The type of evidence required will vary according to the nature of the circumstances. Examples of evidence include a doctor or other health professional’s letter, counsellor’s letter, self-certification form signed by your GP or GP’s Medical Practice (for illnesses of 7 days and under only). Please note that it is a University policy that the self-certification form must be signed by a GP; we cannot accept forms which have not been signed by a GP. Please note that if evidence has not been received within 2 weeks of the submission of your form, and you have not contacted them to inform them of any delay, your application will be refused and no further action will be taken.
Any requests for mitigation will be considered confidentially by a mitigating circumstances panel or sub-panel. Where a request for mitigation is supported, a recommendation will be made to the exam board for them to decide on the best course of action for the student.
You are advised to consult the following guidance, which directs you to seek advice and support before and whilst submitting a request for mitigation.
Guidance for students is available on the web: A Basic Guide to Mitigating Circumstances
For further information about the process and acceptable grounds for mitigation see: Mitigating Circumstances Policy & Procedures: http://documents.manchester.ac.uk/DocuInfo.aspx?DocID=4271
Late Submission Penalty (Including Dissertation)
Work submitted after the deadline without prior approval will be subject to a late penalty in accordance with the University Policy on Submission of Work for Summative Assessment on Taught Programmes. The penalty applied is 10% of available marks deducted per day/24 hours (from the time of the original or extended deadline), until the assignment is submitted or no marks remain.
Penalties for late submission relate to 24 hours/calendar days, so include weekends and weekdays, as well as bank holidays and University closure days.
The mark awarded for the piece of work will be reduced by:
10% of the available marks deducted if up to 24 hours (1 day) late
20% of the available marks deducted if up to 48 hours (2 days) late
30% of the available marks deducted if up to 72 hours (3 days) late
40% of the available marks deducted if up to 96 hours (4 days) late
50% of the available marks deducted if up to 120 hours (5 days) late
60% of the available marks deducted if up to 144 hours (6 days) late
70% of the available marks deducted if up to 168 hours (7 days) late
80% of the available marks deducted if up to 192 hours (8 days) late
90% of the available marks deducted if up to 216 hours (9 days) late
100% of the available marks deducted if up to 240 hours (10 days) late
If the assessment is submitted within 10 days of the deadline the assessment should be marked and feedback to the student provided. If this mark before the penalty is applied reaches the appropriate pass mark but the applied penalty results in a fail of the assessment, the student should not be required to resit the assessment as the original mark can be taken as the resit mark. Further information and examples can be found in the Policy and associated Guidance documents.
For work submitted more than 10 days late, it is regarded as a non-submission and need not be marked. In this case a mark of zero will be awarded and normal resit regulations will apply.
The sliding scale should only be applied to first-sit submissions. For all referred (resit) assessment, any late submission will automatically receive a mark of zero.
For further information:
Policy on the Submission of Work for Summative Assessment on Taught Programmes
Assignment Word Count (Including Dissertation)
In accordance with the University Policy on Marking:
Each written assignment has a word limit which you must state at the top of your first page. It is acceptable, without penalty, for you to submit an assignment within a range that is plus 10% of this limit. If you present an assignment with a word count exceeding the specified limit+10%, the assignment will be marked but 1% will be deducted from this mark for every 100 words over the limit given.
For an original word limit that is 1000 words and an assignment that is marked out of 100. If a submission is made that is 1101 words then it exceeded the 10% leeway, and is more than 100 words over the original limit and should receive a 1 mark deduction.
In accordance with accepted academic practice, when submitting any written assignment for summative assessment, the notion of a word count includes the following without exception:
- All titles or headings that form part of the actual text. This does not include the fly page or reference list
- All words that form the actual essay
- All words forming the titles for figures, tables and boxes, are included but this does not include boxes or tables or figures themselves
- All in-text (that is bracketed) references
- All directly quoted material
Certain assessments may require different penalties for word limits to be applied. For example, if part of the requirement for the assessment is conciseness of presentation of facts and arguments. In such cases it may be that no 10% leeway is allowed and penalties applied may be stricter than described above. In such cases the rules for word count limits and the penalties to be applied will be clearly stated in the assessment brief and in the submission details for that assessment.
