BACHELOR OF MIDWIFERY (HONS)/ INTEGRATED MASTERS
Faculty of Biology, Medicine & Health
School of Health Sciences
Division of Nursing, Midwifery and Social Work
STUDENT HANDBOOK
SEPTEMBER 2023
Version: August 2023
Purpose of this Handbook
The Student Handbook has been developed as a resource for undergraduate healthcare students, providing a comprehensive introduction to the Division of Nursing, Midwifery and Social Work and information on all aspects of your programme of study, and should be used as the first point of reference for questions concerning your program, support and advice, or academic policies and procedures. The University of Manchester is a large and complex organisation and we want to ensure that you know how to access the information and support and guidance you need to succeed in your studies. It is therefore designed to guide you through many aspects of your time as a student and provides useful links to information available through the University’s website, as well as summarising the facilities and support services that are available across the University and how you can access them. It also outlines what you should expect of the Division and what they can expect from you, and clarifies the policies and procedures relevant to your area of study. It is your responsibility to familiarise yourself with the Student Handbook and with the contents of the student pages on Blackboard (http://online.manchester.ac.uk) and to use them as a reference when required since they govern important aspects of your programme and therefore may have a significant impact on your studies and the successful completion of your degree.
Note: The material in this handbook can be provided in alternative formats. Please discuss your requirements with your Academic Adviser in the first instance.
Communication
You should note that email is the default means of communication between staff and students. You must use your official University email address when communicating with the University not least because email sent from non-University mail accounts may be classified as SPAM and hence not read.
Information is also provided electronically using Blackboard where student can find detailed information on units and Division specific information.
Teaching staff and students are normally expected to check their email accounts, Blackboard and other electronic methods of communication on a daily basis during term-time and to respond to messages as appropriate.
Disclaimer
Although the information in this Handbook is accurate at the time of publication, aspects of the programme and of Divisional practice may be subject to modification and revision. The Division reserves the right to modify the programme in unforeseen circumstances, or where the process of academic development and feedback from students, quality assurance processes or external sources, such as professional or regulatory bodies, requires a change to be made. In such circumstances, revised information will be issued. Information provided by the Division in the course of the year should therefore be regarded, where appropriate, as superseding the information contained in the Handbook.
Please keep this Handbook in a safe place, as you will need to refer to it throughout your programme.
1. GENERAL INTRODUCTION
WELCOME TO THE DIVISION OF NURSING MIDWIFERY AND SOCIAL WORK

I am delighted to welcome you to the Division of Nursing, Midwifery and Social Work in the School of Health Sciences at the University of Manchester.
As Head of the Division, I am privileged to lead the massively talented teaching, research and professional support staff teams you will be meeting during your time here at the University of Manchester.
We are thrilled that you have chosen the University of Manchester as the destination for your undergraduate student journey on the BMidwif/MMidwif programme. This is a particularly exciting time to be joining the profession.
You are joining a rich and diverse community of scholars – including students training to be nurses, midwives, social workers and psychological wellbeing practitioners as well as those students already qualified in these and other disciplines completing their postgraduate taught and/or research programmes of study. Our education programmes share a common grounding in robust research – much of which has been generated here at the University of Manchester – by the academic staff you will meet while you are here.
We are dedicated to working in partnership with you – placing you and your success at the centre of what we hope will be a transformational learning experience to support you to realise, if not exceed, your individual goals and aspirations.
We know that you will place a premium on high quality teaching and will expect timely and comprehensive feedback on the assessments you submit. We are committed to consistently excellent standards and a growing number of our lecturers have received external recognition for their high standards of teaching. Our approach to assessment is rigorous. Our assessment strategies are regularly reviewed to ensure that they remain relevant, valid and fair. We recognise the importance of providing feedback on assessments that helps you prepare for building on your success in future assignments and ultimately your practice as a midwife.
We challenge you to embrace all of the opportunities that your programme here will offer, to make the most of your time here at the University of Manchester. We want your student journey with us to be intellectually stretching, rewarding but also memorable, enjoyable and fun.
We are hugely proud of the achievements of our many students and alumni who have made a difference to the health and wellbeing of people locally, nationally and internationally. We look forward to celebrating your achievements while you are here at the University of Manchester.
Welcome again and my very best wishes for your successful student journey here at the University of Manchester.
Professor Hilary Mairs
Head of the Division of Nursing Midwifery & Social Work
PROGRAMME DIRECTOR’S WELCOME
Dear Student Midwife,
May I congratulate you on behalf of the Midwifery programme team for gaining a place at The University of Manchester, School of Health Sciences. We are truly pleased that you have chosen our programme and we are looking forward to providing you with the support you need to succeed in gaining both your Bachelor of Midwifery (Hons) or Master of Midwifery degree, and professional registration as a midwife.
The place you have secured here at Manchester was highly sought after and we are pleased to say that we have recruited you because we saw in you the potential to become an excellent midwife and you demonstrated your commitment to a career in Midwifery. Over the next three or four years we will make it our priority to help you to develop your potential to the maximum. Together with our partners in the NHS we will endeavour to ensure that you become a confident and competent member of the midwifery profession. You will also need to take responsibility for your part in this process.
This is an extremely demanding and challenging course that will stretch you academically, practically and emotionally. It is essential that you familiarise yourself with the contents of this handbook so that you can avail yourself of the information that you will need to help you progress through every stage of the course. It will be important to strike the balance between work and play and we can support you to find out what strategies and techniques will be helpful for your continuing success. Whilst we will provide the academic support you need to succeed it is essential that you make use of the wide range of sources of support that are available to you and that are outlined in this handbook. It is also important that you seek and take note of feedback that is designed to help you improve your performance, both with your academic work and as you develop your skills and attributes in practice.
Finally, I would personally like to welcome you to a challenging and wonderful profession. I would also like to invite you to continue the tradition of excellence that The University of Manchester has established by achieving your full potential. I offer you a sincere welcome and wish you well.
Helen White,
Programme Director – Bachelor / Master of Midwifery
CONTACT DETAILS
The Division of Nursing, Midwifery and Social
The University of Manchester
Jean McFarlane Building
Oxford Road
Manchester
M13 9PL
Division Website: Nursing | Biology, Medicine and Health | University of Manchester
|
Head of School Professor Andy Brass Tel: 0161 306 0600 |
Head of Division Professor Hilary Mairs Tel: 0161 306 7779 hilary.j.mairs@manchester.ac.uk |
|
Director of Education Sam Freeman |
Head of Teaching, Learning & Student Experience Chris Bamford Tel: 0161 306 7613 |
Programme Management Team
|
BMidwif (Hons) / MMidwif Programme Director Dr Helen White Tel: 0161 306 7844 |
Lead Midwife for Education Margaret Walsh |
|
|
Admissions Manager Suzanne Eden Tel: 0161 305 2334 |
Admissions Tutors Sue Thornber and Gill Singleton |
|
|
Year 1 Lead Gillian Singleton Gillian.singleton@manchester.ac.uk Tel: 0161 306 7736 |
Year 2 Lead Catherine Anders Catherine.anders@manchester.ac.uk
|
|
|
Year 3 Lead Alice Ciolino Alice.ciolino@manchester.ac.uk
|
Senior Academic Adviser Gillian Singleton Gillian.singleton@manchester.ac.uk Tel: 0161 306 7736 |
|
|
Student Support Manager Saira Jackson saira.jackson@manchester.ac.uk Tel: 0161 275 2559 |
Teaching and Learning Delivery and Development Manager David Parry Tel: 0161 275 2583 |
|
|
Academic Lead for Midwifery Practice Learning Elizabeth Nocton Elizabeth.nocton@manchester.ac.uk Tel: 0161 306 7724 |
Placements Officer Lindsay Blanks Lindsay.H.Blanks@manchester.ac.uk
|
|
|
Academic Lead for Practice Governance Dr Nigel Henderson Nigel.henderson@manchester.ac.uk Tel: 0161 306 78647775 |
||
Programme Support Staff
Programme Support Staff
Programme Support Office (G304)
The Programme Support Office manages day-to-day administration of the programme, including timetabling, room bookings, registration, enrolments and attendance monitoring.
The office is based on the ground floor of the Jean McFarlane Building.
If you have issues relating to your timetables, attendance or seminar groups a member of the team will be able to help you between 9:00-16:00 Mon-Fri or via shs.programmes@manchester.ac.uk
Placements Support Office (G314)
The Placements Support Office manage day-to-day administration of practice learning for your programme.
The office is based on the ground floor of the Jean McFarlane Building.
If you have issues relating to your practice learning a member of the team will be able to help you between 9:00-16:00 Mon-Fri or via shs.placements@manchester.ac.uk
For Topic Specific Enquiries Contact:
- shs.assessments@manchester.ac.uk for examination and assessment queries.
- shs.attendance@manchester.ac.uk for attendance queries.
- shs.mitcircs@manchester.ac.uk for mitigating circumstances queries.
- shs.dc@manchester.ac.uk for disability support.
- shs.placements@manchester.ac.uk for all placement related queries.
- shs.programmes@manchester.ac.uk for programme related queries.
- shs.wellbeing@manchester.ac.uk for wellbeing student support.
- shs.hub@manchester.ac.uk for the student student support hub for general queries and advice not covered by the above teams.
Information, Advice & Guidance Team
The Information, Advice & Guidance (IAG) team are your first point of contact for any non-academic queries you may have relating to your studies, such as what support is available to you, how to access it, and where to direct any queries which you’re not sure about. The IAG team can be contacted via email at shs.hub@manchester.ac.uk, over the phone at 0161 306 7811, or in person at the student hub which is located on the ground floor of the Jean McFarlane building.
WHERE TO GO FOR HELP AND ADVICE
Academic Adviser
Each student is assigned an Academic Advisor at the beginning of their degree. This will be a member of the academic staff in your department who can offer support and advice on academic and pastoral matters, and are key to the School’s student support structure.
You will meet with your Academic Advisor during Welcome Week, and will then have one-to-one meetings throughout the semester to discuss academic progress, steps taken towards career planning, and professional and personal development.
Your Academic Adviser will provide you with support throughout your programme. Our aim is that by engaging with your Academic Adviser, you:
- will know that your adviser cares about your progression, academic success and future plans
- will feel that you belong and are valued regardless of your background, personal strengths and weaknesses
- will know who to contact if you experience difficulties either personally, academically or in placement
- will work to enhance your academic and personal self-efficacy as a result of setting & reviewing goals and reflecting on your experiences
- will gain and grow in confidence and skills in developing professional relationships
- will gain professional support in managing your placement learning and assessment. You will also have an Academic Assessor who will work with your Academic Advisor to support your progress through the practice and academic elements of the programme.
Your Midwifery programme will examine topics that can illicit strong emotional responses from students. If you are affected in any way by the material covered please seek support from your Academic Adviser who may then refer you to other support services.
Unit Lead
The Unit Lead provides detailed unit information including timetabling and assessment guidelines. If you have any queries relating to an individual unit you should speak to the unit leader.
Year Lead
The year lead will be responsible for having an overview of each year of the programme. This involves liaising regularly with the unit leads for that year and supporting them in managing their unit teams. The year lead will ensure consistency of the delivery of unit learning outcomes and ensure that amendments do not lead to curriculum drift, which means when your learning experience does not match with the unit or programme aims. The year lead will also meet regularly with Academic Advisers to ensure there is a strong link between practice and placement.
Programme Director
The Programme Director’s role is to ensure the smooth running of the programme for which he / she is responsible. This involves chairing the Programme Committee, overseeing the student evaluation process, considering changes and improvements to the programme and ensuring adherence to the guidelines set out in the University’s Academic Standards Code of Practice (Teaching Standards Committee of Senate 1998).
Student Support Office (3.335b, Jean McFarlane Building)
The Student Support Office (SSO) can provide you with advice, guidance and signposting regarding any queries or concerns you may have about: your course, placement, finance, disability, accommodation or life at university in general. You can contact the SSO by email (best to email during the pandemic), telephone or by visiting the office on the 3rd floor of Jean McFarlane Building. Open to visitation: 9am – 4pm, Mon – Fri Tel: 0161 306 7725 / 7717. Email: sso.intern@manchester.ac.uk / Sam.Green-1@manchester.ac.uk
SHARING INFORMATION
The University may share appropriate information relating to your health and/or conduct with external organisations such as your professional employer(s) (for example, relevant NHS Trust, Professional and Statutory Regulatory Bodies (PSRB)), placement and training providers and/or regulator such as the Nursing and Midwifery Council (NMC). This may occur where concerns in relation to your health and/or conduct arise and the University considers it necessary for them to be disclosed to one or more of the above organisations. The University’s Privacy Notice for Registered Students (which is accessible via this link: https://documents.manchester.ac.uk/display.aspx?DocID=19049 includes further information about how the University may use and process your personal data, including the legal basis and conditions which may be relevant to such processing (see section 6 of the Privacy Notice). The University will only disclose special category data (such as data relating to your health) to a third party organisation where one of the additional conditions are satisfied (see section 9 of the Privacy Notice), including where processing is necessary for reasons of substantial public interest.
CONTACTING LECTURERS
- Lecturers will let you know how best to contact them at the beginning of each unit or, as Academic Advisers, at the beginning of the programme.
- Any meetings are best made at the beginning or end of the day so that lecturers and students are able to have a break at lunchtime.
- If you want to make an appointment you should do so via email, using your university email address
- In an urgent situation any available lecturer can be accessed for advice and support. It may then be necessary to share this information with the academic adviser / unit leader / examinations officer or programme director as appropriate.
- Five days is recognised as a reasonable time for lecturers to respond to students. Please remember that some staff are part time or have research days, holidays etc. If you require an urgent appointment, please check the location details at the main reception on the ground floor at Jean McFarlane Building.
Contact details of lecturers teaching on your programme are available in Blackboard.
PROGRAMME SCHEDULE & KEY DATES
Term Dates
| Semester 1 | Commences | 18th September 2023 |
| Ends | 28th January 2024 | |
| Semester 2 (part 1) | Commences | 29th January 2024 |
| Ends | 9th June 2024 | |
| Semester 2 (part 2) | Commences | 17th June 2024 |
| Ends | 15th September 2024 | |
| Resit period (resits may also take place at other times) | Commences | TBC |
| Ends | TBC |
Please note that the chart below provides an overview of Year One of the Programme illustrating holidays, study leave and allocation of days to each unit. Unit leaders will provide detailed timetables and assessment guidelines. An overview (A-Z) for your second and third year will be made available on Blackboard nearer the time.
Clinical experience will be gained on weekdays, weekends and as night shifts throughout the programme. The clinical hours expected in each week are made clear below.
PLEASE NOTE THAT HOLIDAYS WILL NOT CHANGE BUT OTHER ASPECTS OF THE TIMETABLE ARE LIABLE TO ALTERATION TO FACILITATE LEARNING.
PLEAE DO NOT BOOK HOLIDAYS DURING STUDY OR PRACTICE WEEKS.
Programme Holidays for Year 1 students
| Christmas | 18th December 2023 – 31st December 2023 |
| Easter break | 1st April 2024 – 14th April 2024 |
| Early summer break | 10-16th June 2024 |
| Flexible Summer breaks | TBC |
Please note that the dates of annual leave for BMidwif/MMidwif students will differ from year to year so you should check the A-Z on Blackboard before confirming any holiday arrangements. In each year there are some opportunities to select from a number of set holidays. Once agreed these programme holidays are non-negotiable. Any breaks taken outside of the programme annual leave dates will be recorded as an absence. Absence may adversely affect your progression and achievement on the programme and may be reported in employment references. If there are clear and compelling reasons why you need to take annual leave at a different time to the published weeks of leave, please discuss this in the first instance with your academic adviser. See also: Programme Attendance Requirements.
It is also important that you make your family and friends aware that your holidays are prearranged and fixed. Please emphasise that they are not to arrange any holidays on your behalf other than at programme holiday times.
Timetable & Course Programme (A-Z) overview
Your Course Programme (A-Z), which shows the teaching pattern for your units across the academic year is available on the Midwifery Gateway on Blackboard. Your detailed timetable is available via MyManchester, by selecting ‘MyCourse’ and ‘Timetable’.
You will be given guidance on accessing your timetable as part of your welcome and induction. If you are concerned that your timetable is incomplete or that you have not been allocated to a seminar group for a unit, you should contact the Programme Support Office for advice.
Please note this overview is correct at the time of publication. Occasionally changes will need to be made due to placement capacity or similar reasons, in which case an updated version will be made available via ‘Midwifery Gateway’ on Blackboard.
| 2023/24 Year 1 (2022 Curriculum) | |||||||||
| W/C | Week No | Mon | Tues | Wed | Thurs | Fri | Sat | Sun | Practice hours (clinical) |
| 12/09/22 | University Welcome Week SEMESTER 1 University Welcome Week | ||||||||
| 18/09/23 | 1 | WW PM | WW PM PASS | WW PM | WW FAP | WW UCP | DO | DO | 0 |
| 25/09/23 | 2 | PM | UCP | PT | FAP | UCP | DO | DO | 0 |
| 02/10/23 | 3 | PM | PT PASS | PT | FAP | UCP | DO | DO | 0 |
| 09/10/23 | 4 | PM/TID | PT | PT | FAP | UCP | DO | DO | 0 |
| 16/10/23 | 5 | PM | FAP PASS | PT | FAP | UCP | DO | DO | 0 |
| 23/10/23 | 6 | PM | FAP | PT | FAP | UCP | DO | DO | 0 |
| 30/10/23 | 7 | PM/AAGp | FAP PASS | PT | FAP | UCP | DO | DO | 0 |
| 06/11/23 | 8 | PM | FAP | PT | FAP | UCP | DO | DO | 0 |
| 13/11/23 | 9 | FAP | UCP PASS | P/DO | P/DO | P/DO | P/DO | P/DO | 21 |
| 20/11/23 | 10 | FAP/AAGp | UCP | P/DO | P/DO | P/DO | P/DO | P/DO | 21 |
| 27/11/23 | 11 | FAP | UCP PASS | P/DO | P/DO | P/DO | P/DO | P/DO | 21 |
| 04/12/23 | 12 | FAP | PM | P/DO | P/DO | P/DO | P/DO | P/DO | 21 |
| 11/12/23 | 13 | PM | PM* | P/DO | P/DO | P/DO | P/DO | P/DO | 21 |
| 18/12/23 | 14 | ANNUAL LEAVE | |||||||
| 25/12/23 | 15 | AL (BH) | AL (BH) | ||||||
| 01/01/24 | 16 | FAP (BH) | UCP | P/DO | P/DO | P/DO | P/DO | P/DO | 21 |
| 08/01/24 | 17 | FAP | UCP PASS | P/DO | P/DO | P/DO | P/DO | P/DO | 21 |
| 15/01/24 | 18 | UCP/AAGp | UCP | FAP | UCP | UCP* | DO | DO | 0 |
| 22/01/24 | 19 | FAP* | FAP/PASS | FAP | FAP* | FAP* | DO | DO | 0 |
| SEMESTER 2 | |||||||||
| 29/01/24 | 20 | UCB | UCB | FMP | FMP/AcAs | UCB | DO | DO | 0 |
| 05/02/24 | 21 | UCB | FMP | P/DO | P/DO | P/DO | P/DO | P/DO | 21 |
| 12/02/24 | 22 | UCB | UCB/PASS | P/DO | P/DO | P/DO | P/DO | P/DO | 21 |
| 19/02/24 | 23 | UCB | FMP | P/DO | P/DO | P/DO | P/DO | P/DO | 21 |
| 26/02/24 | 24 | PM-R | PM-R | P/DO | P/DO | P/DO | P/DO | P/DO | 21 |
| 04/03/24 | 25 | PM-R | FMP/PASS | P/DO | P/DO | P/DO | P/DO | P/DO | 21 |
| 11/03/24 | 26 | PM-R | UCB | P/DO | P/DO | P/DO | P/DO | P/DO | 21 |
| 18/03/24 | 27 | UCB | FMP | P/DO | P/DO | P/DO | P/DO | P/DO | 21 |
| 25/03/24 | 28 | UCB | PT/PASS | P/DO | P/DO | P/DO (BH) | P/DO | P/DO | 21 |
| 01/04/24 | 29 | AL (BH) | ANNUAL LEAVE | ||||||
| 08/04/24 | 30 | ||||||||
| 15/04/24 | 31 | PM-R | FMP | P/DO | P/DO | P/DO | P/DO | P/DO | 21 |
| 22/04/24 | 32 | PM-R | UCB/PASS | P/DO | P/DO | P/DO | P/DO | P/DO | 21 |
| 29/04/24 | 33 | FMP | UCB | P/DO | P/DO | P/DO | P/DO | P/DO | 21 |
| 06/05/24 | 34 | UCB (BH) | UCB/PASS | P/DO | P/DO | P/DO | P/DO | P/DO | 21 |
| 13/05/24 | 35 | FMP | PT – AAGp | FMP | PT* | UCB | DO | DO | 0 |
| 20/05/24 | 36 | UCB | UCB | FMP | FMP | FMP* | DO | DO | 0 |
| 27/05/24 | 37 | UCB (BH) | UCB | UCB | UCB | UCB* | DO | DO | 0 |
| 03/06/24 | 38 | PM-R | R/PM-R | R/PM-R | PM-R* | PM-R* | DO | DO | 0 |
| EXTENDED SEMESTER | |||||||||
| 10/06/24 | 39 | ANNUAL LEAVE | |||||||
| 17/06/24 | 40 | P/DO | P/DO | P/DO | P/DO | P/DO | P/DO | P/DO | 34 |
| 24/06/24 | 41 | P/DO | P/DO | P/DO | P/DO | P/DO | P/DO | P/DO | 34 |
| 01/07/24 | 42 | P/DO | P/DO | P/DO | P/DO | P/DO | P/DO | P/DO | 34 |
| 08/07/24 | 43 | P/DO | P/DO | P/DO | P/DO | P/DO | P/DO | P/DO | 34 |
| 15/07/24 | 44 | P/DO | P/DO | P/DO | P/DO | P/DO | P/DO | P/DO | 34 |
| 22/07/24 | 45 | Pr/DO* | R/PASS | Pr/DO | Pr/DO | Pr/DO | Pr/DO | Pr/DO | 21 |
| 29/07/24 | 46 | ANNUAL LEAVE (flexi) | 0 | ||||||
| 05/08/24 | 47 | ANNUAL LEAVE (flexi) | 0 | ||||||
| 12/08/24 | 48 | P/DO | P/DO | P/DO | P/DO | P/DO | P/DO | P/DO | 34 |
| 19/08/24 | 49 | P/DO | P/DO | P/DO | P/DO | P/DO | P/DO | P/DO | 34 |
| 26/08/24 | 50 | P/DO (BH) | P/DO | P/DO | P/DO | P/DO | P/DO | P/DO | 34 |
| 02/09/24 | 51 | P/DO | P/DO | P/DO | P/DO | P/DO | P/DO | P/DO | 34 |
| 09/09/24 | 52 | Pr/DO | Pr/DO | Pr/DO | Pr/DO | AcAs/R | Pr/DO | Pr/DO | 21 |
| Central Welcome Week | |||||||||
| Local Welcome Week | |||||||||
| Year 1 | |||||||||
| Theory | |||||||||
| PM / PM-R | NURS14100 Professional Midwifery | ||||||||
| FAP | NURS 14111 Foundations of midwifery practice: anatomy and physiology | ||||||||
| UCP | NURS 14121 Universal midwifery care: pregnancy and health promotion | ||||||||
| FMP | NURS14112 Foundations of midwifery practice: microbiology and pharmacology | ||||||||
| UCB | NURS14122 Universal midwifery care: birth, following birth and infant feeding | ||||||||
| PT | NURS14110 Midwifery practice 1 (theory) | ||||||||
| Practice or day off | |||||||||
| Reflective Practice Week (Yr 1 only) | |||||||||
| Holiday | |||||||||
| BH | Bank Holiday | ||||||||
| Examination period | |||||||||
| XXX* | Assessment submission – may relate to another unit | ||||||||
| PA meeting | |||||||||
| AcAs meeting or review | |||||||||
| Flexible holiday period | |||||||||
HEALTH & SAFETY
You MUST familiarise yourself with the procedures for dealing with an emergency, including suspecting or discovery of a fire and fire exit points. Similarly, you are required to familiarise yourself with the Health and Safety at Work regulations, extracts of which are posted outside Room G.319 Jean McFarlane Building. Anyone requiring first aid for themselves or for others should contact one of the first aiders situated in the building. Their names and telephone numbers are posted in common user areas. There are two Health and Safety advisers for the School. Please see University of Manchester Health and Safety Policy for further information.