Fitness to Practise
Where a programme of study requires the student to undertake practical training in a quasi-professional role in relation to patients, clients or service-users or where the qualification provides a direct license to practise, the Faculty of Biology, Medicine and Health has a duty to ensure that the student is fit to practise. In order to protect present or future patients, clients or service users and to comply with the requirements of professional/regulatory bodies, the Faculty of Biology, Medicine and Health has established a procedure for dealing with student-related fitness to practise issues.
Fitness to Practise issues are initially investigated and considered locally within the School (e.g. by a Health and Conduct Committee) and if necessary referred to the Faculty Fitness to Practise Committee.
A student may appeal against the decision of a Fitness to Practise Committee within twenty days of the decision but only on one or more of the following grounds:
a) procedural irregularity;
b) availability of new evidence which could not reasonably have been expected to be presented to the original hearing;
c) the disproportionate nature of the penalty.
The TLSO facilitates the arrangements for Fitness to Practise Appeals Committees. An Appeals Committee has the power to confirm or alter the original decision, and the outcome is confirmed to students in a Completion of Procedures letter. A student may then decide to pursue a complaint with the OIA.
Information on Fitness to Practise related matters can be found at: www.tlso.manchester.ac.uk/appeals-complaints/fitnesstopractise
Academic Appeals, Complaints, Conduct and Discipline
Academic Appeals
- Students have a right of appeal against a final decision of an Examination Board, or a progress committee, or a graduate committee or equivalent body which affects their academic status or progress in the University.
- Students thinking of appealing should first discuss the matter informally with an appropriate member of staff, in order to better understand the reason for the result or decision and to determine whether the matter can be resolved informally by the School prior to making a formal appeal.
- Should you wish to proceed to a formal appeal, this must be submitted within the timeframe outlined in the Academic Appeals Procedure to the Faculty Appeals and Complaints Team, Room 3.21, Simon Building, University of Manchester, M13 9PL (e-mail: FBMHappealsandcomplaints@manchester.ac.uk).
- The Academic Appeals Procedure (Regulation XIX) and associated documents, including the form on which formal appeals should be submitted, can be found at http://www.regulations.manchester.ac.uk/academic/basic-guide-academic-appeals/
Student Complaints
- The University’s Student Complaints Procedure (Regulation XVIII) and associated documents, including a complaints form, can be found at www.regulations.manchester.ac.uk/academic
- The University has separate procedures to address complaints of bullying, harassment, discrimination and/or victimisation - see https://www.reportandsupport.manchester.ac.uk/
- Students thinking of submitting a formal complaint should, in most instances, attempt informal resolution first (see the procedure). Formal complaints should be submitted on the relevant form to Faculty Appeals and Complaints Team, Room 3.21, Simon Building, University of Manchester, M13 9PL (e-mail: FBMHappealsandcomplaints@manchester.ac.uk).
Conduct and Discipline of Students
- General University information on the conduct and discipline of students can be found at https://www.staffnet.manchester.ac.uk/tlso/academic-appeals-complaints-and-misconduct/
- Faculty policies for students on communication and dress code, social networking. and drugs and alcohol can be found at:
- http://documents.manchester.ac.uk/display.aspx?DocID=29038 (Communication and Dress Code)
- http://documents.manchester.ac.uk/display.aspx?DocID=29039 (Drugs and Alcohol)
- http://documents.manchester.ac.uk/display.aspx?DocID=29040 (Social Networking)
- Information on Academic Malpractice and how to avoid it can be found at http://www.regulations.manchester.ac.uk/guidance-to-students-on-plagiarism-and-other-forms-of-academic-malpractice/
- In accordance with the Policy on Submission of Work for Summative Assessment on Taught Programmes, ‘All typed summative assessment, including dissertations, should be submitted online and subjected to plagiarism detection software, where appropriate’.
The University Library has produced online resources to help students in avoiding plagiarism and academic malpractice at:
4. Student Progression
Monitoring Attendance and Wellbeing of Students
The programme director and teaching staff will monitor the work and attendance of students on the programme. This is for your benefit and helps to ensure you are coping with the work. Regular or a pattern of non-attendance and/or engagement will result in you being contacted by the School to meet with your programme director. Following this, further action will be taken if there isn’t a significant improvement in attendance.
For further information see: Regulation XX Monitoring Attendance and Wellbeing of Students
The University offers a range of advice and support to students experiencing problems with attendance. The A-Z of Services can be found on the MyManchester website. Here you can find a information on a wide range of topics such as library services, disability support and careers advice.
You can also speak to your Programme Director and/or Academic Advisor.
What to do if you are absent
In case of illness you should supply a doctor’s certificate or, if the illness is brief, a self-certification. If you are absent for other reasons then you should write a letter to the Programme Director explaining the circumstances. Medical certificates or letters should be given in person or sent to the Programme Administrator. Whatever your reason for being away, tell your supervisor about it and make any necessary arrangements to catch up with work you have missed.
Progression Requirements
To progress to year 2 of the programme, students are required to successfully pass all year 1 summative assessments and have a minimum attendance rate of 90%.
Satisfactory Completion
Satisfactory completion of each year requires satisfactory attendance, participation in the online components of the programme, and completion of the formative and summative assessments.
Transfers to the programme
Transfers to the programme are not normally permitted.
Special Permissions
It is the expectation of the University that postgraduate taught students pursue their studies on a continuous basis for the stipulated duration of their programme. However, it is recognised that students may encounter personal difficulties or situations which may seriously disrupt or delay their studies. In some cases, an interruption/programme extension/change mode of study or an extension towriting up may be the most sensible option.
Should you wish to apply for special permission, in the first instance, please discuss your circumstances with your Programme Director/Academic Advisor/Dissertation Supervisor.
Withdrawal from the Programme
Students who are considering withdrawing from the programme should discuss this in the first instance with the Programme Director.
If arrangements for withdrawal need to be made, this will be handled by the Programme Administrator, who will manage communication with the Fees and Records Departments and other University bodies as appropriate OR Students may liaise directly with the Programme Administrator who will communicate this information directly to the University Student Services Centre.
5. Student Support
Student Support and Guidance
Student support and guidance within the programme
Support and advice is available to all students both formally and informally from the Programme Directors, the Programme Administrator and research project supervisors.
If you have any queries or would like to discuss any issues at all – academic, administrative, technical or personal – please do not hesitate to get in touch. All personal issues will be dealt with confidentially.
If we are unable to help you directly, we can put you in touch with many of the support services that are available to students of the University through our Student Services Centre.
You can approach these services independently, without the involvement of programme staff. Please refer to the Blackboard Space on Student Support and Guidance which is available via https://my.manchester.ac.uk
Disability Advisory and Support Service (DASS)
The University of Manchester welcomes students with a disability or specific learning difficulties. The University has a Disability Advisory and Support Service, who can supply further information and DASS advisors will be pleased to meet you to discuss you needs. DASS will liaise with your School through the Disability Coordinator to make the necessary arrangements for your support during your time in Manchester.
The DASS office can also provide a copy of the University’s Disability Statement, ‘Opportunities for Students with Additional Support Needs at the University of Manchester’ which sets out the policy and provision for students with a disability.
DASS Contact Details:-
Location: 2nd Floor, University Place
Tel (Disability Service) +44 (0)161 275 7512
Tel (Assessment Centre) +44 (0)161 275 0990
Mobile Number (Text only for d/Deaf students) 07899 658 790
Email (Disability Service) dass@manchester.ac.uk
Email (Assessment Centre) assessments@manchester.ac.uk
School Disability Coordinator Contact Details:-
Email: dc.sms@manchester.ac.uk
Religious Observance and Looking after yourself and your patients during Ramadan
Policy on Religious Observance:
- University Policy
- The Faculty of Biology, Medicine and Health has produced guidance for healthcare students on fasting and caring: Fasting and Caring - Looking after yourself and your patients during Ramadan: guidance for health care students.
Student Pastoral Support (SPS) Team Contacts:
The Student Pastoral Support (SPS) teams are responsible for supporting you in your welfare needs throughout your time on the Programme.