You MUST complete the Health and Safety induction via the Student Gateway on Blackboard via the Midwifery Gateway. This should be completed during Welcome Week.
The Division and its associated Trusts all have NO SMOKING policies which you must strictly adhere to. The University of Manchester has implemented a total no smoking policy throughout the University campus.
Aspects of the course content may cause distress to some students. If you are affected by any of the issues raised, you can access support from your Academic Adviser who may then refer you to other support services such as the counselling service.
Religious Observance and Looking after yourself and your patients during Ramadan
Policy on Religious Observance:
- University Policy
- The Faculty of Biology, Medicine and Health has produced guidance for healthcare students on fasting and caring: display.aspx (manchester.ac.uk)
ADDITIONAL EXPENSES
It is your personal responsibility to ensure that you have appropriate supplements to your uniform, i.e. black, supportive, soft-soled shoes, scissors, pens, etc.
Whilst the library holds a wide range of texts and journals you will find that your studies are best supported by buying some key texts. Recommendations were sent as pre-course reading.
The cost of travel to the University, to sites and between sites is your responsibility, however, students eligible for The Learning Support Fund can claim back some travel expenses online using the Travel and Dual Expenses (TDAE) link. TDAE is part of the broader Learning Support Fund provided by the NHS Travel and Dual Accommodation Expenses (TDAE).
WHERE TO FIND FURTHER INFORMATION
Blackboard
Blackboard, the University’s ‘virtual learning environment’, is used for online teaching. It is a web-based system that complements and builds upon traditional learning methods used at The University of Manchester. By using Blackboard you can:
- view course materials and learning resources
- communicate with lectures and other students
- collaborate in groups
- get feedback
- submit assignments
- monitor your own progress at a time and place of your own convenience
Training in the use of software: The Faculty eLearning team have produced a short introduction to Blackboard for new students. The recording is hosted in two places: the VLS and on YouTube:
The recording is just over seven minutes long and covers most of the commonly used tools in Blackboard.
Once you have registered you will be able to access Blackboard (https://online.manchester.ac.uk).
Student Services Centre
Burlington Street | Tel: +44(0)161 275 5000 | https://www.studentsupport.manchester.ac.uk/student-services/
The Student Services Centre can offer help and advice about tuition fees assessments or payments, Council Tax, examinations and graduation.
MyManchester
You should familiarise yourself with ‘MyManchester’ (http://online.manchester.ac.uk/) sometimes called your Portal. MyManchester is a way of accessing resources and services, including your personalised timetable, Blackboard, the Library, Student Services, non-academic services, University Email and the Student’s Union.
Noticeboards
Divisional notice boards and electronic screens are located in the Atrium on the ground floor of the Jean McFarlane Building and are used to display a wide variety of information relating to teaching, learning and the student experience, as well as additional student activities such as conferences, internal and external speakers, and wellbeing, charity and other events.
INTRODUCTORY COURSES
All students are automatically enrolled onto an introductory unit that provides information on health and safety, academic malpractice and academic literacy. Completion instructions for each of these sections are clearly defined within the course. Completion of the academic malpractice and health and safety sections is mandatory for all students. All assessments must be completed as soon as possible after the programme begins, with the academic malpractice assessment completed before the first piece of coursework is submitted. Completion of these assessments is monitored by the School. All students are also strongly advised to complete the academic literacy section.
2. TEACHING, LEARNING & ASSESSMENT
You have elected to study on our programme leading to the academic award of Bachelor of Midwifery (Hons) or Integrated Masters Degree. Successful completion of this programme also leads to eligibility for professional registration with the Nursing and Midwifery Council as a midwife.
BMIDWIF OVERALL PROGRAMME AIMS AND INTENDED LEARNING OUTCOMES
The BMidwif programme aims to:
- Develop midwives who demonstrate professional behaviour and attitudes and are skilled; therefore competent, confident, evidence-based, resilient and compassionate practitioners, ready to safely practise within local and national maternity services, with the potential to become professional leaders of the future, and prepared to contribute to global maternity services.
- Enable registration with the Nursing and Midwifery Council (NMC) in accordance with their standards framework for nursing and midwifery education (NMC, 2018), standards for student supervision and assessment (NMC, 2018a), standards for pre-registration midwifery programmes (NMC, 2019), standards of proficiency for midwives (NMC, 2019a) and the International Confederation of Midwives’ definition of the midwife (ICM, 2017).
- Develop midwives who are eligible for the award of a Bachelor’s honours degree from the University of Manchester, in accordance with the purposes of a Manchester Undergraduate Education (UoM, 2021).
The Lead Midwife for Education and the programme team, within the School, Faculty and University, will employ a range of teaching and learning strategies including role modelling good practice that aim to:
- Foster an environment where intellectual curiosity and judgement is valued, by encouraging and developing skills in critical thinking, evaluation, analysis, and synthesis, problem solving, and individual or group research-based learning. Students will be equipped with a strong grounding in academic skills and research theory, enabling them to search for and critically appraise research evidence, analyse findings, identify best-practice, and consider the limits of knowledge and appropriate application in midwifery care.
- Engender a philosophy of respectful, inclusive and compassionate care for all pregnant or birthing women and people, their babies and families; respecting, enabling and advocating for their human rights, needs, safeguarding needs, views, preferences, decisions and strengthening their capabilities. This philosophy acknowledges social and health inequalities and aims to mitigate them through high-quality midwifery care that actively rejects prejudice and discrimination.
- Promote the midwife’s role to practise safely and competently in optimising physiological processes, supporting physical, psychological, social, cultural and spiritual safety to maximise positive outcomes, and anticipate, recognise, mitigate and prepare for complications.
- Cultivate and role model professional values and behaviours, a strong commitment to collaborative working with pregnant and birthing women and people and their families, members of the multidisciplinary team, student peers from other professions, health researchers, maternity service leaders and commissioners. This commitment will nurture students’ leadership capabilities and healthy team-working skills.
- Prepare students upon qualification to be accountable for the evidence-based care of pregnant and birthing women and people, their babies and families throughout the childbearing continuum. This includes being the lead professional where the pregnancy and birth is straightforward, the coordinator of care within the multidisciplinary team when complexities exist, and promoting public health through health education, promotion and protection for all.
- Equip students with the skills to evaluate the quality of maternity care, emphasising the roles of service-user voices, understanding local needs, clinical governance, audit and feedback, and probity and root cause analysis when adverse incidents occur.
- Enable students to acquire, develop and be responsible for maintaining secure knowledge and skills (including communication, clinical, leadership, technical and digital literacy), emotional intelligence and self-care, and a commitment to lifelong learning throughout the programme and their careers. Students will be encouraged to value reflection, self- and peer-evaluation, and peer support as tools to enable this.
- Immerse students in an environment that embraces and values cultural inclusivity, and that is committed to equality of opportunity regardless of race, disability, gender identity, religious or other beliefs, sexual orientation or age; thus, enabling students to qualify as midwives who also embody these values.
- In accordance with the University’s commitment to widening participation in higher education, and in conjunction with service users and providers, recruit to the programme, applicants from diverse backgrounds who demonstrate the academic potential to thrive within the learning environment of the University of Manchester, a strong commitment to providing person-centred maternity services and the potential to become the professional leaders of the future.
- Continually evaluate the effectiveness of the programme in meeting these aims in collaboration with students, service users, health professionals and practice partners.
In order to meet the aims for the BMidwif (Hons), learning outcomes have been mapped across the programme within and across units of learning, and within and across each year of the programme. These learning outcomes are derived from and fully mapped to proficiencies set out in the NMC ‘Standards of proficiency for midwives’ (NMC, 2019), key international midwifery documents and the Manchester Matrix – the purposes of a Manchester Undergraduate Education.
BMIDWIF INTENDED LEARNING OUTCOMES
Knowledge and understanding
On successful completion of the programme graduates from the BMidwif will be able to demonstrate:
A1. Critical contextual understanding of political, ethical, legal, social, cultural, philosophical and evidence-based influences on maternity care, and how this impacts on outcomes for pregnant and birthing women and people and their babies, midwives and the wider workforce, and maternity services.
A2. Applied and effective understanding of the impact of communication and leadership skills, styles and theories on team- and partnership-working with a range of individuals to enable safe and effective care; including coherent knowledge of the roles of other health and social-care professionals and critical evaluation of the contribution of interprofessional collaboration to the provision of high-quality and safe maternity care.
A3. Applied knowledge of relevant life sciences (including anatomy and physiology, genetics and genomics, microbiology, biochemistry, pharmacology, epidemiology, psychology, and sociocultural influences) to underpin midwifery care; systematic understanding and critical analysis of risk factors and complications that put pregnant and birthing women and people and their babies at risk, of strategies for identifying and assessing those risks, and of the appropriate actions to anticipate, mitigate and prepare for complications.
A4. Secure, in-depth knowledge and critical understanding of the role and skills of the midwife throughout the childbearing continuum, including concepts of health, public health, health education and promotion in relation to multicultural local and national contexts, and an awareness of the global context of maternity services.
A5. Systematic comprehension of research methods, and critical evaluation of research findings and evidence-based practice considering the limits of knowledge and appropriate application to midwifery practice.
A6. Applied, in-depth knowledge and critical understanding of the complex factors influencing and influenced by infant feeding practices and a range of strategies to support optimum feeding practices.
A7. Critical understanding and knowledge of strategies for benchmarking, evaluating and improving the safety and quality of maternity care through clinical governance, innovation and research, evaluation of service-user experience, clinical audit, appraising the evidence-base, and professional leadership.
A8. Acknowledgement and application of the variety of educational, teaching and coaching practices that support and underpin learning.
A9. Digital literacy and a coherent understanding of health informatics.
A10. Generation of a personal philosophy of professional and ethical midwifery practice, including the need for ongoing reflective practice and metacognition, self-evaluation and self-care, continual professional development, self-efficacy and autonomy.
Intellectual skills
On successful completion of the programme graduates from the BMidwif will be able to:
B1. Critically analyse, synthesise and evaluate information and evidence from a range of sources related to concepts of midwifery practice, including those outlined above (A1–10), in order to develop a coherent and applied understanding of safe and evidence-based midwifery practice, including strategies for development.
B2. Construct and support reasoned arguments, engage in debate and draw logical conclusions related to their knowledge and understanding as outlined above (A1–10).
B3. Be intellectually prepared to make sound judgements and decisions, both professional and clinical, and to provide a rationale for them.
B4. Plan and conduct a systematic search of the evidence-base, and critically analyse, appraise and synthesise the evidence related to maternity care to propose strategies or priorities for practice development, further education and/or research.
B5. Think critically to solve complex problems related to midwifery care and ethical practice in a range of midwifery care contexts.
B6. Systematically and honestly reflect on and evaluate their own professional practice, learning and experiential needs, and fitness to practice, in order to develop and realise a continuing professional development action plan.
Practical skills
On successful completion of the programme graduates from the BMidwif will be able to:
C1. Practise in accordance with professional, ethical and legal frameworks of midwifery practice ensuring the safety, wellbeing and needs of pregnant and birthing women and people and their families remain their central focus (ICM, 2019; NMC, 2015; WHO, 2019), demonstrating the ability to escalate concerns.
C2. Apply the knowledge and understanding outlined above (A1–10) and the intellectual skills outlined above (B1–6) to underpin autonomous midwifery practice.
C3. Practise midwifery skills safely, competently and effectively, including in emergencies, providing continuity of carer through the childbearing continuum.
C4. Develop respectful and collaborative relationships with pregnant and birthing women and people, empowering, enabling and advocating for them to make informed decisions about their care.
C5. Effectively apply principles and strategies related to public health to promote the health of individuals, families and communities.
C6. Undertake and document systematic, accurate and holistic assessments of the physical, psychological and sociocultural health and wellbeing, safeguarding needs, changing needs and informed decisions of pregnant and birthing women and people, babies, groups and communities in order to formulate, document and realise collaborative and dynamic plans of care.
C7. Demonstrate safe and effective practice in relation to the administration and optimisation of prescription and non-prescription medicines, applying principles of antimicrobial stewardship; and infection prevention and control, including the use of personal protective equipment.
C8. Create and maintain safe environments of care through the effective use of quality assurance and risk management strategies.
C9. Effectively communicate with a range of individuals sensitively taking account of their cognitive, mental, physical, and behavioural health challenges.
C10. Facilitate effective learning with pregnant and birthing women and people, peers and colleagues, including demonstration of skills in supporting, supervising and coaching junior colleagues and peers.
Transferable skills & personal qualities
On successful completion of the programme graduates from the BMidwif will be able to:
D1. Communicate and practise sensitively, safely and with a positive attitude towards meeting the needs of people from diverse backgrounds and cultures, demonstrating the characteristics that pregnant and birthing women and people value, such as kindness and trustworthiness, respecting individuals’ beliefs and cultural practices, being able to challenge discrimination, and escalate concerns, including safeguarding.
D2. Demonstrate excellent professional inter-personal and communication skills (including verbal, non-verbal, written and digital) in a variety of clinical and educational setting with people from all backgrounds.
D3. Work collaboratively with others as part of a team, including those from other professions, recognising and optimising leadership skills in self and others.
D4. Optimise use of study skills, critical thinking, research and enquiry, problem solving and numeracy skills to address academic and clinical questions and facilitate personal and others’ learning.
D5. Demonstrate digital capability, agility and innovation using relevant, contemporary digital and information technologies to optimise practice.
D6. Develop and apply lifelong learning skills based on a drive to enhance and develop their professional performance in the work environment, including reflection, self-evaluation, and recognising and taking appropriate actions if stress or other circumstances are affecting them.
D7. Effectively and appropriately respond to and participate in change management in maternity services.
D8. Develop a sense of their own potential to make a difference to the wellbeing of pregnant and birthing women and people and their families and to the future development
MMIDWIF OVERALL PROGRAMME AIMS AND INTENDED LEARNING OUTCOMES
The MMidwif Programme aims to:
- Develop midwives who demonstrate professional behaviour and attitudes and are skilled; therefore, competent, confident, evidence-based, resilient and compassionate practitioners ready to safely practise within local and national maternity services, as professional leaders of the future, and prepared to contribute to global maternity services.
- Enable registration with the Nursing and Midwifery Council (NMC) in accordance with their standards framework for nursing and midwifery education (NMC, 2018), standards for student supervision and assessment (NMC, 2018a), standards for preregistration midwifery programmes (NMC, 2019), standards of proficiency for midwives (NMC, 2019a) and the International Confederation of Midwives’ definition of the midwife.
- Develop midwives who are eligible for the award of a Master’s honours degree from the University of Manchester, in accordance with the purposes of a Manchester Undergraduate Education (UoM, 2021).
The Lead Midwife for Education and the programme team, within the School, Faculty and University, will employ a range of teaching and learning strategies including role modelling good practice that aim to:
- Foster an environment where intellectual curiosity and judgement is valued, by encouraging and developing skills in critical and original thinking, evaluation, analysis, and synthesis, systematic and creative problem solving, and individual or group researchbased learning. Students will develop a comprehensive understanding of different systematic approaches to evidence synthesis, including searching for and critically appraising research evidence, analysing findings to inform current practice and future research, debate the nature of knowledge and demonstrate originality in the application of knowledge.
- Engender a philosophy of respectful, inclusive and compassionate care for all pregnant or birthing women and people, their babies and families; respecting, enabling and advocating for their human rights, needs, safeguarding needs, views, preferences, decisions and strengthening their capabilities. This philosophy acknowledges social and health inequalities and aims to mitigate them through high-quality midwifery care that actively rejects prejudice and discrimination.
- Promote the midwife’s role to practise safely and competently in optimising physiological processes, supporting physical, psychological, social, cultural and spiritual safety to maximise positive outcomes, and anticipate, recognise, mitigate and prepare for complications.
- Cultivate and role model professional values and behaviours, a strong commitment to collaborative working with pregnant and birthing women and people and their families, members of the multidisciplinary team, student peers from other professions, health researchers, maternity service leaders and commissioners. This commitment will nurture students’ healthy team-working skills, leadership capabilities and potential, personal responsibility, and enable personal and professional development and the development of others.
- Prepare students upon qualification to be accountable for the evidence-based care of pregnant and birthing women and people, their babies and families throughout the childbearing continuum. This includes being the lead professional where the pregnancy and birth is straightforward, acting autonomously in planning and implementing care, and the coordinator of care within the multidisciplinary team when complexities exist, promoting public health through health education, promotion and protection for all.
- Equip students with the skills to critically evaluate the quality of maternity care, emphasising the roles of service-user voices, understanding local needs, clinical governance, audit and feedback, probity and root cause analysis when adverse incidents occur, and to utilise effective leadership skills and theory to contribute to the evidence-based development or co-creation of maternity services.
- Enable students to acquire, develop and be responsible for maintaining secure knowledge and skills (including communication, clinical, leadership, technical and digital literacy), emotional intelligence and self-care, and a commitment to lifelong learning throughout the programme and their careers. Students will be encouraged to value reflection, self- and peer-evaluation, and peer support as tools to enable this.
- Immerse students in an environment that embraces and values cultural inclusivity, and that is committed to equality of opportunity regardless of race, disability, gender identity, religious or other beliefs, sexual orientation or age; thus, enabling students to qualify as midwives who also embody these values.
- In accordance with the University’s commitment to widening participation in higher education, and in conjunction with service users and providers, recruit applicants to the programme from diverse backgrounds who demonstrate the academic potential to thrive within the learning environment of the University of Manchester, a strong commitment to providing person-centred maternity services as the professional leaders of the future.
- Continually evaluate the effectiveness of the programme in meeting these aims in collaboration with students, service users, health professionals and practice partners.
In order to meet the aims for the MMidwif (Hons), learning outcomes have been mapped across the programme within and across units of learning, and within and across each year of the programme. These learning outcomes are derived from and fully mapped to proficiencies set out in the NMC ‘Standards of Proficiency for Midwives’ (NMC, 2019), key international midwifery documents, Health Education England’s ‘Maximising Leadership in the Preregistration healthcare curricula’ (NHS England 2018) and the Manchester Matrix – the purposes of a Manchester Undergraduate Education.
MMIDWIF INTENDED LEARNING OUTCOMES
Knowledge and understanding
On successful completion of the programme graduates from the MMidwif will be able to demonstrate:
A1. Contextual, comprehensive and critical understanding of political, ethical, legal, social, cultural, philosophical and evidence-based influences on maternity care, and how this impacts on outcomes for pregnant and birthing women and people and their babies, midwives and the wider workforce, and maternity services.
A2. Applied, effective and critical understanding of the impact of communication and leadership skills, styles and theories on team- and partnership-working with a range of individuals considering their own leadership skills and using reflection to develop. Including comprehensive knowledge of the roles of other health and social-care professionals and critical evaluation of the contribution of interprofessional collaboration to the provision of high-quality, safe and effective maternity care.
A3. Applied knowledge of relevant life sciences (including anatomy and physiology, genetics and genomics, microbiology, biochemistry, pharmacology, epidemiology, psychology, and sociocultural influences) to underpin midwifery care; systematic understanding and critical analysis of risk factors and complications that put pregnant and birthing women and people and their babies at risk, of strategies for identifying and assessing those risks, and of the appropriate actions to anticipate, mitigate and prepare for complications.
A4. Critical and comprehensive understanding and critical awareness of the psychological and emotional impact of pregnancy, birth, bonding and attachment on maternal, parent and infant mental health, and of strategies that have been developed for identifying, assessing and supporting mental health and parent/infant relationships.
A5. Secure, in-depth knowledge and critical understanding of the role and skills of the midwife throughout the childbearing continuum, including a comprehensive understanding of concepts of health, public health, health education and promotion in relation to multicultural local, national and international contexts.