The SPS teams – based centrally on the University campus at the Stopford Building and at each Clinical Education Campus – work together to support you across all years and at all sites.
We can help you with: personal, family or health problems; anxiety about your studies; discussion of the responsibilities of being a PA student; and advice regarding Mitigating Circumstances for assessments. We can also ensure that you are linked in appropriately to the broad range of support available within the Programme and wider University.
University SPS Team Contacts
Contact the Central University SPS Team on med.sps@manchester.ac.uk or 0161 275 1452.
6. Student Conduct and Professionalism
The Physician Associate Programme will help you to develop the professional attitudes necessary for your future career in clinical practice. Not only will you need the discipline to organise and regulate your studies for problem-based learning, you also need to recognise that your behaviour at all times – both inside and outside of University and NHS premises – and your treatment of fellow students, academic and non-academic staff and the general public is of paramount importance. During your medical training, the Programme and the GMC will require you to adhere to the principles laid down in the GMC’s Duties of a Doctor, Achieving good medical practice (2016) and Professional behaviour and fitness to practise (2016).
The GMC requires the Programme to pay close attention to the conduct, behaviour and attitude of their students throughout their training, both on and off University and NHS premises. If the conduct, behaviour or attitude of any student is a cause for concern, for example, antisocial or potentially dangerous behaviour, or a pattern of poor attendance, timekeeping and organisation, the Programme has a duty to ensure that appropriate action is taken – both to help the student understand the problem and develop more appropriate and professional behaviours and, importantly, to safeguard patients and colleagues.
The University has the power to exclude a student from the Programme – even if their academic performance is satisfactory – if they feel that the conduct, behaviour and/or attitude of the student is not consistent with the standards required of the profession.
In order to deal with unprofessional attitudes, actions, conduct and behaviour, the Faculty of Biology Medicine and Health has a Fitness to Practise procedure.
The GMC Guidance “Achieving Good Medical Practice” (2016) and “Professional Behaviour and Fitness to Practise” (2016) set out the professional behaviour expected of medical students, key areas of misconduct, the sanctions available for these, and the processes for student fitness to practise arrangements. This guidance is aimed at medical students, medical schools and anyone involved in medical education.
You are expected to adhere to these guidelines.
Please also read the following:
Faculty of Biology, Medicine and Health Fitness to Practise Procedure
Guidance on Ethics Duty of Care and Confidentiality
“Your studies will bring you into contact with patients and members of the public, who can be physically and emotionally vulnerable. Because of this, and the fact that you’ll be joining a trusted profession, which is regulated by the General Medical Council (GMC), we expect you to understand that there is a difference in the standard of behaviour expected of students on Programmes that bring them into contact with patients and the public.
Specifically, your behaviour at all times, both in the clinical environment and outside of your studies, must justify the trust that patients and the public place in your as a future member of the medical profession. We and your medical school will support you in your journey, which includes teaching and assessment on professionalism.”
Page 4 of the GMC’s Achieving good medical practice: guidance for medical students (2016).
The above GMC guidance outlines the standards of professional behaviour expected of medical students.
All health and social care professionals are bound by the guidance and rules of conduct set out by the Department of Health and Social Care (DHSC) and the relevant regulatory or representative body, e.g. the General Medical Council (GMC) for medical students, General Dental Council (GDC), Nursing and Midwifery Council (NMC), Royal Pharmaceutical Society of Great Britain and Pharmaceutical Society of Northern Ireland, the Health and Care Professions Council (HCPC) and the British Psychological Society (BPS). These in turn define the standards for health and social care education in the UK in settings in which a student is interacting with patients, clients or service users.
Professional attitudes and behaviours are both crucial aspects of a career in medicine and you therefore need to develop these appropriately over the course of the Programme in readiness for your foundation training.
Professionalism encompasses a number of positive attributes such as honesty, integrity, politeness, punctuality, good organisation skills, engaging fully with your studies, complying with University regulations, maintaining your own health, communicating effectively and treating others with respect.
Unprofessional behaviour can include: persistent lateness or absence; dishonesty; rudeness; discrimination, failure to meet deadlines, to respond to communication or to attend teaching sessions and meetings; criminal activity; and drug or alcohol abuse.
You should read and regularly review the GMC’s guidance for students in this area: Achieving good medical practice (2016) and Professional behaviour and fitness to practise (2016).
Aspects of professionalism will be addressed throughout the Programme, including during PBL, PPDPortfolio, ECE visits and ward rounds. Opportunities to demonstrate your professionalism will arise as you progress through the Programme.
If you are involved in a significant incident or pattern of unprofessional behaviour, the Programme has a duty to discuss this with you to ensure you understand the professional requirements of the Programme and a career in medicine and to discuss and agree any support the Programme can offer to enable you to improve your behaviour.
A major occurrence of unprofessional behaviour or a failure to improve a pattern of poor behaviour, despite advice, support and warnings, may lead to referral for consideration by the Chair of the School Fitness to Practise Committee, who will decide if you need to attend a meeting of the Committee to discuss the matter in further detail.
By the end of the Physician Associate Programme, you should have acquired, and be able to demonstrate, the attitudes essential to the practice of medicine, including:
- Respect for patients and colleagues that encompasses, without prejudice, diversity of background, opportunity, language, culture and way of life;
- Recognition of patients’ rights, particularly in regard to confidentiality and consent;
- Ability to cope with uncertainty and adapt to change;
- Awareness of the moral and ethical responsibilities involved in patient care;
- Awareness of the need to ensure provision of the highest possible quality of patient care;
- Development of the capacity for self-audit and for participation in the peer-review process.
In addition, the following objectives have attitudinal implications, especially with respect to the provision of care for populations as well as for individuals.
You should:
- Understand the ethical and legal issues relevant to the practice of medicine;
- Understand the principles of disease prevention and health promotion;
- Have self-management and team-working skills;
- Understand the provision of healthcare in the community and hospital, the constraints affecting its delivery and audit processes through which delivery is monitored.
These objectives reflect the requirements of the General Medical Council with regard to Good Medical Practice.
Developing Attitudes
You should:
- Make sure you are familiar with the principles of professional practice as set out in the GMC’s Achieving good medical practice (2016) and Professional behaviour and fitness to practise (2016);
- Discuss any concerns with your educational supervisor. There may be occasions when you feel other professionals are not following the guidelines (sadly, everyone makes mistakes at times). Be sensitive but be prepared to ask about this;
- Be prepared to listen to comments and helpful criticism from anyone who is involved in your clinical supervision. They are there to help you develop appropriate professional attitudes and gently warn if things are going wrong. The report from your supervisor at the end of each placement is expected to include an appraisal of your development in this field.
7. Student Representation and Feedback
A Student Representative is a student leader and works in partnership with the University staff and Students’ Union to represent the views and experiences of student peers.
The programme’s Student Rep is expected to:
- Complete general SU training & specific school or programme training
- Contact your cohort (other students on your course) to introduce yourself & gather feedback
- Work with staff, the SU and other reps to act on feedback and enact change
- Use existing data to suggest improvements to student experience
- Attend regular staff-student meetings to deliver feedback & propose change
- Attend Faculty level feedback meetings (i.e. Faculty Forum)
There is a dedicated team in the Students’ Union available to support reps with each aspect of the role, along with staff contacts in each programme who help to facilitate the staff-student meetings. Further details of training will be provided for reps once elected and information about additional support/activities for student representatives can be found on the Students’ Union website http://manchesterstudentsunion.com/reps .
You can find more information by visiting the SMS PGT Student Support Hub.
Course Unit Evaluations
The quality of teaching on the programme is monitored in part by student feedback. Thus it is very important that you make your views, good and bad, known. At the end of each course unit, and at the end of the programme, you will be asked to complete an anonymous course unit evaluation form. In addition, please let the course unit leader or the programme director know at any time if you feel there is a problem with a particular area of the programme.
8. Programme Management
Programme Management and Committee Structure
Programme Management
The programme is managed and operated in accordance with the policies, principles, regulations and procedures of the University of Manchester.
Programme Directors relate to the School and Faculty Postgraduate Teaching Committees on matters relating to admissions, exams, reviews and approval of new programmes and units, quality assurance etc. and policy issues of broad relevance to the Graduate School.