A6. Systematic comprehension and practical understanding of research methods, in-depth knowledge and skills in identifying and retrieving appropriate evidence, critical interpretation and synthesis of quantitative and qualitative evidence, critical assessment of the quality of evidence using appropriate quality assessment tools and originality in the application of knowledge.
A7. Critical evaluation of the principles and application of health economics and their relevance to resource allocation, considering the impact of maternity policy on the coordination and delivery of maternity services and service development.
A8. Applied, in-depth knowledge and critical understanding of the complex factors influencing and influenced by infant feeding practices and a range of strategies to support optimum feeding practices.
A9. Comprehensive understanding and knowledge of critically appraised strategies for benchmarking, evaluating and improving the safety and quality of maternity care through clinical governance, innovation and translation of research into midwifery practice, evaluation of service-user experience, clinical audit, appraising the evidence-base, and professional leadership and link this to the effective and efficient management of resources.
A10. Acknowledgement and original application of the variety of educational, teaching and coaching practices that support and underpin learning.
A11. Digital literacy and a coherent understanding of health informatics.
A12. Generation of a personal philosophy of professional and ethical midwifery practice, including the need for ongoing reflective practice and metacognition, self-evaluation and self-care, continual professional development and independent learning, self-efficacy and autonomy.
Intellectual skills
On successful completion of the programme graduates from the MMidwif will be able to:
B1. Critically analyse, synthesise and evaluate information and evidence from a range of sources related to concepts of midwifery practice, including those outlined above (A1–12), in order to develop a coherent, applied and original understanding of safe and evidence-based midwifery practice, including current challenges and insights, to generate and strategies for development.
B2. Construct, support and critique reasoned arguments, engage in debate and draw logical conclusions related to their knowledge and understanding as outlined above (A1– 12).
B3. Be intellectually prepared to make sound judgements and decisions, even in the absence of complete data, both professional and clinical, to provide a rationale for them, and communicate them to specialist and non-specialist audiences.
B4. Plan, conduct and critique methods of identifying and retrieving the appropriate evidence, critically appraise research using different study designs to propose original strategies or priorities for practice development, further education and/or research.
B5. Debate critically the nature of evidence and the goal of evidence-based practice.
B6. Think critically, systematically and creatively to solve complex problems related to midwifery care and ethical practice in a range of midwifery care contexts.
B7. Critically understand of the mechanisms that can be used to influence organisational change and public policy, demonstrating development of political awareness and skills.
B8. Systematically and honestly reflect on and evaluate their own professional practice, learning and experiential needs, leadership potential and fitness to practice, in order to develop and realise a professional action plan.
Practical skills
On successful completion of the programme graduates from the MMidwif will be able to:
C1. Practise in accordance with professional, ethical and legal frameworks of midwifery practice ensuring the safety, wellbeing and needs of pregnant and birthing women and people and their families remain their central focus (ICM, 2019; NMC, 2015; WHO, 2019), demonstrating the ability to escalate concerns.
C2. Apply the knowledge and understanding outlined above (A1–12) and the intellectual skills outlined above (B1–8) to underpin autonomous midwifery practice.
C3. Practise midwifery skills safely, competently and effectively, including in emergencies, providing continuity of carer through the childbearing continuum.
C4. Develop respectful and collaborative relationships with pregnant and birthing women and people, empowering, enabling and advocating for them to make informed decisions about their care.
C5. Effectively appraise and apply principles, strategies, and local, national and international guidelines related to public health to promote the health of individuals, families and communities.
C6. Undertake and document systematic, accurate and holistic assessments of the physical, psychological and sociocultural health and wellbeing, safeguarding needs, changing needs and informed decisions of pregnant and birthing women and people, babies, groups and communities in order to formulate, document and realise collaborative and dynamic plans of care.
C7. Demonstrate safe and effective practice in relation to the administration and optimisation of prescription and non-prescription medicines, applying principles of antimicrobial stewardship; and infection prevention and control, including the use of personal protective equipment.
C8. Create and maintain safe environments of care through the effective use of quality assurance and risk management strategies. Identify and analyse developments necessary within maternity services to meet national and local policy directives for maternity service development and change.
C9. Effectively communicate with a range of individuals sensitively taking account of their cognitive, mental, physical, and behavioural health challenges.
C10. Facilitate effective learning using a range of educational practices in an original way with pregnant and birthing women and people, peers and colleagues, including demonstration of skills in supporting and supervising junior colleagues and peers.
C11. Demonstrate critical understanding of systematic review methods.
C12. Adapt and respond appropriately to changing situations of care, demonstrating sound judgement, personal responsibility and initiative in complex and unpredictable professional environments. Show commitment to interprofessional learning and working whilst working autonomously where appropriate.
Transferrable skills & personal qualities
On successful completion of the programme graduates from the MMidwif will be able to:
D1. Communicate and practise sensitively, safely and effectively with a positive attitude towards meeting the needs of people from diverse backgrounds and cultures, demonstrating the characteristics that pregnant and birthing women and people value, such as kindness and trustworthiness, respecting individuals’ beliefs and cultural practices, being able to challenge discrimination, and escalate concerns, including safeguarding.
D2. Demonstrate excellent professional inter-personal and communication skills (including verbal, non-verbal, written and digital) in a variety of clinical and educational setting with people from all backgrounds.
D3. Critically explore and evaluate concepts, processes and skills related to collaborative, collegiate and effective interprofessional team working, recognising and optimising leadership skills in self and others.
D4. Optimise use of independent learning ability, critical thinking, research and enquiry, creative and systematic problem solving and numeracy skills to address academic and clinical questions, facilitate personal learning and that of others.
D5. Utilise systematic and creative approaches to problem solving and decision-making in relation to complex issues demonstrating resilience, empathetic leadership and emotional intelligence when faced with difficult and complex leadership problems and practice issues.
D6. Demonstrate digital capability, agility and innovation using relevant, contemporary digital and information technologies to optimise practice.
D7. Develop and apply lifelong learning skills based on a drive to enhance and develop their professional performance in the work environment, including reflection, self-evaluation, and recognising and taking appropriate actions if stress or other circumstances are affecting them.
D8. Critically reflect on their own academic and practical performance identifying abilities, limitations and opportunities to improve academically and as a practitioner and educator, utilising a range of improvement strategies.
D9. Respond to, initiate and manage change in maternity services effectively and appropriately, based on critical evaluation of current services and the evidence-base.
D10. Develop self-direction and a sense of their own potential to make a difference to the wellbeing of pregnant and birthing women and people and their families and to the future development of midwifery.
PROGRAMME STRUCTURE
This contemporary and innovative full-time midwifery programme offers the opportunity to study for either a Bachelor of Midwifery (Hons) (BMidwif) or an integrated Masters in Midwifery (MMidwif). The length of the BMidwif is 4,600 hours studied over 3 years, in accordance with the Nursing and Midwifery Council (NMC) (2019) regulations. The length of the MMidwif is 5,468 hours studied over 4 years. Based on consultation the BMidwif (which incorporates the first 2 years of the MMidwif) will run over 45 weeks; years 3 and 4 of the MMidwif will each run over 35 weeks. Each week in any year will comprise around 35 hours of study in either theory or practice, or a mixture of both. Successful completion of either award will result in eligibility to register with the NMC as a midwife. In each year of each programme, 50% of learning is theoretical and 50% of learning is based in midwifery and related learning environments (NMC, 2019).
The theory component will be a blend of face-to-face teaching, including teaching of clinical skills in our skills laboratories, online teaching, guided independent and self-directed study. Learning in clinical practice will take place under the supervision of qualified midwives and other health professionals across two placement sites at local NHS Trust maternity clinical learning environment provider sites. Knowledge, attitude, and skills will be assessed using a variety of methods, including written academic assignments, written examinations, viva voce examinations, clinical skills examinations in the skills laboratories and assessment of performance in clinical practice using the national and NMC-validated Midwifery Ongoing Record of Achievement (MORA).
In year 1, the programme commences with a block of approximately 8 weeks of theory learning, prior to starting in midwifery and related learning environments. From this point onwards you will continue to work directly with women/birthing people, newborn infants and their families under the supervision of qualified midwives and other health professionals. The 50:50 integration of theory and practice learning evolves throughout the programme as your experience and confidence develop. In semesters 1 and 2 of year one, theory and practice are integrated within most weeks, in order to provide you with the support you need as you start to gain experience in practice learning environments. Towards the end of year 1 and in years 2 and 3 you will undertake blocks of weeks in practice learning environments, and blocks of theory learning. This hybrid approach to integrating practice and theory learning aims to provide nurturing support at the start of the programme, then transitioning to longer blocks of time to enable you to focus on the programme requirements in each learning setting.
BMidwif (Hons) route:
Semester 1 and semester 2 in each year of study follow normal University semester dates, however each year also has an ‘extended semester 2’ period because of Nursing & Midwifery Council (2009) regulations regarding the length of midwifery programmes (4,600 hours), and the requirements of European Directives (Directive 2005/36/EC).
MMidwif route:
In years 3 and 4 of the MMidwif route, the length of study in each year is shorter and there is not an extended semester 2. Each year is 35 weeks long (1,200 hours of study each).
Units of study
All units of study must be completed for success in the BMidwif (Hons) and MMidwif degrees. There are no optional units although in the last 2 weeks of year 2, students may opt to undertake an unassessed area of study and elective placement related to their future career aspirations. These options include: midwifery professional consolidation, developing a research or education career, and international midwifery practice.
Assessments in semester 1 will be completed by end of the semester in line with the university’s examination cycle. Some units in semester 2 will have assessments completed at the end of semester 2 in line with the university’s examination cycle. Alternative assessment periods will be utilised for units where learning continues into the extended semester period (NMC, 2019), including the practice learning assessment evidenced within the MORA.
There are 15 units of study within the BMidwif programme, and 19 in the MMidwif. All units in the first three years have credit rating in multiples of 10 credits, with the 4th year units in the MMidwif being in multiples of 15 credits. The Midwifery Practice units in each year of the programme combine practice learning assessment (via the MORA) with theory learning assessments. At the University of Manchester, your clinical assessment grade will count towards your final degree classification. The clinical practice assessment accounts for 30 credits in years 1 and 2; and 40 credits in year 3 (both BMidwif and MMidwif) and year 4. It should be noted that all units are compulsory and must be successfully completed in order to obtain both the registered midwife qualification and the academic award.
FHEQ Levels 4 to 6 are studied over the three years of the BMidwif, and Levels 4 to 7 are studied across the 4 years of the MMidwif. Full details of units/credits/learning outcomes are presented later in this handbook. The focus of level 4, first year study is on the foundations of midwifery knowledge and application of this to universal midwifery care. At subsequent levels this knowledge is built upon to allow you to understand and detect more complex scenarios and competency care for those with additional care needs. Throughout the programme you will develop the skills to practice as a professional midwife including in continuity of midwifery carer models; to retrieve, critically appraise and apply research-based evidence; to work collaboratively with others and become leaders of the future. Ultimately the Programme will prepare students for employment as midwives at the point of registration, ensuring they are fit for purpose within the local NHS Trusts.
Teaching and learning strategies have been developed to enable you to have a commitment to life-long learning and equip you with the necessary enquiry, thinking and problem-solving skills to support you in this process. It will also help facilitate the development of midwifery practitioners who are able to reflect on their clinical activities and evaluate their own performance against available evidence.
The programme units are constantly updated to meet the changing needs of women/birthing people and their families, in response to student evaluations and external drivers such as Department of Health directives and NMC requirements.
This programme has been developed through co-creation with a range of stakeholders including current and past students, service users and our practice learning environment partners. The programme is underpinned in structure and philosophy by the most recent NMC Standards for midwifery practice, has been mapped to key national and international midwifery documents and developed following a wide and comprehensive review of current information about the future of the maternity services.
The particular strengths in this programme related to curricular developments are:
- Fully embedding continuity of midwifery carer into practice and theory
- Hybrid approach to integrating theory and practice
- Qualification as a Newborn and Infant Physical Examination practitioner
- Gaining a teaching accreditation with Advance HE as an associate fellow
- The midwife’s important role in public health
- Standards related to the Baby Friendly Initiative
- Research teaching that aligns with our strong Divisional strategy
- Theory learning starting with the foundations of midwifery knowledge incorporating life sciences
- Leadership development, mapped to Health Education England’s model (HEE, 2018)
- Opportunity to explore future career opportunities such as international experience and social enterprise
Content notes: There are occasions in this programme when some sensitive issues and subjects will be covered or discussed that you may find emotionally challenging or feel uncomfortable with. It is important that such issues are addressed within this programme, so that you are prepared to provide high-quality care to individuals who may be affected and to protect yourselves in these situations should they arise in the clinical learning environment. Hence it remains essential that you engage in teaching and learning related to these sensitive issues.
You are encouraged to look at the content of individual units in advance if you think that you might struggle with some of the topics in the course. Topics may include domestic violence, child abuse, termination of pregnancy, mental illness, and racism (this list is not exhaustive as any topic may be distressing depending on individuals’ circumstances). If you feel that you may struggle with the content, you may want to seek support in advance and useful contacts may be your AA or the unit lead.
This programme aims to provide an open space for a critical yet civil exchange of ideas. We ask all learners to help create an atmosphere of mutual sensitivity and respect, just as you will in the clinical learning environment. Please ensure that you are respectful of others and do not use words or share ideas that are offensive or inflammatory. If you disagree with another learner’s ideas, ensure that you discuss their ideas rather than criticising them personally.
If you are concerned about any discussions, please contact the unit lead or the programme director.
INTEGRATED MASTERS IN MIDWIFERY
Students who wish to take the opportunity to qualify with a Masters in Midwifery have the opportunity to study at level 7 in the 4-year integrated Masters programme. To be eligible for the programme you must have achieved an average of a 2:1 (60% and over) throughout your study in years 1 and 2 of the programme. To remain eligible you also need to maintain this level of achievement in year 3.
While years 1 and 2 are exactly the same, irrespective of you electing to study to BMidwif or MMidwif level, year 3 differs. You will undertake fewer theory and practice hours in year 3 of the MMidwif, and the programme runs over 35 weeks. The programme structure, teaching, learning and assessment expectations will also differ on the MMidwif. If you are successful in maintaining the 2:1 average in year 3, you will continue onto study at level 7 in year 4.
If you are unsuccessful in maintaining the 2:1 average in year 3, you will still have the option to qualify with a BMidwif with eligibility to register with the NMC at the end of year 3. This will necessitate making up additional practice and theory hours to meet the NMC Standards (NMC, 2019).
Year 1:
Year 1 lays the foundations for you to develop the knowledge, understanding and skills for competent midwifery practice. ‘Professional Midwifery’ is the basis of a clear thread that runs through the programme enabling you to develop study and research skills, and introduce the concepts of professionalism and ethical practice. You will experience interprofessional education by joining together with learners on the BNurs/MNurs programme for the research thread of this unit. The ‘Foundations’ units support your knowledge of anatomy and physiology, microbiology and pharmacology with which to underpin your understanding of the physiology, and later pathophysiologies, related to childbearing. The ‘Universal Midwifery Care’ units directly reflect Domain 3 of the Standards of Proficiency for Midwives (NMC, 2019), related to the care and support provided to all women/birthing people, their newborn infants and their families. ‘Midwifery Practice 1’ supports you through your first experiences of caring directly for women/birthing people, their newborn infants and their families throughout the childbearing continuum.
| Year 1 – 120 credits at FHEQ Level 4 | ||||
| Semester 1 | Semester 2 | Semester 2 (+) | Credits | Assessment |
| Professional Midwifery | 20 | 1) Information leaflet for learner midwives (1500 words) (50%) (Sem 1) 2) Open book exam (1.5 hours) (50%) (Sem 2) | ||
| Foundations of Midwifery Practice: Anatomy and Physiology | 20 | Online unseen exam, multiple choice (1 hour) and open-book short answer questions (complete within 24 hours) (100%) | ||
| Universal Midwifery Care: Pregnancy and Health Promotion | 10 | Written essay (1500 words) (100%) | ||
| Foundations of Midwifery Practice: Microbiology | 10 | 1) Poster presentation (1000 words) (100%) 2) SafeMedicate drug calculations exam (0%) | ||
| and Pharmacology | ||||
| Universal Midwifery Care: Birth, Following Birth and Infant Feeding | 20 | Written essay: evidence-based care plan (2,500 words) (100%) | ||
| Midwifery Practice 1 | 40 | 1) Clinical proficiencies and MORA assessment (75%)* 2) Structured reflection (1500 words) (25%) | ||
* Practice assessment
Year 2:
Year 2 supports you to build on and develop your knowledge, understanding and skills in order to apply these in more complex scenarios and competently care for those with additional needs. ‘Professional Midwifery: Being Evidence-based’ continues the thread of developing your research skills with direct application to your clinical roles. The ‘Additional Midwifery Care’ units reflect the Domain 4 of the Standards of Proficiency for Midwives (NMC, 2019), and build on the ‘Universal Midwifery Care’ units. The ‘Healthy Teams in Maternity Care’ unit reflects the midwife’s role as part of the multidisciplinary team and in providing an immediate emergency response and first-line management when complications arise. ‘Midwifery Practice 2’ supports you to apply your knowledge of universal and additional care and support, through contribution to the care of all women/birthing people, their newborn infants and families. The Midwifery Practice 2 unit will also enable you to experience clinical practice in another setting through an elective placement, which could be in another Trust in the UK or overseas; and to develop your knowledge, understanding and skills in performing the Newborn and Infant Physical Examination (NIPE).
| Year 2 – 120 credits at FHEQ level 5 | ||||
| Semester 1 | Semester 2 | Semester 2 (+) | Credits | Assessment |
| Professional Midwifery: Being Evidence-based | 20 | Written essay (2500 words): critical appraisal (100%) | ||
| Additional Midwifery Care: Part 1 | 20 | Written essay (2500 words): to include evidence-based care plan (1500 words) with personal development plan (1000 words) (100%) | ||
| Additional Midwifery Care: Part 2 | 20 | Written essay (2500 words): Case study (100%) | ||
| Healthy Teams in Maternity Care | 20 | OSCE and viva (30 minutes) (100%) | ||
| Midwifery Practice 2 | 40 | 1) Clinical proficiencies and MORA assessment (75%)* 2) Critical reflection (1500 words) (25%) 3) Safe Medicate Drugs calculations (0%) | ||
* Practice assessment
Year 3:
Year 3 enables you to consolidate your knowledge, understanding and skills, encouraging you to think strategically about the role of the midwife, as an accountable and autonomous clinician, scholar, leader and educator. ‘Promoting Health for Life’ is the capstone unit for the public health thread, when you utilise your knowledge and understanding to think strategically about the midwife’s role in promoting a healthy life course for families. ‘Professional Midwifery: Scholarly Leadership’ encourages you to apply your research and critical thinking skills to practice-related topics and quality improvement of services. The remaining units in year 3 differ depending on which route you are taking. Those on the BMidwif will take the 30 credit ‘Promoting Excellence in Midwifery’ unit. This unit considers the many different roles of the midwife, including leader, communicator, professional, change-maker and educator. Embedded into this unit is guided preparation for you to apply for the Associate Fellowship of Advance Higher Education (HE) (AFAHE), which forms part of the assessment. ‘Midwifery Practice 3 (BMidwif)’ supports you to apply your consolidated knowledge and understanding, demonstrating proficiency in all areas and your leadership and educator skills. You will also be supported to complete your NIPE qualification. Those on the MMidwif route will take the 10 credit ‘Promoting Excellence in Midwifery Unit’. This unit also considers the many roles of the midwife, in particular as leaders, communicators, professionals and change-makers. Leadership and education form a major aspect of your 4th year studies. ‘Midwifery Practice 3 (MMidwif)’ also supports you to apply your knowledge and understanding by demonstrating proficiency, and to complete the NIPE qualification. You will step-up to the 4th year through a self-directed reflection on your role within a clinical team.
| Year 3 – 120 credits at FHEQ Level 6 | ||||
| Semester 1 | Semester 2 | Semester 2 (+) | Credits | Assessment |
| Promoting Health for Life | 20 | 1) Portfolio (2000 words): Public health strategy (80%) 2) OSCE – Breastfeeding challenges (20%) | ||
| Professional Midwifery: Scholarly Leadership | 30 | Written essay & vlog/blog: Structured literature review (4000 words) and 10 minute vlog (or 1000 word blog) to disseminate information (100%) | ||
| BMidwif: Promoting Excellence in Midwifery | 30 | Patchwork text (4500 words), including AFAHE application | ||
| MMidwif: Promoting Excellence in Midwifery | 10 | Patchwork text (1500 words) | ||
| BMidwif: Midwifery Practice 3 | 40 | 1) Clinical proficiencies and MORA assessment (100%)* 2) NIPE: 20 summative NIPE assessments (0%) 3) Safe Medicate Drugs calculations (0%) | ||
| MMidwif: Midwifery Practice 3 | 60 | 1) Clinical proficiencies and MORA assessment (67%)* 2) NIPE: 20 summative NIPE assessments (0%) | ||
| 3) Written essay: reflective account of continuity of carer experience (2000 words) (33%) 4) Safe Medicate Drugs calculations (0%) | ||||
* Practice Assessment
Year 4:
The principle focus in year 4 is leadership, reflecting the national and local goals to deliver improvements in maternity care through strong, effective midwifery leadership (RCM, 2019). All three theory units in year 4 will share learning with multi-professional learners, which may include post-registration health professionals. ‘Critical Appraisal and Evidence Synthesis’ forms part of the Division’s established Masters in Research and enables you to develop a comprehensive understanding of and skills in critical appraisal and evidence synthesis. These skills are essential to midwifery leadership roles in clinical practice, education, management and research. ‘Leader, Educator, Manager, Co-ordinator’ spans 2 semesters and reflects the enhanced skills learners are expected to apply in clinical practice at level 7. Within this unit you will be supported and guided to apply for the AFAHE accreditation. In ‘Perinatal Parent and Infant Mental Health’ you will critically explore perinatal mental health and the impact on parents, families and infants and strategies and interventions to identify, assess and support. All theory units will enable you to develop the intellectual skills to deal with complex issues in a systematic and creative way, to assist you in making sound judgements which you can communicate clearly to a range of audiences. ‘Midwifery Practice 4’ supports you to apply these skills in clinical encounters, demonstrating self-direction and originality in solving problems. You will further develop your knowledge, understanding and skills in clinical practice to act autonomously in planning and implementing midwifery care, and demonstrate leadership skills to enhance team working and develop others.
| Year 4 – 120 credits at FHEQ level 7 | ||||
| Semester 1 | Semester 2 | Semester 2 (+) | Credits | Assessment |
| Critical Appraisal and Evidence Synthesis | 15 | Online assessment comprising of short answer questions (equivalent 3,500 words) | ||
| Perinatal Parent and Infant Mental Health | 15 | Written essay or poster presentation (3500 words) (100%) | ||
| Leader, Educator, Manager, Co-ordinator | 30 | Patchwork text (4,500 words), including AFAHE application (100%) | ||
| Midwifery Practice 4 | 60 | 1) Clinical proficiencies and MORA assessment (67%)* 2) Critical incident accounts (2,000 words) (33%) | ||
| 3) 10 summative NIPE assessments (0%) 3) Safe Medicate Drugs calculations (0%) | ||||
* Practice Assessment
Further information on all BMidwif/MMidwif units is available via Blackboard and online on the University of Manchester webpages.
UNIVERSITY DEGREE REGULATIONS
The University’s undergraduate degree regulations are available at: Regulations | Academic-related regulations | Undergraduate Degree Regulations | The University of Manchester
The University’s postgraduate degree regulations are available at: Regulations | Academic-related regulations | Postgraduate Degree Regulations | The University of Manchester
PROGRAMME REGULATIONS AND PROFESSIONAL REQUIREMENTS
Introduction
These regulations supplement the degree regulations of The University of Manchester valid at the time of the student’s admission to the University.
The Nursing & Midwifery Council (NMC) dictate that the minimum award for a preregistration midwifery education programme is a Bachelor’s degree in Midwifery (NMC 2019a). There is no option to register for practice with the NMC if the Honours degree level outcomes cannot be achieved.
Programme Specific Regulations
For MMidwif programme, the following weighting will be used to determine the degree classification:
Y1 to Y4 (L4 to L7 FHEQ) using weights of 0.0 (L4), 0.2 (L5), 0.4 (L6) and 0.4 (L7),
For BMidwif (Hons) programme, the following weighting will be used to determine the degree classification:
Y1 to Y3 (L4 to 6 FHEQ) using weights of 0.0 (L4), 0.33 (L5), and 0.67 (L6),
No accreditation of prior learning (APL) is permissible for entry to midwifery degree programmes. The midwifery programme is exempt from the degree regulations pertaining to APL: “Schools can stipulate when APL is not allowed due to Professional Body requirements.” NMC Standards for pre-registration midwifery programmes (2019) section 1.3 states that “recognition of prior learning is not permitted for pre-registration midwifery programmes”.
The NMC Midwifery standards refer to ‘parts’ of the programme, whereby students should complete all elements of one ‘part’ before progressing to another. NMC Standards for Supervision and Assessment of students (2019b) 9.1, 9.4 and NMC Standards Framework for Nursing and Midwifery Education (2019c) 3.8 refer to “9.1 academic assessors collate and confirm student achievement of proficiencies and programme outcomes in the academic environment for each part of the programme” and “progression for each part of the programme”.
Each ‘part’ is an academic year hence students cannot have more than 150 hours of practice learning or any theory or practice learning outcomes outstanding at the end of one part/ academic year of the programme, as this would prevent them progressing to the next part of the programme. Students having less than 150 hours outstanding will be noted at the September Exam Board and be given retrieval opportunities to complete their hours and/or practice / theory learning outcomes prior to a final board in late November/early December. Students who have amassed more than 150 hours of practice learning and / or practice / theory learning outcomes outstanding will be reviewed and may be required to interrupt the programme and recommence at a later date subject to eligibility to resit. The requirement to interrupt is to enable students time to address the issues that are impacting on their ability to keep up with practice hours, and to avoid accrual of any further hours deficit. Following interruption, the agreed return date would take account of the hours deficit to ensure that the student has enough opportunity to complete the required hours within the programme, which may mean a return date in advance of the start of the next year.
A maximum of 40 credits can be carried over into the next year at the discretion of the Examination Board, who will refer to regulation G36 in these considerations.
No compensation is permissible NMC Standards Framework for Nursing and Midwifery Education (2019c) section 5.16 “there is no compensation in assessments across theory and practice learning.”
Reassessment is essential in the final year of the BMidwif (Hons) and the MMidwif in order to satisfy the requirements of the NMC but referred marks will be capped at the pass mark. NMC Standards for pre-registration midwifery programmes (2019a) section 4.3 “ensure throughout the programme that students meet the NMC Standards of proficiency for midwives and programme outcomes”. Referral marks must be capped at 40 for UG and 50 for the master’s year as no compensation is permissible (above).
Reassessment is required in the final year as all components need to be passed.
Exit awards
BMidwif (Hons) with eligibility for Professional Registration with the NMC (for those originally intending the MMidwif but do not continue to L7)
Learners must achieve a minimum of 360 credits, which includes 120 credits at each QAA FHEQ levels 4–6. Professional registration as a midwife is only possible when all theory and practice hours are complete (minimum 4600 hours, 50% theory and 50% practice) and all clinical proficiencies are achieved at the end of the third year, level 6. This will necessitate an additional 166 hours each theory and practice to make up the difference between the MMidwif route and the BMidwif route in year 3. Practice hours and achievement of all clinical proficiencies must be demonstrated and theory hours can be achieved through completion of the extra theory delivered on the BMidwif route, including successful application for Associate Fellowship of Advance Higher Education (AFAHE).
Bachelor of Science Healthcare Studies (maternal and fetal)
This exit award is available to students who do not complete the BMidwif programme and have achieved at least 300 credits, which must include 60 credits at QAA FHEQ level 6. No option for professional registration.
ASSESSMENT
Introduction to Assessment
This section reflects the assessment regulations of the University of Manchester. The standard of the University’s awards and the students’ confidence in the equity and parity of the assessment of their work depends crucially on the scrupulous conduct of all matters relating to the assessment process.
The Bachelor of Midwifery programme and the Master of Midwifery are bound by the degree regulations of the University of Manchester valid at the time of the student’s admission to the University. In addition to these regulations, there is a requirement for additional rules and regulations in relation to midwifery education, as prescribed by the Nursing & Midwifery Council (NMC).
All units of study need to be assessed and in this programme you will be assessed in both theory and practice elements.
The purpose of assessment is to form a judgement on the quality of your work, to ascertain and certify levels of achievement, and to enable examiners’ to report on the standard of performance reached by students.
You will have formative opportunities to undertake that will help you meet the requirements of assessments. Assessments must be passed in order for an award to be conferred. Failure to pass all assessments will affect your progression through the course and may result in discontinuation of your studies.
The pass mark for all assessed work is 40% for years 1-3 and 50% for the integrated master’s year, unless stated otherwise.
The dynamic nature of midwifery education, the variety of assessment strategies, and the changes in University regulations will lead to periodic review of the assessment information within this handbook.
You will be notified of updates through the Blackboard Community Areas – Midwifery Gateway and Practice Learning Gateway. It is important to check this information on a regular basis.
It is essential that you familiarise yourself with these regulations so that you are aware of the correct procedures to follow for all assessment matters.
Systems are in place to support your progression throughout the programme. Please take time to read the rest of this section as it will guide you through relevant processes. If you have a problem or concern at any stage of the assessment process it is beneficial to the student to deal with issues as they arise by contacting their academic adviser in the first instance.
Range of Assessments
A range of assessments are utilised within the programme in order to assess your knowledge, understanding, and developing intellectual, practical and key transferable skills.
There is also a significant amount of practice assessment. In each year you will complete a Midwifery Practice unit that involves clinical placements requiring achievement of practice-based outcomes and competencies, these will be assessed by a Practice Assessor confirming achievement of proficiencies. Your progress will be evidenced in the Midwifery Ongoing Record of Achievement (or MORA) which will be accessed via an online system called PARE (Practice Assessment Record and Evaluation). This is essential to assess your abilities to demonstrate achievement of the knowledge and skills necessary to meet the proficiencies required by the NMC for entry to the professional register. You must demonstrate that you are at the required level in all the unit learning outcomes and the NMC proficiencies in order to pass the practice unit in each part (academic year). You must also pass all theoretical assessments. Both theory and practice assessments contribute to the grade awarded for the unit. Your Academic Assessor will collate and confirm achievement of proficiencies and other programme outcomes at the end of each part (academic year). The Academic Assessor will work in partnership with our Practice Assessor to recommend progression to the next part (academic year) of the programme.
For each assessment, you will be provided with written guidelines to help you formulate your work. For those units incorporating both practical and theoretical assessment elements, both elements of the assessment must be passed in order for you to be awarded credit for the unit.
Preparing for Assessments
Thorough preparation for any form of assessment should enable you to reach your maximum potential.
For each unit of study there is a unit lead and a deputy unit lead who provide much of the teaching for the unit and who work together to provide guidance and feedback opportunities in relation to the unit assessments.
Opportunities for academic support is normally timetabled where you can meet with the unit lead and/or deputy unit lead to discuss issues relating to your assessment work.
Opportunities to gain formative feedback on your work prior to assessment will be provided. This will take a variety of formats. For example the unit leads may provide an opportunity for you to submit up to 500 words of formative work. The purpose of this is to provide feedback on style and level of writing and ability to integrate evidence into your lines of discussion Other formative feedback opportunities may include a seminar where you can present your work to a small group to allow discussion about a case study and your plans for your assignment.
Where the unit assessment is an examination you will have an opportunity to undertake practice questions and discuss answer plans.
There will be plenty opportunities to gain developmental feedback throughout the programme, so you are strongly advised to actively participate in seminars, academic support sessions and/or by completing practice examination questions as appropriate.
Details of appropriate and specific academic support within units are contained within your unit handbooks and on the timetable. Unit leads may provide formative feedback from draft work normally no later than two weeks prior to submission. Should a unit lead be unavailable for any reason you are advised to contact the Deputy Unit Lead in the first instance for guidance.
Should you feel there are any adverse circumstances that may be affecting your ability to engage with your studies you are strongly advised to discuss these with your unit lead, academic adviser, practice supervisor, or practice assessor as appropriate.
MANAGEMENT OF THE ASSESSMENT PROCESS
University and Professional Requirements for Progression
Both the University and the NMC set requirements for progression from one part of the course to the next. NMC progression points exist before the end of each academic year of the programme, and at the end of year 3 (Year 4 for MMidwif) for progression to the register.
Progression
- Progression to the final year (level 7) of the Integrated Masters is dependent upon you achieving an average of at least an upper second classification by the end of the second year in order to register for the Masters (level 7) element of the course.
- If you undertake the MMidwif component and subsequently withdraw, you must complete all outstanding necessary theory and practice learning elements in order to be eligible to register with the NMC with a Bachelors (Hons) degree in order to practice as a midwife.
- You are required to declare, at the beginning of each new year of study and upon return from interruptions, any changes to or that there are no changes to your health and your Disclosure & Barring Service record via a self-declaration.
Guidelines for Assessment Course Work Requirements
Guidelines for written assignments are provided in Unit guides available on Blackboard.
Guidelines for each written assignment are discussed with you before the submission date. If you are seeking further guidance on marked work you should review your feedback and contact the first marker of that work if further clarification is needed.
- You must check each of your unit outlines very carefully to determine the course work requirements for that particular unit. It is strongly recommended that if you do not understand any aspect of an assignment or are otherwise experiencing some related difficulty you should contact the unit leader as soon as possible to discuss the situation. The self-recognition of academic limitations is not a point of failure. All tutors have a function to support students.
- You must make a note of all submission deadlines for course work and make every effort to submit all your course work in on time. Penalties will be applied for failure to meet a submission deadline.
- You need to submit each unit assignment via the online submission process. Alternatively, where online submission is not available another method of submission will be provided.
- All work handed in must be accompanied by the relevant submission details completed by you, including your correct ID number and course unit code (beginning “NURS”).
- If due to illness, mitigating circumstances or other serious personal problems you cannot hand a piece of course work in on time you must complete an extension request form and submit this along with any supporting evidence to the Examinations Office more than 1 day (24 hours) prior to the hand-in deadline date, to request some extra time to complete your course essay. Once agreed you will be emailed an alternative submission date.
- Essays will usually be marked by a lecturer who has contributed to the teaching of the course being assessed, or another member of academic staff with expertise in the area being assessed.
- Moderation should sample all fails, all borderlines (49%, 59%, 69% etc), and a sample (approximately 15%) of the remaining scripts. The total number of scripts moderated should be at least 20% of all submissions.
- You must note that any grade or mark which you receive prior to the Examination Board is provisional, since the Board considers and makes final decisions on academic assessments.
- Essays are the equivalent of examination scripts and as such you should exercise care over your work.
- You must reference your work appropriately using the Harvard referencing system. Further details regarding this method of referencing are included in this For any student who has cited throughout their work but fails to provide a reference list, the assessment will be marked and a 10% reduction will be applied by the marker. The rubric will be used to reflect this mark reduction. A comment will be provided by the marker, in the feedback, noting the lack of a reference list. This change does not replace or impact on the policy pertaining to academic malpractice.
- If you submit an essay which is outside the prescribed word limit you will be penalised by a reduction in the mark awarded. This may result in an essay which would have been considered to be a pass being deemed to be a fail.
Do not write your name on any part of the assignment as the assessment process is supposed to be anonymous. All work submitted online will be given a deadline of 12 noon on the submission date. This is an absolute deadline.
You must gain a receipt for the work to prove that you submitted the work on time and keep the receipt for your records.
Confirm in writing that the work being submitted is you own work that it has not been plagiarised and has not been submitted for any other form of assessment anywhere else.
Word Limits
Each written assignment has a word limit. It is acceptable, without penalty, for you to submit an assignment within a range that is plus or minus 10% of this limit. The rationale for this is to provide a degree of parity for marking and moderating purposes and allow you to demonstrate a degree of academic discipline. It is often more difficult to know what to leave out than it is to know what to put in.
It is not the practice of examiners to count the number of words contained in every assignment. You should clearly state the number of words on the submission cover sheet. This word count should not include the title page, the reference list or any appendices.
If you present an assignment that exceeds the maximum word limit, a penalty of 1% per 100 words above that limit will be imposed.
In accordance with accepted academic practice when you submit any written assignment for summative assessment in the format outlined above the notion of a word count includes the following without exception:
- All titles or headings that form part of the actual text. This does not include the fly page or reference list.
- All words that form the actual essay
- All words forming the titles for figures, tables and boxes, are included but this does not include boxes or tables or figures themselves
- All in-text (that is bracketed) references
- All directly quoted material
Presentation of Assignments
- Presentation is an important aspect of assignment writing. Poor presentation of assignments can result in poor marks. You are strongly advised to take heed of the following guidelines. Further aspects of assignment presentation can be obtained from Academic Advisers, Unit leaders, and the study skills workbook.
- All work handed in must be accompanied by the relevant submission details completed by you, including your correct ID number and course unit code (beginning “NURS”). This should be inserted into the header.
- Each page must be numbered, preferably at the bottom centre position.
- Each assignment must possess a reference list using the Harvard referencing style. For any student who has cited throughout their work but fails to provide a reference list, the assessment will be marked, and a 10% reduction will be applied by the marker. The rubric will be used to reflect this mark reduction. A comment will be provided by the marker, in the feedback, noting the lack of a reference list. This change does not replace or impact on the policy pertaining to academic malpractice.
- Assignments should not be decorated. This is unacceptable in academic work.
- The specific requirements for assessments can be found in the individual unit guide.
Referencing – The Harvard System
Accurate referencing of all written work is essential as it enables readers to (i) assess the accuracy of the writer’s interpretation of source material; (ii) check the writer’s integrity; and (iii) easily seek out material that may be of interest to their own studies. All assignments completed for this programme of study are required to have a reference list.
Though there are many referencing/bibliographical systems around, the Harvard system is the system adopted by many of the prestigious social work and social science journals. More importantly, it is the system, which the Division of Nursing, Midwifery & Social Work has adopted.
This means that it is the only system, which is acceptable for any work submitted by students within the Division. Please see the Library’s Referencing Guide.
ACADEMIC MALPRACTICE: PLAGIARISM, COLLUSION, FABRICATION/FALSIFICATION
As a student, you are expected to cooperate in the learning process throughout your programme of study by completing assignments of various kinds that are the product of your own study or research. For most students this does not present a problem, but occasionally, whether unwittingly or otherwise, a student may commit what is known as plagiarism or some other form of academic malpractice when carrying out an assignment. This may come about because students have been used to different conventions in their prior educational experience or through general ignorance of what is expected of them.
This guidance is designed to help you understand what we regard as academic malpractice and hence to help you to avoid committing it. You should read it carefully, because academic malpractice is regarded as a serious offence and students found to have committed it will be penalised.
Academic malpractice is any activity – intentional or otherwise – that is likely to undermine the integrity essential to scholarship and research. Academic malpractice includes plagiarism, collusion, fabrication or falsification of results and anything else intended by those committing it to achieve credit that they do not properly deserve. In addition to the advice that follows, your Division will give you advice on how to avoid academic malpractice in the context of your discipline. It will also design assessments so as to help you avoid the temptation to commit academic malpractice. Finally, you should take note that work you submit may be screened electronically to check against other material on the web and in other submitted work.
Information on Academic Malpractice and how to avoid it can be found: click here
The University Library has produced online resources to help students in avoiding plagiarism and academic malpractice: click here
Plagiarism
Plagiarism is presenting the ideas, work or words of other people without proper, clear and unambiguous acknowledgement. It also includes self-plagiarism (which occurs where, for example, you submit work that you have presented for assessment on a previous occasion), and the submission of material from essay banks (even if the authors of such material appear to be giving you permission to use it in this way). Obviously, the most blatant example of plagiarism would be to copy another student’s work. Hence it is essential to make clear in your assignments the distinction between:
- the ideas and work of other people that you may have quite legitimately exploited and developed, and
- the ideas or material that you have personally contributed.
To assist you, here is the library’s e–learning essentials guide.
Collusion
Collusion occurs when a student or students collaborate with another student or students, as an individual or group to gain a mark or grade to which they are not entitled. Students who allow another student to copy their work or who make their work available to another student are also committing collusion and both the copier and the provider of the work are liable to be penalised.
Fabrication / Falsification
Fabrication or falsification of data or results by individual students or groups of students is the presentation or inclusion in a piece of work of figures or data which have been made up or altered and which have no basis in verifiable sources; this may or may not involve other instances of academic malpractice.
If you commit any form of academic malpractice, teaching staff will not be able to assess your individual abilities objectively or accurately. Any short-term gain you might have hoped to achieve will be cancelled out by the loss of proper feedback you might have received, and in the long run such behaviour is likely to damage your overall intellectual development, to say nothing of your self-esteem. You are the one who loses.
TurnitinUK
The University uses electronic systems for the purposes of detecting plagiarism and other forms of academic malpractice and for marking. Such systems include TurnitinUK, the plagiarism detection service used by the University.
As part of the formative and/or summative assessment process, you may be asked to submit electronic versions of your work to TurnitinUK and/or other electronic systems used by the University (this requirement may be in addition to a requirement to submit a paper copy of your work). If you are asked to do this, you must do so within the required timescales.
The School also reserves the right to submit work handed in by you for formative or summative assessment to TurnitinUK and/or other electronic systems used by the University.
Please note that when work is submitted to the relevant electronic systems, it may be copied and then stored in a database to allow appropriate checks to be made.
The use of Artificial Intelligence (AI)
We urge students to be cautious when using a chatbot or AI tool within their learning. Chatbots and AI tools can be useful, but there are a number of risks associated with using them. Please ensure that you are aware of what is permissible use of AI for each assignment. You can utilise AI to generate ideas, key themes, and plan your assessment but not to write your assessment. Do not use AI to generate text, or partial text for use in your assessment unless the assignment brief explicitly states that this is permitted, otherwise use will be deemed academic malpractice. This is academic malpractice because the words and ideas generated are not your own and not an accurate reflection of your learning. Further to this, the words and ideas generated by the chatbot or AI tool may make use of other, human authors’ ideas without referencing them, which is plagiarism. Where a chatbot or other form of AI has been used, make sure you acknowledge that use. Information on how to cite can be found here: https://manchester-uk.libanswers.com/teaching-and-learning/faq/264824 Some units, for example those on AI and technology, permit the use of AI. However, they require you to sign a code of conduct which must be adhered to. Make sure you understand and follow these codes. If you are unclear on what is permissible, speak to the unit lead.
ASSESSMENT PROCESS
How to Submit Assessed Work
All assignment texts must be submitted by 12.00pm on the date specified unless stated. All essays must be submitted online via Blackboard. When submitting your assignment online, this must include your reference list as part of the same document. For any student who has cited throughout their work but fails to provide a reference list, the assessment will be marked and a 10% reduction will be applied by the marker. The rubric will be used to reflect this mark reduction. A comment will be provided by the marker, in the feedback, noting the lack of a reference list. This change does not replace or impact on the policy pertaining to academic malpractice.
All work submitted online will produce an e-receipt which should then be filed kept for your records. This receipt is proof that the submitted assignment has been received by the examinations office. Failure to produce an e-receipt when questioning whether a submission has been uploaded will result in a non-submission and a mark of 0% being awarded. It is your responsibility to ensure that you have read and understand the online submission guidelines prior to submission. Regardless of whether you submit work in person, via post or online you must obtain a receipt that verifies on what date the essay was submitted. Unless an extension has been formally granted work must be submitted on or before the published submission date. If a receipt is not generated for an on-line submission, you should try again to upload your work or immediately contact the examinations office for advice if the submission deadline is very close.
The submission of work online will be supported by the examinations office up until the deadline for a submission has passed. You are therefore encouraged to plan ahead and not leave the submission of work online to the last minute.
Once an assignment has been submitted it may need to be retained by the department for quality assessment purposes. Therefore, you must keep a copy of each assignment before submission to the department.
Location of Examinations Office
The Examinations Secretary is located in the Division of Nursing, Midwifery & Social Work exams office, Jean McFarlane Building, University Place. In recognizing ‘normal office hours’ (Mon-Fri 9.00am-4.00pm) you should take account of the normal breaks which occur during the working day in the morning and afternoon and at lunchtime. During the COVID19 pandemic the staff may be working remotely and so the office may not be staffed. You should contact examination office staff by email in the first instance: shs.assessments@manchester.ac.uk.
Submission Dates
See the examinations folder on the Blackboard Midwifery Gateway Community Area. Please note that examination dates are determined by the Central University Examinations team and will fall within the period specified on the assessments schedule unless stated. For information on late submission due to illness or other reasons please refer to the Mitigating Circumstances section of this document.
Late Submission Penalty (Including Dissertation)
Work submitted after the deadline without prior approval will be subject to a late penalty in accordance with the University Policy on Submission of Work for Summative Assessment on Taught Programmes. The penalty applied is 10% of available marks deducted per day/24 hours (from the time of the original or extended deadline), until the assignment is submitted or no marks remain.
Penalties for late submission relate to 24 hours/calendar days, so include weekends and weekdays, as well as bank holidays and University closure days.
The mark awarded for the piece of work will be reduced by:
10% of the available marks deducted if up to 24 hours (1 day) late
20% of the available marks deducted if up to 48 hours (2 days) late
30% of the available marks deducted if up to 72 hours (3 days) late
40% of the available marks deducted if up to 96 hours (4 days) late
50% of the available marks deducted if up to 120 hours (5 days) late
60% of the available marks deducted if up to 144 hours (6 days) late
70% of the available marks deducted if up to 168 hours (7 days) late
80% of the available marks deducted if up to 192 hours (8 days) late
90% of the available marks deducted if up to 216 hours (9 days) late
100% of the available marks deducted if up to 240 hours (10 days) late
If the assessment is submitted within 10 calendar days of the deadline, the assessment should be marked and feedback to the student provided. If this mark before the penalty is applied reaches the appropriate pass mark but the applied penalty results in a fail of the assessment, the student should not be required to resit the assessment as the original mark can be taken in lieu of a resit/referral and normal resit/referral procedures will apply. Further information and examples can be found in the Policy and associated Guidance documents below.
For work submitted more than 10 days late, it is regarded as a non-submission and need not be marked. In this case, a mark of zero will be awarded and normal resit procedures will apply.
The sliding scale should only be applied to first-sit submissions. For all referred (resit) assessment, any late submission will automatically receive a mark of zero.
For further information:
Policy on the Submission of Work for Summative Assessment on Taught Programmes
Assignment Word Count (including the dissertation)
In accordance with the University Policy on Marking, Schools must have procedures in place to apply a penalty if the word count exceeds the limit by more than 10%.
Each written assignment has a word limit, which you must state at the top of your first page. It is acceptable, without penalty, for you to submit an assignment within a range that is plus 10% of this limit. If you present an assignment with a word count exceeding the specified limit +10%, the assignment will be marked but 1% will be deducted from this mark for every 100 words over the limit given.
For an original word limit that is 1000 words and an assignment that is marked out of 100: If a submission is made that is 1101 words then it exceeds the 10% leeway, and is more than 100 words over the original limit and should receive a 1 mark deduction.
In accordance with accepted academic practice, when submitting any written assignment for summative assessment, the notion of a word count includes the following without exception:
· All titles or headings that form part of the actual text. This does not include the fly page or reference list.
· All words that form the actual essay.
· All words forming the titles for figures, tables and boxes, are included but this does not include boxes or tables or figures themselves.
· All in-text (that is bracketed) references.
· All directly quoted material.
Certain assessments may require different penalties for word limits to be applied. For example, if part of the requirement for the assessment is conciseness of presentation of facts and arguments. In such cases it may be that no 10% leeway is allowed and penalties applied may be stricter than described above. In such cases the rules for word count limits and the penalties to be applied will be clearly stated in the assessment brief and in the submission details for that assessment.
EXTENSIONS AND MITIGATING CIRCUMSTANCES
Extensions
If you experience difficulties that will prevent you from submitting assessed coursework on time, you can request an extension of up to one week. You need to provide a credible reason for your extension, in line with the extension policy, but you do not need to submit evidence to support your request.
Please think carefully about whether one-week is enough time to submit and how this will impact the rest of your workload before requesting an extension.
To apply for an extension, you will need to complete this form:
https://www.qualtrics.manchester.ac.uk/jfe/form/SV_56LcBQhsaZ6Agsu
Extensions should be applied for by 15:00pm on the day of your original assessment submission date. Any applications after this time will not be considered and you will need to apply for mitigating circumstances.
If mitigating circumstances prevent you from submitting an extension request in advance, or mean that you miss the extended deadline that has been awarded, you should submit mitigating circumstances following the procedures outlined in the mitigating circumstances procedure. Please note, such requests for mitigation will only be considered where students provide a clear justification (including evidence) for failing to follow the normal extension request procedure.
Some DASS students are entitled to an automatic one-week extension, which does not need to be applied for. If you are a DASS student with this automatic extension and require longer than one-week, please complete the form above by 15:00pm on the day of your DASS submission date.
If you are on a clinical programme and your reason for an extension or mitigating circumstances may impact on your placement, your academic team will be made aware so that they can review your fitness to practice.
For all programmes, if you apply for repeated extensions your Academic Advisor will be made aware so that they can support you appropriately. If this exceeds four extensions in one semester, your Programme Director will also be informed.
Mitigating Circumstances
Sometimes, factors beyond your control may interfere with your ability to attend to your academic studies. The University’s mitigating circumstances procedures exist to try to mitigate against the impact that this could have on your grades.
The full mitigating circumstances policy can be accessed via the following link: https://www.studentsupport.manchester.ac.uk/study-support/mitigating-circumstances/.
We strongly recommend that you seek advice from a member of the Wellbeing team before submitting any claim for mitigating circumstances. You can contact them via shs.mitcircs@manchester.ac.uk or shs.wellbeing@manchester.ac.uk
Grounds for mitigation
Grounds for mitigation are unforeseeable or unpreventable circumstances that could have, or did have, a significant adverse effect on your academic performance.
Possible mitigating circumstances include:
- significant illness or injury
- the death or critical/significant illness of a close family member/dependant
- significant family crises or major financial problems leading to acute stress
- absence for public service e.g., jury service
Circumstances that will not normally be regarded as grounds for mitigation include:
- holidays, moving house and events that were planned or could reasonably have been expected
- assessments that are scheduled close together
- misreading the timetable or misunderstanding the requirements for assessments
- inadequate planning and time management
- consequences of paid employment
- exam stress or panic attacks not diagnosed as illness or supported by medical evidence
- disruption in an examination room during the course of an assessment which has not been recorded by the invigilators
Applying for mitigation
You should inform us if you experience difficulties that may negatively affect your performance on assessed work. You can inform us of such difficulties by submitting an online Mitigating Circumstances Form. The form must be completed by you. It will ask you to provide details of your difficult circumstances and to list the assessments affected. It is important that you list each separate assessment, giving details of the course unit and the nature of the assessment (e.g. PSYC10711 Essay or PSYC10100 Week 4 Quiz). Your form should also be supported with evidence, which is independent and time-specific (for example, a doctor’s note which confirms that you were ill and indicates the period affected). Our Student Support and Wellbeing team can advise you on the information required on the form.
You should inform us of mitigating circumstances as soon as you become aware that they might affect your performance. Typically, mitigating circumstances must be submitted prior to the assessment taking place. In exceptional circumstances, where it is not possible to inform us in advance, you should submit your Mitigating Circumstances application as soon as possible after deadline or scheduled examination, supported by a credible and compelling explanation of why your claim could not be submitted in advance.
Please note, not informing the University of circumstances due to personal feelings, e.g., shame, embarrassment and pride, or having concerns over the confidential treatment of requests for mitigation, are not considered to be credible and compelling explanations as to why the circumstances could not be made known or shown by these deadlines. If the details of the mitigating circumstances are considered to be highly confidential, you can discuss with the wellbeing team shs.wellbeing@manchester.ac.uk the best way to submit an application. The committee handle all requests for mitigation with sensitivity and due regard for confidentiality.
How mitigation is considered and applied
Evidence for personal and medical mitigating circumstances is considered by a mitigating circumstances committee. It is this committee’s role to determine whether there is evidence of mitigating circumstances, whether those circumstances could have had an effect on your performance, and the likely impact. The committee will consider all submissions and, where there is evidence that circumstances have been serious enough to have an effect on one or more elements of assessment, the committee will make recommendations to the exam board.
The exam board, at the recommendation of the mitigating circumstances committee, can take a limited number of actions to apply mitigation. In most cases, acceptance of the mitigation will involve revoking any late submission penalties or allowing for the missed or failed coursework/exam to be taken again as a first sit.
A claim for mitigating circumstances may be turned down for several reasons:
- The circumstances detailed by the student are not regarded as grounds for mitigation under the Policy on Mitigating Circumstances
- The supporting evidence does not cover the relevant period
- The supporting evidence is not supplied by an appropriate (independent) source
- The supporting evidence is deemed insufficient to support the student’s claim of the seriousness of impact on their assessment performance
- The wording of the evidence supplied does not support the student’s claim e.g. the material does not provide a medical diagnosis
- No evidence is provided, and the student has not given any explanation as to the reasons why nor indicated when evidence could be available
- The evidence relates to a chronic condition which the student is already in receipt of support from the Disability Advisory and Support Service (DASS). This does not include instances where the student has an acute flare up of a pre-existing condition which may be accepted if properly evidenced and confirmed by DASS
- The deadline for submitting mitigating circumstances has been missed, without a credible and compelling reason
- The claim relates to an ongoing condition or circumstance previously used to claim mitigation where the Panel, on the earlier occasion, instructed the student that this mitigation could not be used again and may have instructed the student to access support from the Disability Advisory and Support Service
MARKING CRITERIA – GUIDELINES FOR ACADEMIC ACHIEVEMENT
General Statements
Specific guidelines for each assignment will be issued by the unit leader. However, a set of general marking criteria is in use across the Division and these apply to all academic work at undergraduate level. These are as follows:
General Statements which apply across all Levels:
- At every level you should apply presentation guidelines as set out in the programme handbook/guidelines for the assessment.
- At every level you should adhere to the recommended method of referencing as set out in the programme handbook.
- At every level you should demonstrate (as a minimum) knowledge/awareness of acceptable standards of practice.
- At every level you are required to address the aims of the assessments as set out in the assessment guidelines.
You are advised to stay within the recommended word limit for assignments +/- 10%. The penalty which are levied for words in excess of this limit will be a ratio of 1% per 100 words.
The Division uses one set of generic marking criteria to mark all assessments. The marking criteria are structured on 9 themes:
- Transferable skills
- Learning outcomes and assessment criteria: adherence to the criteria for assessment in the question.
- Structure, planning and organization.
- Evidence of reading that is appropriate, relevant, broad, and accurately recorded.
- Use of research to support the discussion
- Knowledge and understanding of the topic, the main issues and the concepts
- Application of theory to practice
- Reflection on practice which identifies professional development and responsibility
- Arguments: the understanding of the topic and associated issues/debates
The level descriptors increase incrementally each year of the programme according to the academic level. All marking will reflect the descriptors and marks will be allocated from 0-100%.
The full marking criteria are available in the Assessments area of Midwifery Gateway on Blackboard. You are encouraged to familiarise yourself with the descriptors to gain a better understanding of the academic level required of your assessments for each year of the programme, as well as understand how marks are awarded according to the descriptors.
EXTERNAL EXAMINERS
The role of the External Examiner:
External Examiners are individuals from another institution or organisation who monitor the assessment processes of the University to ensure fairness and academic standards. They ensure that assessment and examination procedures have been fairly and properly implemented and that decisions have been made after appropriate deliberation. They also ensure that standards of awards and levels of student performance are at least comparable with those in equivalent higher education institutions.
External Examiners’ reports:
External Examiners’ reports relating to this programme will be shared with student representatives at the BMidwif (Hons) Programme Committee, and details of any actions carried out by the programme team/School, in response to the External Examiners’ comments will be discussed. Students should contact their student representatives if they require any further information about External Examiners’ reports or the process for considering them.
The External Examiners for this programme are:
Year 1
Zoi Vardavaki, Senior Midwifery Lecturer, London South Bank University.
Year 2
Priti Patel, (Programme External Examiner) Senior Midwifery Lecturer, Lead Midwife for Education, London South Bank University. (Tenure ends December 2023)
Year 3
Claire Clews, Senior Lecturer in Midwifery, Lead Midwife for Education, University of Northampton.
Year 4
TBC
Please note that it is inappropriate for students to make direct contact with External Examiners under any circumstances, in particular with regards to a student’s individual performance in assessments. Other appropriate mechanisms are available for students, including the University’s appeals or complaints procedures and the UMSU Advice Centre. In cases where a student does contact an External Examiner directly, External Examiners have been requested not to respond to direct queries. Instead, External Examiners should report the matter to their School contact who will then contact the student to remind them of the other methods available for students. If students have any queries concerning this, they should contact the Programme Office.
DBS AND ANNUAL DECLARATION OF GOOD HEALTH & GOOD CHARACTER
The offer of a place to study on this programme is conditional upon clearance of your suitability to practise Midwifery, following investigation and consideration of any past criminal convictions or cautions. Enhanced disclosure will be undertaken through the Disclosure and Barring Service (DBS). A self–declaration before commencing will be compared with a DBS completed soon after you start the programme. The DBS may be repeated at any time during your studies. If information is subsequently provided through the DBS which indicates that you may not be a person fit to practise, full consideration will be given to your continuation on the programme, but you may be excluded from the programme at any point on the basis of information provided to us by the Disclosure and Barring Service.
You are responsible for keeping your certificate from your Disclosure and Baring Service and are advised to keep a record of your DBS number and issue date. In some practice areas you may be asked to provide evidence of your DBS number and issue date.
You are required to provide the Division with information relating to any charges, convictions or cautions, which you may have received either in this country or in other countries as soon as you can after receiving it. You must also complete this declaration on an annual basis. Any information provided is treated in the strictest confidence and may not necessarily lead to a reconsideration of your position on the programme. However, failure to disclose any information at this stage, which may be provided to us at a later date by the Disclosure and Barring Service through its enhanced disclosure, will be viewed most seriously and will result in a reconsideration of your suitability to practise. You will be sent an electronic form to complete at the start of each academic year.
See also: Behaviour & Professional Conduct
OCCUPATIONAL HEALTH CLEARANCE
Continuation on the programme is conditional on continued health clearance. The BMidwif (Hons) / MMidwif programme is predicated on an integrated model of learning combining both theory and practice. If at any stage the Division is notified that you are not fit to attend, either by an advisory notification from Occupational Health or through a GP fit note you would normally be placed on sick leave (attending neither theory or practice). A continued period of sick-leave may lead to a period of interruption from the programme. See also: Attendance and Interruptions.
In order to maintain safety for the public, your colleagues and yourself, the Division will defer to the advice and recommendations of Occupational Health in matters of health and fitness for the programme.
During the course of your programme you may engage in Exposure-Prone Procedures and you should follow the guidelines in the Division’s Exposure-Prone Procedures Policy (https://documents.manchester.ac.uk/display.aspx?DocID=46917). If you have any concerns about your own health in this regard please refer to the advice available on Blackboard.
Note that you will be asked to engage with a risk assessment process in relation to attending placement during the COVID19 pandemic. Students who at any point are assessed as being at very high risk from COVID19 will be asked to discuss the option to interrupt their studies until their risk is lower or until the risk from COVID19 in the UK has declined. Engagement with the risk assessment process is required before placements can be confirmed. The University of Manchester works closely with NHS partners and other Greater Manchester Universities to ensure a high quality and consistent approach to health and safety in all learning environments.
The Occupational Health Department operate an ‘open door’ policy where you can make an appointment at any stage of your course. Where you self-refer to Occupational Health no report or contact with the Division is made without your consent. If it is mutually agreed that a report would be helpful then this will be undertaken with your consent.
If you have health concerns (physical or psychological) or a disability that affects your ability to study you may be referred formally to the Occupational Health Service by anyone with a concern e.g. Division, accommodation pastoral team etc. You may also be referred if study is affecting your health. The referring party should advise you of the reason for referral. When referred, the Occupational Health department will email you to arrange an appointment time.
In making decisions with regards to medical fitness for the programme, Occupational Health will ensure that they comply with relevant legislation, e.g. Equality Act 2010 and National Fitness Standards.
The Occupational Health Physicians and Occupational Health Nurses are all bound by the Code of Professional Conduct as set out by the GMC and NMC and the information you provide to the Occupational Health Service is subject to the General Data Protection Regulation (GDPR) and the Data Protection Act 2018 and will only be divulged with your informed consent.
You must inform your Academic Adviser or self-refer to Occupational Health if you are pregnant: see Policy for Pregnant Students. Pregnancy may affect your COVID19 risk status so it is important to discuss this with your Academic Adviser.
You must inform the Occupational Health Services of any needlestick or sharps injury which occurs whilst on placement in addition to meeting the accident reporting requirements of the NHS placement provider. You must also notify your academic adviser.
RESPONSIBILITIES OF STAFF AND STUDENTS
The Student Charter
Students on the BMidwif and MMidwif sign up to both the University’s Student Charter and the Division’s Student Charter and Conditions of Practice Experience (This can be found in the Appendix at the end of this handbook).
Checking Blackboard & your University email account
The Division uses Blackboard as the central location for information about all student resources. You will be given training on how to use Blackboard in your induction.
As a student you are required to check Blackboard daily, as this is where the Division would post both generic and specific information relating to course units and programmes. You will have access to course unit areas in Blackboard for the duration of the programme.
You are also required to check your university email account regularly as this is the agreed method of communicating with students so you will miss important information if you do not read your emails regularly.
Blackboard Student Communities
The various Blackboard community pages such as Midwifery Gateway and the Practice Learning Gateway have been devised to provide information that is generic to all course units within the programme. Please explore these sites to find lots of important information to help you get going with your studies.
3. PRACTICE LEARNING
THE ARRANGEMENT OF PRACTICE LEARNING EXPERIENCES
The placement of any midwifery or nursing students within the maternity services of the NHS Trusts affiliated with The University of Manchester should be negotiated through the Allocations Officer for this programme.
Different Trusts organise the provision of midwifery care in different ways so learning environments will vary from Trust to Trust, although the Allocations Officer in conjunction with the Academic Lead for Midwifery Practice will ensure that you experience the range of learning environments needed to meet the practice learning requirements of the programme.
The Allocations Officer will normally inform you of your allocation at the beginning of the programme and thereafter, prior to the commencement of each year of the programme. Notification will be provided via your university e-mail.
The BMidwif/MMidwif programme will expose you to learning environments in two different hospital sites across the Greater Manchester region to facilitate a variety of experiences. In year 1, we endeavour to provide learning experiences in one hospital, and then another hospital for years 2 and 3 (and 4 if applicable). However this arrangement is subject to availability and the provision of maternity services in the area.
You will be allocated a Practice Assessor in each year / part of the programme, who will assess your learning and development across several learning environments.
HUB & SPOKE
During some allocations you may want to arrange to visit a related department or gain relevant experience. An example might be that during your allocation to the antenatal clinic you would like to spend an afternoon in the ultrasound scan department when there is no official clinic running. Your Practice Supervisor(s) / Practice Assessor should facilitate the organisation of this and any requests should be raised during the initial interview.
As you move through the programme you should document evidence of having cared for maternity service users with concurrent medical or gynaecological conditions. You should also arrange spoke visits (where available) to relevant medical and gynaecological learning environments to develop your understanding further. This experience should also be documented in the MORA, within the ‘Complementary placement records’, to evidence that you have met the EU requirements in this field. The PEFs will provide details of how to organise spoke visits.
CONTINUITY OF MIDWIFERY CARER
Evidence supports midwifery continuity of carer as a safe and effective model of care, which optimises outcomes and enhances individual experiences for childbearing women/people, their babies and families (Perriman et al., 2018; Sandall et al., 2016; Forster et al., 2016; Rayment-Jones, 2015; Mclachlan et al., 2012). Continuity of carer (CoC) is a central aspect of maternity policy and has become a focal part of the National Maternity Transformation Programme (NHS England, 2016; NHS England, 2017). In recognition of the importance of CoC, and the future midwife’s role working within this model of care, the new NMC standards of proficiency for midwives (NMC, 2019a) have devoted a whole domain to continuity: ‘Domain 2: Safe and effective care: promoting and providing continuity of care and carer’. This domain stipulates the CoC requirements for undergraduate midwifery students to “demonstrate the ability to provide continuity of midwifery carer across the whole continuum of care and in diverse settings for women and newborn infants with and without complications and additional needs” (NMC, 2019a., pp. 17)
The provision of midwifery students CoC has been identified to be beneficial for professional learning, development and skills acquisition (Moncrieff et al., 2020; Sidebotham and Fenwick, 2019; Rawnson, 2011). Similarly to CoC provision by qualified midwives, continuity by student midwives has been shown to have a positive impact for the individuals receiving the care and associated with improved clinical outcomes (Tickle et al., 2021).
CoC is a key thread that runs throughout the programme, in both university-based theory and practice-based learning. By embedding CoC in this way as a student midwife you will be exposed to optimal learning opportunities, which will continuously enable you to link your acquired theoretical knowledge and practice-based experience of CoC. The hybrid programme structure has been developed to enhance learning, enabling you as a student midwife flexibility and the opportunity to maximise your experience of midwifery continuity. As a student midwife within the practice learning environment, you will be involved in the provision of maternity care through the pregnancy continuum, including holding a small caseload. The level of your participation in this care will develop throughout the course and in accordance with your stage of learning. This practice-based learning will complement your theoretical learning; starting in year one with a focus on universal care and midwifery-led care pathways, and then developing from year two to include continuity of care for those with additional needs. This structure of your CoC experience within the practice learning environment is outlined as follows:
- Year 1: As a student midwife you will observe and participate in the provision of care through the pregnancy continuum for a small number of women/people on a midwifery-led pathway
- Year 2: As a student midwife you will contribute to the provision of continuity of carer for a small caseload of women/people, including those with additional care needs
- Year 3: As a student midwife you will demonstrate proficiency in providing continuity of carer for a small caseload of women/people. You should aim to recruit some women/people with additional needs or complexities that enable further self-development of specific skills
- Year 4: As a student midwife you will gain further experience related to working within a continuity of carer team/model
Your experiences of providing CoC within the programme will be used as evidence of your developing proficiency in providing midwifery care across the childbearing continuum. Your experiences should be recorded and reflected upon in the MORA. The NMC standards for supervision and assessment (NMC, 2018a) will be adhered to for all practice-based learning and therefore for all CoC experiences as a student midwife you will be working under the supervision of a qualified midwife. In partnership with the practice learning providers the University will provide clear guidance and support for you regarding student midwives’ provision of CoC. This will optimise the CoC learning experience (Moncrieff et al., 2020) alongside promoting safety for yourself as a student midwife and for the individuals you are caring for.
ATTENDING HOME BIRTHS
We would like to facilitate your attendance at home births where feasible. If you have a home birth imminent in your community area, you should discuss this with your Community Practice Supervisor and with your unit leader(s) so that they can highlight sessions that must be attended and those that could be made up later should you need to attend the birth during a theory day. A maximum of 3 days per year of theory time may be used in this way. Missed theory sessions must be made up. Additional practice hours can be documented in PARE.
MIDWIFERY ONGOING RECORD OF ACHIEVEMENT (MORA)
Assessment within the Midwifery Ongoing Record of Achievement (MORA) evidences your development towards the required proficiency of all midwives and forms an important part of the assessment strategy over the programme. The MORA is hosted by an online platform called Practice Assessment Record & Evaluation (PARE) https://onlinepare.net. PARE also allows you to provide feedback and evaluation of your learning experience in an easy and timely manner. The feedback that you provide is essential to ensure that practice learning experiences are enhanced and supported for all learners in practice.
The Midwifery Ongoing Record of Achievement (MORA) comprises:
- NMC proficiencies that relate to the NMC Standards of proficiency for midwives (NMC, 2019); a proportion of which must be achieved to a specified level in each year of the programme.
- Space for you to generate evidence of achievement of proficiencies, including:
- Practice Episode Records
- Breastfeeding assessment records
- Feedback from Supervisors
- Feedback from service users
- Your own reflections
- Records of clinical experiences of providing care for a certain number of women/birthing people and babies, to achieve Directive 2005/36/EC
- This includes records within the Complementary placement records
- Practice Assessor reviews, including 2 formative assessments and 1 summative holistic assessment each year
- Records of meetings
- Records of your completed practice hours
Further guidance on use and completion of the MORA is available on PARE in the ‘MORA Context Document’ and in the ‘Student Guidance’ section.
PRACTICE LEARNING REGULATIONS & GUIDELINES
All learners are allocated to practice learning environments that meet the requirements of the curriculum. All learning environments undergo an education audit and have assurances that there are enough Practice Supervisors and Practice Assessors to support teaching and assessment of students in practice. You will be allocated to a variety of learning environments to ensure you experience practice across a range of settings. The provision of learning experiences throughout the curriculum has been developed and expanded in partnership between service and University colleagues. You will be required to travel to your allocated learning environment.
Learners are normally informed of their allocation to a learning environment 4 weeks prior to commencement. Notification of allocations is via your student e-mail account. Students MUST contact the learning environment 2 weeks prior to commencing to discuss arrangements for arrival. Learning environments allocated to learners will not normally be changed. In exceptional circumstances learners may request a change to their allocation by completing the Trust Change Request form available on Blackboard within the Practice Learning Gateway.
Your Academic Adviser / Academic Assessor is available for you to discuss your MORA development and practice learning progress. Should you have any areas of concern relating to your learning environment you can discuss these with your Academic Adviser / Academic Assessor. There are also formal procedures available to report your concerns / evaluations of your practice experiences: guidance on providing feedback and raising concerns is available in the Practice Learning gateway in Blackboard.
If you sustain a sharps injury or needlestick injury in the learning environment, you must report this immediately to your Practice Supervisor / Practice Assessor and Academic Advisor. You must also attend the University Occupational Health Department for review, even if the learning environment ask for you be reviewed at your trust Occupational Health Department.
See also: Attendance requirements
WHO WILL BE AVAILABLE TO SUPPORT ME DURING MY PRACTICE LEARNING EXPERIENCE?
Practice Supervisors (PS)
Registered Midwives or other registered health or social care professionals are able to be Practice Supervisors. They have current knowledge and experience and are appropriately prepared for the role in which they;
- Ensure safe and effective learning experiences
- Facilitate independent learning
- Provide co-ordination and continuity of support and supervision
- Ensure observation on your conduct, proficiency, and achievement of programme outcomes are shared with key staff, for example, other Supervisors
- Contribute to assessment and record regular feedback
They have responsibilities for overseeing your progress during your learning experience and may undertake your initial interview supporting you to identify your learning needs, discussing the learning opportunities and completion of your learning plan.
Supervisors have an important role in contributing to your assessment and giving you regular feedback, collaborating with other Supervisors and your nominated Practice Assessor. You may, depending on your allocated learning environment, have several Practice Supervisors supporting your development.
Practice Assessors (PA)
Practice Assessors for midwifery students must be Registered Midwives with current knowledge and expertise and are appropriately prepared for the role in which they;
- Conduct assessments, informed by feedback from Practice Supervisors
- Make and record objective decisions, drawing on records, observations, student reflection and other resources
- Periodically observe you in practice (by objective evidence-based assessment)
- Gather and coordinate feedback from Practice Supervisors and other relevant people
- Schedule communication with Academic Assessors at relevant points
- Review assessment documentation in your MORA that has been completed by your Supervisor(s) and a range of other health or social care professionals who have contributed to your development
- Assess your conduct, proficiency and achievement of proficiencies and will complete the 2 formative reviews and final summative holistic assessment and review of proficiency achievement at the end of the year.
As well as undertaking the required supervision and assessments, the role of the Practice Supervisor and Practice Assessor also includes identifying relevant learning opportunities and creating learning and development plans with the student. In situations where a concern is raised about progress, knowledge-base or conduct, a progression plan will be developed by your Practice Assessor in collaboration with you and your Academic Assessor.
Academic Assessors (AcAs)
Academic Assessors must be Registered Midwives who are nominated for each Part of the programme and are appropriately prepared for the role which includes;
- Working in partnership with your Academic Adviser
- Working in partnership with the Practice Assessor to evaluate and recommend you for progression for each part of the programme. In this context a part refers to the end of each year
- Understanding your learning and achievement in practice
- Undertaking scheduled communication and collaboration with your Practice Assessor
- Collating and confirming your achievement of the proficiencies required within each part of the programme, based on assessment and information that is objective and fair
You will be allocated an Academic Assessor for each Part of the programme (i.e. each year) and within each year there are different levels of performance that you need to demonstrate.
Academic Assessors will collate and confirm your achievement of the proficiencies required within each part of the programme. They will review your progress throughout the year and complete the final assessment in collaboration with the Practice Assessor, having considered your progress and all the evidence. Your Academic Assessor will review your MORA progress following each Practice Assessor review (formative and summative reviews), as indicated on your timetable. If there are any development needs in relation to your performance, they will work with the Practice Assessor in agreeing a progression plan. The progression plan will be reviewed by your Practice Assessor and Academic Assessor together to ensure that the progression plan outcomes have been achieved, or consider further actions. Following the summative holistic assessment (and a retrieval opportunity, where needed) at the end of each part, the Academic Assessor will confirm achievement of the outcomes required in that part or indicate non-achievement.
Your Academic Assessor in the final allocation in your final year will review and confirm overall achievement of the programme practice requirements in collaboration with your Practice Assessor to recommend progression to registration.
Practice Education Facilitators (PEF)
Practice Education Facilitators (PEF) are Trust employees whose role is to facilitate learning in practice for all undergraduate healthcare students, with a particular focus on quality assurance and inter-professional learning. The PEF has an overview of your learning environment and is a point if contact if needed. Please refer to the Practice Gateway within Blackboard for further information. In some trusts, there are Practice Education Practitioners (PEPs) who support the PEFs.
University Link Lecturers (ULL)
An ULL acts as the primary link between the University and the learning environment.
The Midwifery ULL role includes:
- Working effectively as a team with PEFs, taking a risk assessment approach, to ensure the provision of appropriate learning environments
- Provide student, Practice Supervisor and Practice Assessor support
- Working collaboratively with all stakeholders and ensuring good channels of communication are in place
A list of ULLs is located via the Practice Learning Gateway within Blackboard.
Student Illness during Practice Learning Experiences
If you are ill or absent for any reason during practice learning experiences, on the first day of absence you should inform your Practice Supervisor / Practice Assessor (or a designated deputy) of the reason. You can report this illness yourself or you can ask someone else to report it on your behalf if necessary. We recommend you let your Academic Adviser know that you are off sick.
If you are unable to attend your learning environment for any reason it is important that:
- All relevant people are informed in the interest of professionalism and safety
- Your absence is noted on your PARE timesheet
Please note that nursing / midwifery students are not automatically entitled to Wednesday afternoons off. If you are a member of a university club which meets on a Wednesday afternoon you can try to negotiate this time off with the Practice area, but you will need to make this time up on another weekday or at the weekend.
Due to NMC regulations, all absences including authorised absences must be made up to complete the programme. You can find guidance on making up missed practice hours on the Practice Learning Gateway in Blackboard.
ATTENDANCE IN PRACTICE
All students are required to work the normal shift times of their learning environment starting and finishing at the same time as other staff (with similar breaks). Commitment to attendance and punctuality is important and will be closely monitored.
During the programme you are considered as supernumerary, this means you are not calculated as part of the workforce, it does not mean you are unable to undertake any duties. You will be expected to observe and participate in clinical activities and duties with supervision as appropriate to your level and abilities.
You will be expected to work early and late shifts, standard and long day shifts and some night duty. You are also expected to work some weekends with your Practice Supervisor(s). Requests for a bank holiday as a day off should be considered sympathetically. In some learning environments and for your continuity of carer experiences you will be expected to work ‘on-call’ duties alongside your Practice Supervisor. If you have difficulty meeting the ‘on-call’ requirements of the learning environment, you should discuss this with your Academic Adviser. Bank holidays are included in your annual leave allocation, therefore you should work a normal week, without an extra day off during a bank holiday week.
It is not acceptable to swap days off unless in an emergency as this will affect planned practice supervision and therefore your assessment. If you are having any difficulties in practice you should speak to your Academic Advisor.
It is not acceptable for you to use the days allocated for practice for other purposes such as completing assignments or attending academic tutorials – unless confirmed in writing by the Academic Adviser. Time is allocated for these activities during the study days.
Further guidance and support about working shifts can be found on Blackboard within the Practice Learning Gateway.
You are expected to attend all practice days. Any time missed will need to be made up due to statutes concerning midwifery education which dictate the length of education and training that each student must undertake in order to be eligible to register as a midwife.
Further guidance about the attendance regulations for this programme can be found later in this handbook. Non-attendance due to paid employment commitments is considered to be un-authorised absence and will be responded to in accordance with the programme policy.
Any changes to allocated off duty can only be authorised by the student’s Practice Supervisor / Practice Assessor who may ask for an explanation. Swapping of shifts/practice weeks to make up for sickness or absence or to change holiday weeks is not permitted. Amendments to allocations can only be made by the Allocations Officer. Additional shifts may be planned with your Practice Supervisor to help you make up missed practice time – see the making up time policy available on Blackboard within the Practice Learning Gateway.
Online Timesheets in PARE are used for recording attendance in practice. These are completed by the student and signed by the Practice Supervisor(s) on a daily basis. These completed timesheets are required as evidence of meeting the 100% attendance requirements of the programme. If these are not complete at the end of each semester it may prevent progression to the following semester. Students are strongly advised to get their timesheet signed each shift as it is difficult for Practice Supervisors to remember what shifts you worked once the learning experience has been completed. Practice Supervisor(s) may refuse to sign old timesheets so you may need to work those hours again.
Any sickness or absence during your learning experience must be reported to the placement and noted in your online timesheet in PARE. You should also notify your academic adviser of any sickness or absence affecting your attendance.
When you are on a practice learning experience, you remain a registered student of The University of Manchester and will continue to be governed by The University of Manchester’s Rules and Regulations. You should also abide by any relevant learning environment area rules and regulations.
CAR INSURANCE
Please note that when undertaking learning experiences, students may invalidate their car insurance if they make journeys after their arrival on duty as this may be considered to be using your vehicle for work purposes. Many insurance companies will allow policy holders to travel between different places of work without it being classed as business use. Any car use during the working date other than to travel to or from your work base could be considered as business use, so any such use should be checked with insurers.
4. STUDENT PROGRESSION
ATTENDANCE REQUIREMENTS
In keeping with Regulation XX – Monitoring Attendance and Wellbeing of Students, the University records and monitors your attendance to:
- Support academic attainment and progression;
- Ensure student wellbeing; and
- Satisfy external reporting/accreditation requirements.
As a student on the BMidwif/MMidwif programme you are required to complete both theoretical and practice-based learning. In accordance with the NMC standards governing our current programme, you will need to complete the whole programme which totals 4600 hours of learning over the course of the BMidwif programme or 5468 hours learning over the course of the MMidwif programme, 50% of which takes place in practice (NMC, 2019).
You are expected to engage fully with all theory and practice components of the programme. This includes attending/completing 100% of University timetabled teaching activities (synchronous and asynchronous lectures, seminars, skills teaching, Academic Adviser meetings, etc.), practice hours for each clinical placement, and completing independent study as indicated on the timetable.
Students cannot have more than 150 hours of practice learning outstanding at the end of one part / academic year of the programme. Students having less than 150 hours outstanding will be noted at the September Exam Board and be given retrieval opportunities to complete their hours and/or practice learning outcomes prior to a final board in late November/early December. Students who have amassed more than 150 hours of practice learning outstanding will be reviewed and may be required to interrupt the programme and recommence at a later date subject to eligibility to resit.
A full version of the BMidwif/MMidwif attendance policy as approved by the programme committee is available in Midwifery Gateway on Blackboard.
Reporting Absence
It is important that you are aware of attendance expectations and keep the Division appropriately informed of any issues affecting your ability to attend either theory or practice. If you are unable to attend you must notify the Division at the start of your period of absence. This should be done by emailing BMidwifery@manchester.ac.uk and your academic adviser.
You should detail the reason for the absence (for example: sickness, childcare) and the anticipated length of the absence. If you are absent on placement days should also contact your clinical placement to inform them of your absence – an important professional responsibility.
The Division differentiates between authorised and unauthorised absence from the programme. Absence from the programme can be authorised due to documented sickness, or by an Academic Adviser or Year Lead for other reasons. Please note that due to NMC regulations, all absences including authorised absences must be made up in order to complete the programme.
Absences due to sickness of between 1 and 7 days can be self-certified. Sickness absences of more than 7 days require a doctor’s note. Absences due to other reasons such as carers leave, compassionate leave or attendance at an interview or conference can be authorised by an Academic Adviser who will complete an authorised absence form which is submitted to the Programme Director.
Attendance Monitoring
Due to the professional nature of the course there is a 100% attendance expectation. Any time missed must be made up in order to meet the requirements of the NMC.
Attendance at all synchronous (or live) theory sessions will be monitored, including face-to face and online teaching. It is your responsibility to ensure that you register your attendance.
Do not sign anyone else in on the register and do not request a friend to sign you in. If you sign the register for anyone else or request that some else signs to say you were present, this contravenes the NMC Code for Professional standards of practice and behaviour for nurses, midwives and nursing associates (NMC 2018). See standards 10.1, 10.3, 10.4, 20.2. The programme team will take action if you sign for anyone else. This may be considered evidence of fraudulent documentation and dishonesty and can result in a Fitness to Practice Committee Referral and even discontinuation from the programme.
If you are sometimes struggling to attend the taught sessions, please seek support and discuss this with your academic advisor.
It is your professional responsibility to complete all asynchronous (or not live) theory sessions, such as online activities, pre-recorded lectures, and guided reading. These are timetabled to assist you in pacing your studies and to help you prepare for future live theory sessions, simulation, or assessments, hence it is strongly recommended that you complete them on the day they are set.
Engagement with asynchronous activities and the unit overall may be periodically monitored via quizzes or online tasks.
Any theory session that is missed needs to be completed through private study. You need to complete the work and then fill in a Missed Teaching form (available from Midwifery Gateway – Forms & Uniforms). The form should be sent, along with any supporting evidence of the work you have completed, to your unit teacher/unit lead for approval. Some sessions cannot be made up via the missed teaching process. You will be advised about other options for catching up this missed learning opportunity.
On practice days, you must report your absences to the Trust, the University and your Academic Advisor, irrespective of plans for the time to be made up.
Trigger points
In order to support academic attainment and monitor wellbeing, Academic Advisers will be given regular updates of their Advisees’ attendance profiles. Students who reach trigger points (detailed below) will be flagged to the Academic Adviser for follow up.
The role of the Academic Adviser in attendance monitoring is a supportive one, to ensure that you are well and engaging with the programme. Academic Advisers will treat cases of poor attendance on an individual basis, but would normally complete a ‘poor attendance interview’ and agree a range of actions with you. These may include regular meetings, referral to Occupational Health or revisiting guidance on the attendance requirements.
| Trigger point | Detail | Action |
| First | 10 hours of absence | Student is contacted to ensure they are aware of absence notification procedure, remind of how to make up missed sessions and encourage student to seek support from AA if there any issues affecting attendance (AA copied in). |
| Second | 15 hours of absence OR Ongoing problems with attendance relating health or personal difficulties | Academic Adviser informed and student invited to a meeting to discuss their attendance; practice attendance will also be reviewed. A plan for making up missed theory and/or clinical hours agreed. An informal warning may be issued, with requirement to improve attendance. |
| Third | 20 hours of absence OR Ongoing problems with attendance relating health or personal difficulties 25 hours of absence OR Ongoing problems with attendance relating health or personal difficulties | As above. A formal warning may be issued, with requirement to improve attendance. |
| Forth | As above. Programme Director informed. Student may be compelled to interrupt the programme, or asked to clarify whether they have withdrawn. Student may be referred to Fitness to Practice / Health & Conduct Committee. |
Consequences and sanctions
Academic Advisers aim to support students to achieve full attendance. If you do not meet the attendance requirements despite supportive measures you may be compelled to interrupt the programme or be invited to the Fitness to Practice Committee. Sanctions of the Fitness to Practice Committee in matters of poor attendance include formal written warnings, requiring you to repeat the year of study, discontinuation from the programme and referral to the Faculty of Biology, Health & Medicine Fitness to Practice Committee. The guidance on Managing Attendance and Reporting Absence can be found in Appendix II and in the Student Gateway.
If you are absent without explanation or contact for an extended period you will be asked to formally clarify your intentions regarding the programme. Failure to respond to this will lead to discontinuation from the programme, using the last known date in attendance.
Advice & Support
You are encouraged to be proactive in seeking support and managing any issues that impact your attendance or wider ability to engage with the programme. Academic Advisers are the primary source of pastoral support within the programme, but you may also access support from the Senior Academic Adviser, Year Lead and Student Support Office within the Division, as well as University services including Occupational Health, the Disability Support Office and the Counselling Service.
See also: Student Support.
PROGRAMME INTERRUPTIONS AND WITHDRAWALS
It is the expectation that you will pursue your studies on the BMidwif (Hons) or MMidwif programme on a continuous basis for the duration of your programme, and complete within 3 or 4 years of commencement, respectively.
If you are experiencing uncertainty about your position on the programme should contact your Academic Adviser for advice and support in the first instance. The Programme Director or Senior Academic Adviser are also able to offer you support.
Withdrawals
If you decide that you are unable to continue your programme, you can withdraw from your studies. You will need to be aware of the below implications when considering withdrawing from the programme, so we would always advise discussing any queries you may have with the Student Support and Wellbeing Team/Programme Director/Year Tutor/Academic Advisor.
- Tuition Fees
- Accommodation (if living in UoM halls)
- Future career prospects
If you then wish to withdraw from the programme, either via email, during a welfare meeting, or following a meeting with an AA, you will need to complete a SHS Withdrawal Request Form, which can be obtained by contacting the Student Support and Wellbeing team on shs.wellbeing@manchester.ac.uk
Students need to complete and sign the form, returning it back to the shs.wellbeing@manchester.ac.uk email address. No supporting evidence is required for a request to withdraw. The form will then be sent to the relevant member of academic staff for approval (this may be the Programme Director, Year Tutor or Academic Advisor).
Once the Student Support and Wellbeing Team has received the form which has been approved by the relevant member of staff, a standard confirmation letter will be sent to you confirming the details of the withdrawal.
Policy for Pregnant Students
If you become aware that you are pregnant you should initially inform your Academic Advisor. You should arrange to meet with your Academic Advisor to secure a referral to Occupational Health and to discuss your plans for maternity leave. You should also examine with them the implications for your studies in relation to sharing information with clinical colleagues if on placement and also the need to secure a formally agreed authorised absence from your studies via the interruptions policy as extant within undergraduate programmes.
In all instances you are required to inform the School of your pregnancy and to secure an appointment with Occupational Health to ensure that all necessary support mechanisms and reasonable adjustments are in place to protect yourself, especially in relation to risk associated with COVID infection.
Prior to any period of interruption you will need to meet your Programme Director and Academic Advisor to formalise and agree the interruption. At this interview you should complete a Request for Interruption Form and agree the date of interruption and a provisional return date. It is your responsibility to contact the school 15 weeks prior to your return to confirm your intentions.
You are required to provide the University with some form of confirmation of the pregnancy before commencing maternity leave, for example, a MATB1 form, which is available from a GP or midwife. This form is usually provided once a pregnancy has been established for 20 weeks.
If you are in receipt of the Learning Support Fund (LSF) – Training Grant, Parental Support and Exceptional Support Fund – you may be considered for continued payment up to the last date of the payment term in which you began your authorised period of leave. There are 3 terms in the LSF payment year; November, March and May. No further LSF payments will be made until you return to the programme.
Please self-refer to Occupational Health in the first instance if you experience any problems with your pregnancy that you feel impacts on your programme of study.
Pregnant Students and Practice Placements
For students engaging in clinical practice a Risk Assessment will be required:
Students must inform the placement manager of their pregnancy on each placement so that a risk assessment specific to the area can be undertaken and recorded. Likely areas to be considered may include:
- Participation in manual handling procedures
- Exposure to radiotherapeutic investigations
- Sequencing and length of shift patterns
- Exposure to infectious disease
- Working in Theatres
- Preparation and administration of cytotoxic chemotherapeutic agents
- Exposure to hazardous waste
- Provision of Uniforms
- Access to rest areas
- Students who are non-responders to Hepatitis B vaccination, may require restrictions to practice based on risk assessment.
Students Returning to Study
You will be informed that you must take at least two weeks compulsory leave following birth by law: Pregnancy and Maternity Rights.
It is your responsibility to contact the school 15 weeks prior to your return to confirm your intentions.
You will be required to have a review with Occupational Health prior to your return to secure clearances to recommence your programme of study.
Interruptions
It is the expectation that you pursue your studies on a continuous basis for the duration of your programme. It is recognised however that you may encounter unforeseen circumstances which may significantly disrupt your studies and prevent them from completing the programme in the normal timeframe.
If at any point in your studies you feel that you need to take some time away from your degree, you can interrupt your studies and return once you are ready. You need to be aware of the below implications when considering taking an interruption, so it is best to discuss any queries you may have with the Student Support and Wellbeing Team/Programme Director/Year Tutor/Academic Advisor.
There are a few important things to think about when deciding to interrupt:
- Primarily, your wellbeing. If an interruption is the best decision for you, it should benefit your present and future wellbeing and support you completing your degree to the best of your abilities.
- Tuition Fees
- Accommodation (if living in UoM halls)
- Possible changes to course content on return
- Tier 4 students MUST be referred to the Student Immigration Team in SSC to discuss consequences of interruption (3.2 Policy on Interruptions to UG and PGT Programmes of Study)
If you then wish to request an interruption to study, either via email, during a welfare meeting, or following a meeting with an AA, you would need to complete an SHS Interruption Request Form, which can be obtained by contacting the Student Support and Wellbeing team on shs.wellbeing@manchester.ac.uk. It is helpful to know at this stage how long you expect to interrupt for and when you might return.
You need to complete and sign the form, returning it back to the shs.wellbeing@manchester.ac.uk email address with any appropriate supporting evidence. The form will then be sent to the relevant member of academic staff for approval (this may be the Programme Director, Year Tutor or Academic Advisor).
*Please note that students will be contacted by the Student Support and Wellbeing Team prior to their return to study/return from interruption*
BMidwif policy regarding interruptions.
The University policy is that students can normally interrupt their degree studies for 1 year. In line with this, the BMidwif programme normally agrees an interruption for up to one year when requested by the student or required for progression reasons. However due to the demanding nature of the programme involving placement attendance as well as theoretical study, we are willing to allow students to apply to extend their interruption for a 2nd period (so interrupting for a further 12months), to help them overcome their personal difficulties and hopefully be able to return to study and practice at the appropriate point in the programme. An individualised plan for return from interruption will be developed with the student at the point of interruption and will then be reviewed several weeks before the student actually returns, to confirm the appropriateness of the plan in the light of their circumstances and learning & assessment needs at that time.
This limit of 2 years of interruption is to ensure that the student’s learning remains current so that they can provide safe and effective care for service users by drawing on their up-to-date knowledge and skills for midwifery practice. For this reason, a request for a 2nd year of interruption in the later stages of the programme may not be agreed, as the programme team need to be confident that the student is ready for clinical practice as a qualified midwife at the point of completion.
A limit of 2 years interruption will normally be applied to all interruption requests. In unusual circumstances, exceptions to this rule may be considered at the discretion of the Programme Director & Lead Midwife for Education. These circumstances will usually relate to the delivery of the programme such as major changes to the curriculum or the availability of placements.
Returning from Interruption
Once on interruption, it is your responsibility to keep in contact with the Division and confirm your intention to return to the programme. You will be given specific instructions for confirming your intention to return in your interruption approval letter, but will be required to give adequate notice for the Division to make administrative arrangements for your return. Returning from interruption may be subject to conditions set by the Programme, including academic progress, health clearance on approval by Health & Conduct or Fitness to Practice Committee. Where a return from interruption is conditional, this will be clearly indicated in the interruption approval letter.
Interruption by Student Request
If you feel that you would benefit from a leave of absence from the programme for any reason, you should initially discuss this with your Academic Adviser. You are encouraged to be proactive in accessing support, advice and guidance from your Academic Adviser, Year/Field Lead, Occupational Health, the Disability Support Office and Student Support Office as may be beneficial.
Formal requests for interruption are made by meeting with your Programme Director or Cohort/ Year Lead (or their acting deputy) to complete an Interruption Request Form (Appendix 1). If you are requesting interruption you should provide third-party evidence of your circumstances to enable the programme to fully consider whether an interruption is the best course of action for the you. Documentation submitted in support of an interruption may be shared with the Examinations Office in order to apply the mitigation circumstances policy to assessments affected by the circumstances leading to your interruption. Once used, evidence will be treated confidentially and kept on your file.
As the interruption meeting will include advice and guidance on the practicalities of interrupting and a personalised return plan it is anticipated that the request form would be completed during the meeting. In exceptional circumstances only this may be completed remotely. Final approval will be confirmed in the interruption letter which you should receive within 5 working days of the meeting.
As stated above support and guidance on the interruptions process is available via a number of means including Programme Directors, Academic Adviser, Student Support and Cohort/Year Leads. It is important to ensure that all cases for interruptions are dealt with in an efficient and proactive manner as future tuition fee and bursary funding may be affected.
Interruption by Divisional Committee
In rare cases, the Division may require a student to interrupt your programme. You would normally interrupt the programme as soon as it became apparent that either:
- You are in breach of the professional progression requirements of your programme
- You are not fit for study on the recommendation of Occupational Health or the Fitness to Study Committee
- You have failed to meet the attendance requirement of your programme as detailed in the relevant programme handbook
- The Programme Director judges that you will be unlikely to be able to meet the professional progression requirements and it in your best interest to commence a period of interruption immediately
This regulation is designed to protect you by minimising the amount of time that students repeat, which will impact you future funding.
Financial Support
Such a change in circumstances may have implications for your student finance and accommodation so we strongly recommend that you contact your Student Finance company and the University’s Student Services Centre (ssc@manchester.ac.uk / 0161 275 5000) for full details of how you will be affected. Further guidance can also be found here.
If you are in receipt of a student loan it is your responsibility to contact Student Finance UK to suspend your student loan.
Tuition Fees
If you receive a tuition fee loan from Student Finance, the amount you borrow depends on the date you interrupted:
| Liability Dates for 2023/2023 | Amount | |
| Withdrawal/interruption between 03/10/2022 – 15/01/2023 | 25% of the total fee will be charged | |
| Withdrawal/interruption between 16/01/2023 – 16/04/2023 | 50% of the total fee will be charged | |
| Withdrawal/interruption between 17/04/2023 – 09/06/2023 | 100% of the total fee will be charged |
You will not be charged fees during your interruption. If you are self-funding, and have overpaid fees i.e. for a period longer than your interruption date, you can request a refund or have the portion saved for next year. You should speak with the Student Services Centre for further information: funding@manchester.ac.uk
Student Finance Maintenance Loans:
We will inform Student Finance that you have interrupted your studies. They will recalculate your entitlement of maintenance loan and grant based on the date you last attended. This could mean that you have received more than entitled to, and they will ask you to pay back any overpayment of maintenance grant. Student Finance may pay up to 60 days sick pay in any one academic year where students interrupt for health reasons but payment post-interruption is at their discretion. If you have interrupted for health reasons, with your permission, we can inform Student Finance and they may pay an additional discretionary 60 days allowance of funding. More information can be found on the Money Advice Team Fact Sheets: https://www.studentsupport.manchester.ac.uk/finances/a-z/
The Learning Support Fund (LSF):
If you are entitled to funding from the LSF, the programme administration will them that you have interrupted your studies. They will recalculate your entitlement of Training Grant and Parental Allowance based on the date you last attended. This could mean that you have received more than entitled to, and they will ask you to pay back any overpayment of maintenance grant. You may submit any outstanding claims for travel and Dual Accommodation Expenses that were accrued prior to interruption within 6 months of the date they were incurred.
Access:
As you are not a registered student, your access to University premises will be the same as a member of the public; you will lose onsite IT and library access. However, you will retain access to My Manchester, your student email account and the Careers Service. You will lose access to some resources in Blackboard so download any materials that you will need. You can access:
Lecture podcasts via https://video.manchester.ac.uk/lectures
Blackboard archives via http://online.manchester.ac.uk/
Visa:
UKVI will be notified of your interruption and your visa will be cancelled; you will need to return home within 60 days. If you need advice about the implications your interruption will have on your immigration status, please contact the Student Immigration Team at the Student Services Centre (contact details below).
Interruptions Procedure: Interruption by student request
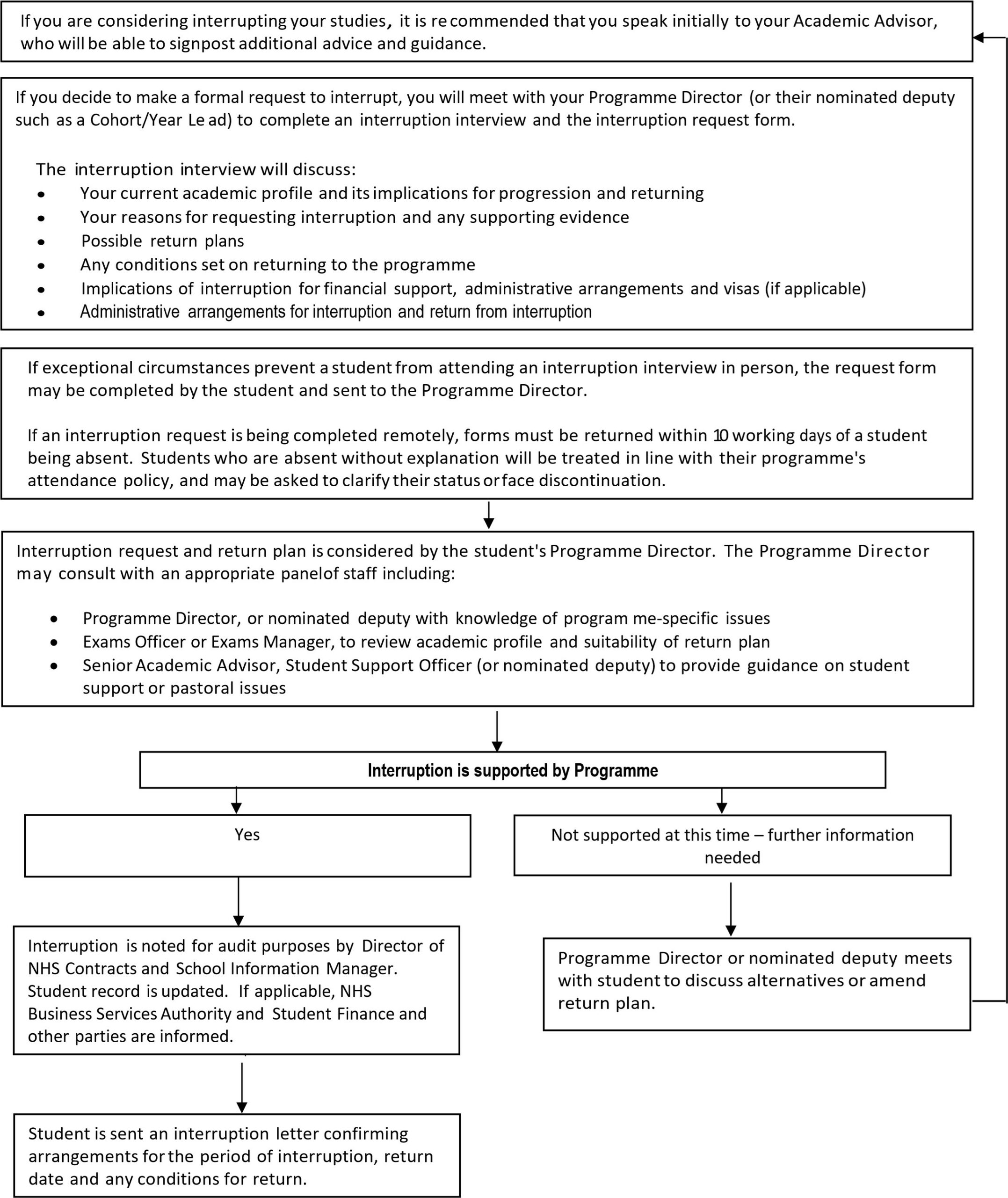
Return from Interruption
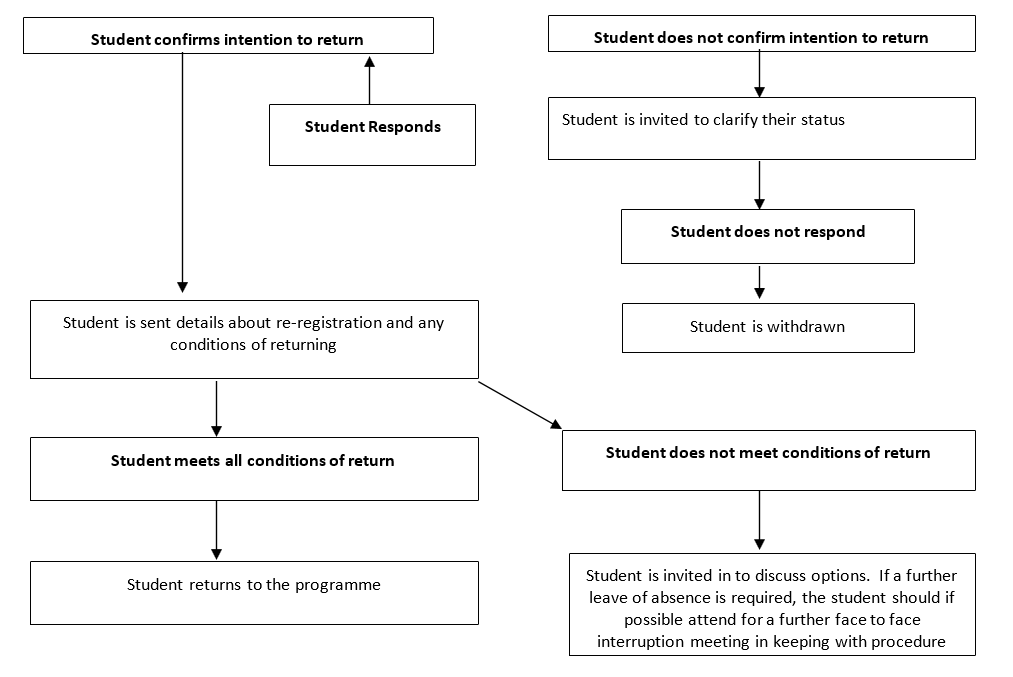
Student Finance: If your return date is in the next academic year, Student Finance will not automatically carry over your loans so ensure you re-apply.
If you interrupted for health reasons: Before you return, you must submit evidence from a medical professional that you are now well enough to resume your studies. We may refer you to the University Occupational Health department so this can be confirmed and we will arrange this before your return date. We will also arrange for you to meet with the Senior Adviser to discuss ongoing health needs. We may also refer you to the Disability Advisement and Support Service (if you are not already registered with them) if your condition is ongoing.
Under our regulations, long-term conditions will not normally be considered by the Faculty more than once. This means that you are unlikely to be able to apply for mitigation for the same reasons in the future unless there is a major change or exacerbation in your situation.
Literature Review/Project: We will try to maintain your supervisor; if this is not possible, we will assign a new supervisor or look for a similar subject area or project type if you have not yet commenced this unit.
Visa: Please email supportoffice.sbs@manchester.ac.uk 2-3 months before your return date to request a new CAS.
Making up time missed due to sickness and absence
Any absences from the course must be made up prior to registration as a midwife. There are two ways this time may be made up. These are:
- Making up a missed university day through private study to demonstrate achievement of the learning outcomes is at the discretion of the unit lead. Some theoretical sessions missed can only be made up by attendance at a later session on the same topic.
- You should complete a ‘missed Teaching Form’ (available via Blackboard), identifying what session you have missed and what private study you have done to catch up the missed session.
- You should take this to the unit leader.
- The unit leader will discuss the work and if satisfied, sign the form and update your record.
- You may make up missed clinical practice hours using the guidance in the Making up Time in Practice policy that can be found on the Practice Learning Gateway within Blackboard.
You are encouraged to review your attendance record periodically. This can be done by requesting a copy via your Academic Adviser. If you feel an error has occurred in you records, you should discuss this with your academic adviser as close to the time as possible. Records can only be altered with written confirmation from the Academic adviser or Unit Leader.
If you have sickness / absence time to make up, you should bear this in mind when planning holidays at the end of the course. It is the normal policy that you must make up your time before you take your final weeks of holiday. However, if you have a lot of time to make up you may be allowed to take your holidays before you make up your missed time.
JURY SERVICE
There is a possibility that you may be approached to fulfil this service during your time as a student. Although we acknowledge this experience might well be beneficial to your understanding of the legal system, the possibility that the commitment may extend beyond two weeks is a very real one and as such would interfere markedly with the continuity of the theoretical and clinical experience.
Those who administer Jury Service sometimes allow students in full-time education, including students of nursing / midwifery, to defer of the service. If you are asked to do Jury Service we do have a standard letter which can be sent on your behalf, explaining your current position as a student. Please contact the programme team to ask for a letter requesting exemption from jury service.
THE UNIVERSITY AND SECONDING EMPLOYERS
Students who are seconded to the University from their employer for a programme of study should note the following:
The University will not routinely share information about student progress and attendance with seconding employers. However, circumstances may arise where it is appropriate for information held by the University or the employer, which may affect student progression and continuation on programmes of study or employer support, to be shared between these parties. The University will respond to reasonable requests by employers for such information and may on occasion seek information from employers. Agreement to the sharing of such information for seconded students is a pre-requisite for entry and continuation on programmes of study. Students who wish to be excluded from this agreement should formally notify the Programme Director in writing, who will relay this information to the seconding employer.
INDIVIDUAL PROGRESS AND DEVELOPMENT REVIEW
All students should be offered opportunities to meet with their Academic Adviser, three times during the first semester of their programme and twice in each subsequent semester. Where extended terms operate in the second semester, an additional Academic Adviser session should be arranged. During this meeting issues to be discussed may include:
- Student’s study progress and requirements
- Any supervision and guidance that the student may require
- Placements
- Expectations of the programme
- Attitudes
- Any other items that either the student or the tutor may wish to raise, or
- Particular issues that may be relevant to the continuing success of the student
A summary will be made of the meeting, to be signed yourself and your Academic Adviser, which will then be inserted into your file.
ACADEMIC AWARD & CLASSIFICATION
Following the successful completion of full time study on the programme and the required course units The University of Manchester will award: A Bachelor of Midwifery (Hons) degree, or A Master of Midwifery degree
Degree Classification
BMidwif:
Classification of the BMidwif (Hons) degree awarded will be determined from the marks achieved by the student in all the theoretical and practice-based assessments for level 5 and 6 units. Students must accrue 360 credits in total to be awarded an honours degree (120 credits at level 4, 120 credits at level 5 and 120 credits at level 6). The weighting given to the marks gained within each unit is in proportion to the credit weighting of the unit. The calculation of the classification shall be weighted as follows:
- Year 1 (L4) – 0, Year 2 (L5) – 0.33, Year 3 (L6) – 0.67.
The degree classification is then worked out according to the table below.
Honours Degree Classification:
| I | 70%+ | |
| II(i) | 60-69% | |
| II(ii) | 50-59% | |
| III | 40-49% | |
| Fail | <40% |
MMidwif:
Classification of the MMidwif degree awarded will be determined from the marks achieved by the student in all the theoretical and practice-based assessments for level 5, 6 and 7 units. Students must accrue 480 credits in total to be awarded an honours degree (120 credits at level 4, 120 credits at level 5, 120 credits at level 6, and 120 credits at level 7). The weighting given to the marks gained within each unit is in proportion to the credit weighting of the unit. The calculation of the classification shall be weighted as follows:
- Year 1 (L4) – 0.0, Year 2 (L5) – 0.2, Year 3 (L6) – 0.4 and Year 4 (L7) – 0.4.
Professional Registration as a midwife with the NMC
On successful completion of the programme you will be eligible to register as a midwife with the NMC. In this case successful completion of the programme includes the following:
- Successful completion of all theoretical and practical assessments
- Successful completion of all proficiencies
- Successful completion of all Statutory Clinical Experiences as determined by EC Directive 2005/36/EC of the European parliament and of the Council (2005)
- Completion of all attendance requirements
- Completion of MORA
In order to graduate, you must at least have met the requirements for the relevant academic award, BMidwif (Hons) Degree (360 credits) or MMidwif degree (480 credits).
A personal identifying number will be allocated to each student prior to completion of the course. This number does not permit you to work as a Midwife in any capacity and is purely for communication with the NMC. Details of this will be sent out to you by e-mail. It is the student’s responsibility to ensure that all personal details held on record are correct.
Following ratification of final results at the Awarding Examination Board details of students who have successfully completed the course will be forwarded to the Nursing and Midwifery Council. A Declaration of Good Health and Good Character is signed by the Lead Midwife for Education (or their nominee) and sent to the NMC. The School will receive confirmation that this information has been safely received.
Each student will normally receive a registration pack from the NMC within two weeks of completion information being sent from the School. To be entered on the register, the NMC must have received a completed registration pack from the student and the Declaration of Good Health and Good Character from the School.
It is important that you apply to register with the NMC within five years of your completion date or you will not be able to register with them (NMC, 2019). If you do not register your qualification within five years, you may have to complete a pre-registration programme again. You may apply for jobs before your registration is live but you must be aware that any employment offer will be subject to successful registration. It is the student’s responsibility to liaise with their prospective employer if there is any known delay to registration. Failure to do this may jeopardise your offer of employment.
Non-Completion of the MMidwif Programme
If you elect to undertake the MMidwif, but are unsuccessful at level 7, you will still have the opportunity to qualify for the BMidwif, with eligibility to register with the NMC.
BMidwif (Hons) with eligibility for Professional Registration with the NMC (for those originally intending the MMidwif but do not continue to L7)
Learners must achieve a minimum of 360 credits, which includes 120 credits at each QAA FHEQ levels 4–6. Professional registration as a midwife is only possible when all theory and practice hours are complete (minimum 4600 hours, 50% theory and 50% practice) and all clinical proficiencies are achieved at the end of the third year, level 6. This will necessitate an additional 166 hours each theory and practice to make up the difference between the MMidwif route and the BMidwif route in year 3. Practice hours and achievement of all clinical proficiencies must be demonstrated and theory hours can be achieved through completion of the extra theory delivered on the BMidwif route, including successful application for Associate Fellowship of the Higher Education Authority (AFAHE).
Learners completing the BMidwif programme of study with 300 credits (60 of which must be at level 6) and who do not complete the a unit of study, the practice assessments or hours of study required for professional registration as a midwife will exit the programme with a non-practice award of “BSc Healthcare Studies (Maternal and Fetal)” and will not be able to register with the NMC to practise midwifery.
Students completing the programme of study with 240 credits and who do not complete any level 6 credits may be able to exit the programme with a Diploma in Healthcare Studies (Maternal and Fetal).
Students completing the programme of study with 120 credits and who do not complete any level 5 and 6 credits may be able to exit the programme with a Certificate in Healthcare Studies (Maternal and Fetal).
Completion of Programme
After the final Examination Board meets and agrees the list of completed graduands, pass lists are produced by the Examinations administrator and displayed online for students to access. All successful graduands will be written to confirming their award. Registration for graduation is via an online facility provided by central Student Services.
Students eligible for graduation are encouraged to check the online student system normally 6-8 weeks prior to their ceremony taking place to register their attendance at the ceremony and to request tickets for family/friends.
http://www.studentnet.manchester.ac.uk/selfservice/graduation/
You will receive your Qualification Certificate at the Awards Ceremony (or through the post if you are unable to attend). All queries relating to your Award should be addressed to Student Services (Tel: (0161) 275 5000).
GRADUATION
A person who has passed the degree examination shall be deemed to be a graduate of the University from the date of the meeting of Senate at which the relevant examination result was confirmed. Candidates, who so wish, may be presented for conferment of the degree or diploma at the appropriate ceremony following confirmation of the result.
The names that are printed on the degree certificate will be the student’s name as recorded in the University student record system, which you update each year when you re-register online. It is important, therefore, that you check your record thoroughly to ensure that your name is correctly recorded. The name printed on the degree certificate cannot subsequently be amended without valid proof of the correct name (i.e. birth certificate, passport, etc.) and this service may incur a charge.
5. BEHAVIOUR & PROFESSIONAL CONDUCT
Academic Appeals, Complaints, Conduct and Discipline
Academic Appeals
- For the most up to date information regarding appeals, students should refer to the University’s general support pages, since the pages are updated to reflect changes in policy and guidelines.
- Students have a right of appeal against a final decision of an Examination Board, or a progress committee, or a graduate committee or equivalent body which affects their academic status or progress in the University.
- Students thinking of appealing should first discuss the matter informally with an appropriate member of staff, in order to better understand the reason for the result or decision and to determine whether the matter can be resolved informally by the School prior to making a formal appeal.
- Should you wish to proceed to a formal appeal, this must be submitted within the timeframe outlined in the Academic Appeals Procedure to the Faculty Appeals and Complaints Team electronically by e-mail: FBMHappealsandcomplaints@manchester.ac.uk).
- The Academic Appeals Procedure (Regulation XIX) and associated documents, including the form on which formal appeals should be submitted, can be found at http://www.regulations.manchester.ac.uk/academic/basic-guide-academic-appeals/
Student Complaints
- The University’s Student Complaints Procedure (Regulation XVIII) and associated documents, including a complaints form, can be found at www.regulations.manchester.ac.uk/academic
- The University has separate procedures to address complaints of bullying, harassment, discrimination and/or victimisation – see https://www.reportandsupport.manchester.ac.uk/
- Students thinking of submitting a formal complaint should, in most instances, attempt informal resolution first (see the procedure). Formal complaints should be submitted on the relevant form to Faculty Appeals and Complaints Team electronically by e-mail: FBMHappealsandcomplaints@manchester.ac.uk).
Conduct and Discipline of Students
- General University information on the conduct and discipline of students can be found at https://www.staffnet.manchester.ac.uk/tlso/academic-appeals-complaints-and-misconduct/conduct-and-discipline-of-students/
- Faculty policies for students on communication and dress code, social networking and drugs and alcohol can be found at:
-
- http://documents.manchester.ac.uk/display.aspx?DocID=29038 (Communication and Dress Code)
- http://documents.manchester.ac.uk/display.aspx?DocID=29039 (Drugs and Alcohol)
- http://documents.manchester.ac.uk/display.aspx?DocID=29040 (Social Networking)
-
- Information on Academic Malpractice and how to avoid it can be found at http://www.regulations.manchester.ac.uk/guidance-to-students-on-plagiarism-and-other-forms-of-academic-malpractice/
- In accordance with the Policy on Submission of Work for Summative Assessment on Taught Programmes, ‘All typed summative assessment, including dissertations, should be submitted online and subjected to plagiarism detection software, where appropriate’.
The University Library has produced online resources to help students in avoiding plagiarism and academic malpractice at: https://www.library.manchester.ac.uk/training/my-learning-essentials/online-resources/
An Introduction to Referencing and Avoiding Plagiarism is provided by the Student Guidance Service at:
An Introduction to Referencing and Avoiding Plagiarism (Student Guidance Service)
The Student Support website provides guidance on Good Study Skills at:
https://www.studentsupport.manchester.ac.uk/study-support/goodstudyskills/
The Student Support website also provides guidance on avoiding academic malpractice: https://www.studentsupport.manchester.ac.uk/study-support/academic-support/assessments-and-exams/avoiding-academic-malpractice/
You are expected to behave in a professional manner when within the University premises. Any student demonstrating inappropriate behaviour may be asked to leave the premises and may be referred to the Occupational Health Department or to the Fitness to Practice / Health & Conduct Committee.
You are expected to behave in a professional manner when on placement. Any student demonstrating inappropriate behaviour may not achieve their holistic assessment, may be asked to leave the placement and will be reported to the University, which will be investigated by a Concern Review Panel and may result in referral to the Fitness to Practice committee.
Inappropriate behaviours include being under the influence of alcohol or illegal drugs, being rude or aggressive to fellow students or staff, smoking in restricted areas or putting students’ or staff member’s health and safety at risk.
A Fitness to Practice Committee may decide to prevent students from proceeding to the next year of study if:
- the student has not behaved in accordance with the principles of the NMC The Code: Professional standards of practice and behaviour for nurses and midwives1 or
- the student’s health would prevent them from fulfilling the NMC’s The Code: Professional standards of practice and behaviour for nurses and midwives6
- the student does not uphold the NMC’s The Code: Professional standards of practice and behaviour for nurses and midwives6
See also: Dignity at Work & Study and Regulation XVII Conduct & Discipline of Students and Supporting Trans Staff and Students at the University.
BEHAVIOUR AND PROFESSIONAL CONDUCT
You are expected to behave in a professional manner at all times when in practice. Should you demonstrate inappropriate behaviour you may fail your skills assessment or be asked to leave the learning environment. Your behaviour will be reported to the University. You may then be referred to the Occupational Health Department or the School or Faculty Fitness to Practice Committee.
Inappropriate behaviours include (but are not limited to); inappropriate use of social media (see University guidance and policy on social media use), being under the influence of alcohol or illegal drugs, being rude or aggressive to fellow students, staff or service users, smoking in restricted areas or putting students’ or staff member’s health and safety at risk.
If, during the programme you receive any police convictions, cautions or “bind-overs” you should discuss this immediately with your Academic Adviser for support and guidance. You will also be asked to complete the on-line good health and good character form each year.
Please also refer to The Code (NMC, 2018) for guidance on professional conduct for nursing and midwifery students, available at: https://www.nmc.org.uk/globalassets/sitedocuments/nmc-publications/nmc-code.pdf.
See also: Behaviour & Professional Conduct
Dignity at Work and Study
The University seeks to create a study environment which is free of harassment and which protects the dignity of all students irrespective of sexual orientation, racial or ethnic background, religion or disabled status. It regards sexual, racial or personal harassment as most serious and requires all students to observe its policy in this area. Personal harassment takes many forms. It is uninvited and unwanted actions which cause offence and/or embarrassment, fear, stress or tension. It can be an isolated act such as a comment or wilful gesture, or it can take the form of repeated behaviour against a person.
In cases where a complaint of harassment is substantiated, the individual responsible may be subject to disciplinary action under General Regulation XVII (Conduct & Discipline of Students).
The University Policy Statement on Dignity and Work and Study for Students is available in the A-Z of Student Services. This document contains details of the University Resources, policies and procedures and will be given to all students at registration. If you prefer to access the full university policy on-line it is located at the following web address University Policy Statement on Dignity and Work.
Confidentiality
By the nature of nursing and midwifery, you will be exposed to confidential information about patients/clients and others. Breaching confidentiality may only be appropriate in exceptional circumstances. Inappropriate breaching of confidentiality is a betrayal of trust and is a serious matter and as such may lead to disciplinary action. All students will undertake education and training in Data Protection and Information Governance via the University and our practice partners. Any breach of information governance will result in disciplinary action for the student.
All student nurses and midwives are expected to abide by the NMC code (NMC 2018) which covers issues of confidentiality.
You must not give information to the Press regarding events which take place in the Division or any of the placement areas. Any enquiries from the Press must be directed to the Chief Executive or the Senior Officer (if in a clinical placement) or Head of School.
If you are requested to make a statement for the NHS Trust or for the NMC, help and advice should be sought from your Academic Adviser as soon as possible.
Regarding Confidentiality in Assessments please refer to the exams and assessments area on the Blackboard Study Gateway.
STUDENT UNIFORM POLICY
Introduction
Wearing a uniform is essential to project a smart, professional image in the workplace. Nursing and Midwifery students of the University of Manchester are required to be well presented at all times in the clinical area. They are not only representing their profession, but also the University. Patients and clients can be assured of your commitment to best practice in infection prevention and control if your uniform is clean and you dress according to appropriate standards.
Most Trusts that you are likely to work in will have their own uniform or dress code and you are required to strictly adhere to those policies, in addition to the Division’s policy.
The policy below (and available on Blackboard) applies to all Nursing and Midwifery students who undertake placements organised by the Division. This policy supplements the Communication and Dress Code for Students in the Faculty of Biology, Medicine and Health at The University of Manchester.
Failure to comply with the uniform policy will be regarded as unprofessional behaviour and steps will be taken to invoke the Division’s procedure regarding discipline if necessary.
University of Manchester Student Midwife Uniform
You will be provided with a maximum of three complete sets of uniform by the University at the beginning of your programme of study as follows:
- White dress with purple trim and University Logo
Or
- White tunic with purple trim and University Logo and navy blue trousers
Replacement Uniforms
‘Alexandra’ is the only University approved supplier for University of Manchester student Nurse/Midwife uniforms.
You can purchase additional sets of uniform from the University suppliers at the same cost as paid by the University at the time of ordering.
Additional uniforms can be ordered and purchased by students from the supplier at the time of initial ‘fitting’ and any replacement/additional uniforms subsequently required can be ordered via the supplier website using the unique code you can obtain from shs.placements@manchester.ac.uk . You are responsible for the costs of any additional and/or replacement uniforms, and any additional delivery costs. Instructions for setting up your account and ordering replacement uniforms are available in the BMidwif Gateway.
You must only use the University approved supplier for any additional or replacement sets/items of uniform as these are supplied to a strict specification in line with relevant local and national guidance.
You will be provided with a University name badge bearing your full name, designation (student nurse or student midwife) and the logo of the University of Manchester. These must be worn at all times as part of the uniform in addition to any badge provided by the placement provider.
Replacement University name badges can be ordered from the Programme Support Office, G.319 Jean McFarlane Building.
Where this Policy Applies:
When in placement in clinical / community environments you must wear your University of Manchester uniform at all times whilst at the placement.
Due to the nature of work and specific patient/client groups they serve, some Trust staff will in some clinical areas wear their own clothes. In these instances, you will be required to wear your own clothes but these must be appropriate to the work environment, look clean and smart and adhere to any local policies.
Plain, appropriate clothing must be worn and no advertisement logos or slogans should be visible.
University uniform must also be worn when undertaking any clinical skills training sessions in the University or in the Trust. This includes any training undertaken in the clinical skills laboratories at the University such as moving and handling and basic life support training and update sessions.
You must not, as far as possible, wear your uniforms outside of the placement area and must change into your own clothes upon completion of a shift. When working in community you should wear a coat that covers the uniform entirely. The Department of Health advises that the public do not like to see hospital staff in uniform away from the workplace because they may perceive this as a risk to hygiene and infection control in the workplace. COVID infection control measures may also prohibit staff travelling in their uniforms.
Uniform Appearance and Care
A clean uniform must be worn for every new shift. You are responsible for washing and ironing your own uniforms. The Department of Health recommends that uniforms be washed at a minimum of 60° Celsius for at least 10 minutes which is sufficient to remove most microorganisms. Uniforms must look clean and neat at all times. If an item gets stained or damaged then a replacement must be obtained as soon as possible (see above for how to obtain replacement or additional uniforms).
Adjustments to the uniform for cultural / ethnic or religious reasons will be considered where possible but must be in line with national and local policies. In relation to the University supplied items of uniform, adjustments to sleeve length are not offered. Any student wishing to wear long sleeves for religious reasons will be required to purchase their own under garments / disposable sleeves.
Black headscarf / turban / skull cap may be worn.
The correct size of uniform must be worn and students must not wear cardigans or other over garments in the clinical areas.
Appropriate shoes must be worn. These must be black, flat, full shoes not boots, which cover the entire foot, have a non-slip rubber sole, and be plain (not suede or canvas). It is not acceptable to wear any other type of shoe.
Tights that are black or skin coloured only may be worn, with no embellishments. Only plain black socks may be worn.
Whilst on placements the following will also apply:
- Hair must be tidy and long hair must be tied/clipped back off the face and collar. Protruding hair decorations must not be worn. If required, neutral colour decoration should be used to secure hair.
- Long hair should be firmly tied back in such a way as not to interfere with duties or patient care.
- Beards and moustaches should be neatly trimmed.
- Fingernails should be clean, short and free of all nail polish. Acrylic nails must not be worn at any time due to the risk of infection (McNeil 2001)
- If make-up is worn, this should be discrete and false eyelashes are not acceptable. Perfumes and after-shave should be used sparingly.
- In the interest of infection control and minimising risks to the student and the patient/client NO jewellery other than small, plain stud earrings (one per ear) and one plain band ring is permitted at any time whilst wearing uniform. Wristwatches and bangles must not be worn when attending to patients.
- Any visible piercings must be removed whilst in the clinical area and / or treating patients or clients.
- Tattoos that may cause offence should be covered accordingly and should adhere to the required dress code described above.
References:
McNeil S.A, Foster C.L, Hedderwick S.A (2001) Clin Infect Dis 32:367-372 Department of Health (2007) Uniforms and Workwear. An evidence base for developing local policy. © Crown Copyright 2007 [online: (Local Uniform Policy)
CLINICAL SKILLS LABORATORY: STUDENT CONDUCT
You must follow the regulations below when using the laboratories:
- Aspx (manchester.ac.uk) (Social Networking)
- http://documents.manchester.ac.uk/display.aspx?DocID=29038 (Communication and Dress Code)
- Faculty of Medical and Human Sciences (manchester.ac.uk) (Drugs & Alcohol)
HEALTH CLEARANCE
Continuation on the programme is conditional on continued health clearance: see Occupational Health clearance.
You are expected to be proactive in managing both physical and psychological health issues and seek support from your Academic Adviser or self-refer to Occupational Health if you have any concerns about the impact of health issues on your ability to study.
It is your responsibility to attend agreed health screening, referral and immunisation appointments and specifically to securely retain the vaccination history information provided by Occupational Health at the end of the course of vaccines. Occupational Health recommends that no student commences on clinical placement until they have had an initial health screening appointment. You are encouraged to advise Occupational Health if you have any significant health related concerns that could affect your fitness to for the programme.
The programme team will be keen to support you manage any health issues. You have a professional responsibility to engage with occupational health processes in order to “maintain the level of health you need to carry out your professional role” (NMC 2018). Failure to do could result in a referral to a Fitness to Study or Fitness to Practice Committee.
Crisis counselling is provided by the Universities Counselling service however Occupational Health can offer support and advice with regards fitness to return to the programme.
Occupational Health will advise the Division if you do not attend a formal appointment and this may impact your progression.
Please note that the Universities Counselling and Mental Health services offer confidential help with any personal issues affecting work, self-esteem, relationships, sexuality, mental health and general well-being. See also: https://www.counsellingservice.manchester.ac.uk/.
If you have a disability or an issue such as Dyslexia, Dyspraxia, Dyscalculia then the Disability Advisory & Support Service [DASS] would welcome you registering for advice and additional support. See also: https://www.dass.manchester.ac.uk/
GOOD HEALTH AND GOOD CHARACTER
You must declare any criminal convictions, cautions, reprimands or warnings received (either in this country or overseas) that may call into question your good character as soon as possible, as this may impact your continuation on the programme. For each year of your studies, you will be required to complete an annual self-declaration of Good Health & Good Character confirming your continued good character.
PART-TIME EMPLOYMENT
You are advised to think carefully about how you will balance work in theory and practice against the demands of part-time employment and to limit any hours they work accordingly. The Division is not able to provide character references for part-time employment undertaken during a programme of study, but will provide details of your programme of study.
If however you do have a part-time job in a particular clinical area, please inform the allocations department. We recommend that you do not have a clinical placement in the same area as your part-time job, due to the conflict of interests which may arise.
UNIT EVALUATIONS
Since we are encouraging you to develop your willingness and ability to ask searching questions about midwifery practice, we expect you to offer equally appropriate criticisms of our work in midwifery education. In this respect, we agree to accept your evaluation of our work. You, as new midwives, carry forward our aspirations, and you will help to assure the on-going development of midwifery education.
6. STUDENT SUPPORT
Student Support and Wellbeing Team
The Student Support and Wellbeing Team can support your wellbeing needs through the year. The team is here to support you when you wish to discuss circumstances such as interrupting your studies, financial issues, the submission of details of mitigating circumstances and any personal concerns that are affecting your ability to study and engage fully with your course. It is important to point out that Student Support is not a counselling service; it is a practical support service.
Support from the University
As a student at the University of Manchester, you have access to a huge range of support services and resources. This includes, but is not limited to, support relating to your studies, finances, health and wellbeing, settling in and making friends, personal safety and planning for your future beyond University.
Students’ Union Advice Centre
The Students’ Union has advisers who can help with any matter ranging from finances to housing and beyond. The Advice Centre is on the first floor in the Student Union Building, and is open Monday to Friday, 9.30am to 4.30pm, term time and vacation. See http://manchesterstudentsunion.com/.
Support of care experienced and estranged students
The University of Manchester recognises that care experienced students, and those that become estranged from their families often require additional support. This may take the form of, amongst other things, financial support, help with accommodation, provision of quiet study are as and general support. Please contact shs.wellbeing@manchester.ac.uk for further details on how to access support.
Support for Students with Disability and Long-Term Health Problems
If you have a disability, or have learning support needs, we advise that you register with the Disability Advisory and Support Service (DASS). They can offer a range of services to help you make the most of your University experience. Where appropriate, they will work with you to develop a support plan which will put in place any support you require for exams, from the library or from teaching staff.
Registering with DASS is particularly important for students where ongoing or recurring difficulties may impact their academic performance. The University’s Policy on Mitigating Circumstances (see section 6) does not allow students to make repeated claims for the same condition, because to qualify for mitigation, the circumstance must be ‘unforeseeable’. However, the Mitigating Circumstances Committee can award further mitigation where DASS support your claim; for example, by advising the committee that your condition is associated with ‘flare-ups’ (which are unforeseeable).
You find more information and how to register with DASS here: http://www.dass.manchester.ac.uk/
Support for International Students
Manchester has a thriving International student community and you will have lots of opportunities to engage with students from all over the world. The International Society (http://www.internationalsociety.org.uk), based on Oxford Road, organises trips, events, activities and community projects which are open to both International and British students. The Language Centre also provides support to International students who have concerns about their English skills (http://www.languagecentre.manchester.ac.uk/).
UoM Counselling Service
The Counselling & Mental Health Service works in partnership with other support services within the university and are here to provide support for you should you feel you need help with your mental health.
The Counselling & Mental Health Service offer a range of workshops, groups, 1-1 appointments and other resources to help you. For more information and to book an appointment click here: Get Help
You can also phone for advice on 0161 275 2864 between 9.00am – 4.30pm (Monday – Friday).
Student Support and Wellbeing Contact Details
shs.mitcircs@manchester.ac.uk – for information and guidance on mitigating circumstances and extensions, including sending evidence and receiving outcomes of applications.
shs.attendance@manchester.ac.uk – for queries related to attendance monitoring.
shs.wellbeing@manchester.ac.uk – for support and signposting to university wellbeing resources, as well as making a wellbeing appointment with an advisor.
shs.dc@manchester.ac.uk – for Disability Advisory and Support Service (DASS) enquiries.
OCCUPATIONAL HEALTH
Web: http://www.occhealth.manchester.ac.uk/
Email: waterlooocchealth@manchester.ac.uk
Tel: 0161 275 2858
On-going support for all students is provided by the Occupational Health Department. The aim of the service is to promote the health and wellbeing of all students and the prevention of illness and injuries at work. This is achieved by ensuring students are offered at commencement an initial health screening appointment where key health related information is provided and appropriate immunisation provided.
CAREERS SERVICE
Web: http://www.careers.manchester.ac.uk/
Email: careers.info@manchester.ac.uk
Tel: 0161 275 2829
The Careers Service aims to improve the employability of students by providing them with key skills and knowledge. To help students formulate and implement well-informed choices about their careers they deliver and manage numerous services, projects, courses and events. The Careers Service work in partnership with colleagues across The University of