The Programme Committee will meet each semester and consist of the Programme Director, Programme Administrator, Programme Committee members and the unit co-ordinators.
The remit of the committee will be to:
- Oversee the teaching, assessment and examining arrangements;
- Monitor cohort progression including failure rate, withdrawal rate;
- Evaluate the extent to which the learning outcomes are achieved by students;
- Monitor, maintain and enhance standards of all aspects of the programme;
- Evaluate the effectiveness of the curriculum and of assessment in relation to programme learning outcomes;
- Evaluate the effectiveness and relevance of the teaching and learning methods employed;
- Review and revise the programme in the light of any relevant Quality Assurance Agency (QAA) benchmarks, any other relevant external and/or professional requirements and developing knowledge in the subject area;
- Receive, consider and respond to feedback from students, employers and external examiners;
- Where the need for change is identified, effect the changes quickly and efficiently;
- Produce an annual action plan via annual monitoring;
- Produce reports for periodic review
- Produce relevant information for an Institutional Audit;
- Review programme documentation, e.g., programme handbooks, programme specifications, promotional literature and programme website;
- Ensure suitable and efficient arrangements are in place for recruitment, admission and induction.
Committee Structure
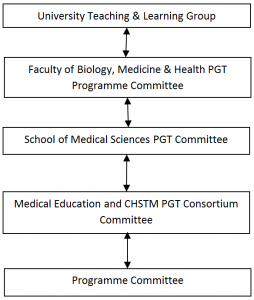
The Programme Committee acts as a curriculum development team for the Programme. The Programme Committee will report to a School, or Department, or Faculty level committee. The Programme Director is responsible for the management of the programme, and the Programme Committee is established to support the Programme Director in the carrying out of their responsibilities.
Programme Committee
The Programme Committee meets every 3-4 months. The committee’s functions and responsibilities are to maintain the standards of teaching, to evaluate and revise the programme in the light of feedback, to monitor student progression and to provide a forum for discussion between the University and the students. The Programme Committee considers feedback from component and ad hoc feedback coordinated by the student representatives. The Programme Committee reviews the annual monitoring report and acts on recommendations arising from the continuous monitoring process.
The membership of the Programme Committee includes: the Programme Director, the Programme Administrator; Academic Lead for Student Support, Welfare and Professionalism, Academic Lead for Assessment, Academic Lead for PPD, teaching staff and student representatives.
External Examiner
External Examiners are individuals from another institution or organisation who monitor the assessment processes of the University to ensure fairness and academic standards. They ensure that assessment and examination procedures have been fairly and properly implemented and that decisions have been made after appropriate deliberation. They also ensure that standards of awards and levels of student performance are at least comparable with those in equivalent higher education institutions.
External Examiners’ reports
External Examiners’ reports relating to this programme will be shared with student representatives at the Staff Student Liaison Committee and/or Programme Committee where details of any actions carried out by the programme team/School in response to the External Examiners’ comments will be discussed. Students should contact their student representatives if they require any further information about External Examiners’ reports or the process for considering them.
External Examiner Details
The External Examiner for this programme is Dr Gillian Conde who is based at the Birmingham Medical School.
You will have the opportunity to meet the external examiner(s) at several points in the programme and they will often observe assessments (e.g. the OSCE). Please note that it is for information only and it is inappropriate for students to make direct contact with External Examiners under any circumstances, in particular with regards to a student’s individual performance in assessments.
Other appropriate mechanisms are available for students, including the University’s appeals or complaints procedures and the UMSU Advice Centre. In cases where a student does contact an External Examiner directly, External Examiners have been requested not to respond to direct queries. Instead, External Examiners should report the matter to their School contact who will then contact the student to remind them of the other methods available for students. If students have any queries concerning this, they should contact their Programme Administrator in the first instance.
9. Learning Resources
Libraries
All registered students may become members of the University of Manchester Library on the main campus.
Up-to-date news about the library is available here.
Information Technology
Students should already be familiar with the basics of using a personal computer, for example using:
- Microsoft Word
- The internet as an aid to study
- Email to communicate
- A web-based search engine to search a clinical database (e.g. PubMed)
Blackboard, the University’s ‘virtual learning environment’, will be used for online teaching. Previous experience in using Blackboard is not necessary, but a willingness to learn new packages is essential.
Students should check their University email account at least daily during the programme. You should always contact us using your University account, we will not normally respond to messages from other accounts during the programme.
Applicants should have regular access to the same PC or Mac on which they are able to adjust the settings, if required, as Blackboard may require you to make minor adjustments to your settings or browser. At the present time, the NHS Trust firewalls will not permit access to some web-based materials. Therefore, applicants must ensure that they have regular access to a suitable computer elsewhere.
Access to a broadband internet connection will significantly improve the download times for web pages, and is necessary for streaming video. It is essential to have a soundcard with a headset or speakers as students will be required to watch and listen to video/audio material.
In addition, students will need the following installed on their computer:
- A suitable internet browser (Internet Explorer, Google Chrome or Mozilla Firefox)
- Microsoft Office or equivalent (e.g. OpenOffice)
- Adobe Acrobat Reader (free download) or Preview for Mac
- Flashplayer (free download)
- Java 2 RTE (free download)
The University of Manchester Library Computer Cluster Area is located on the first, second and third floors, and provides a total of 250 Computers. There are a number of Laserjet printers serving this set-up. One area of the computer clusters is sectioned off for e-mail. Support is available from the Computer Cluster Support Office on the first floor of the library. The cluster is accessible during library opening hours.
IT Services Support Centre online
Details of what IT support is available and how to access it can be found on the FBMH eLearning Support page.
Login to the Support Centre online to log a request, book an appointment for an IT visit, or search the Knowledge Base.
Telephone: +44 (0)161 306 5544 (or extension 65544). Telephone support is available 24 hours a day, seven days a week.
In person: Walk-up help and support is available at the Joule Library, Main Library or Alan Gilbert Learning Commons:
Use Support Centre online for support with eLearning, from where you may make a request, or search the Knowledge Base.
For IT and eLearning support visit:
https://elearning.bmh.manchester.ac.uk/student/technical-support/
Blackboard
Blackboard, the University's 'virtual learning environment', will be used for online teaching.
What is Blackboard?
Blackboard is a web-based system that complements and builds upon traditional learning methods used at The University of Manchester. By using Blackboard you can
- view course materials and learning resources,
- communicate with lectures and other students,
- collaborate in groups,
- get feedback
- submit assignments
- monitoring your own progress at a time and place of your own convenience.
Training in the use of software
The Faculty eLearning team have produced a short introduction to Blackboard for new students. The recording is hosted in two places: the Video Portal and on YouTube:
The recording is just over seven minutes long and covers most of the commonly used tools in Blackboard.
10. Useful Links
Academic Support Policies
A full list of University Policies and documents
Academic Appeals (Regulation XIX)
Academic Malpractice: Procedure for the Handling of Cases
Basic Guide to Student Complaints
Conduct and Discipline of Students (Regulations XVII)
General University information on the Conduct and Discipline of Students
Faculty policies for students on Communication and Dress Code, Social Networking and Drugs & Alcohol
Information on Academic Malpractice and how to avoid it
Data Protection
Guidance for the Presentation of Taught Masters Dissertations
Guidance to Students on Plagiarism and Other Forms of Academic Malpractice
Policy on Submission of Work for Summative Assessment on Taught Programmes
Policy on Mitigating Circumstances
Mitigating Circumstances Guidance for Students
PGT Degree Regulations
Policy on Feedback to Undergraduate and Postgraduate Taught Students
Student Complaints Procedure
Student Charter
Work and Attendance of Students (Regulation XX)
Student Support
A-Z of Student Services
Accommodation
Blackboard via My Manchester
Careers Service
Counselling Service
Disability Advisory and Support Service
University Language Centre – Study English - Tel: 0161 306 3397
Equality, Diversity and Inclusion for Staff and Students
Health & Fitness
Health & Safety Policy
International Advice Team
IT and eLearning Support
Mature Students Guide
Occupational Health Services for Students
Personal Development Planning
A Personal Safety Guide for International Students
Students Union

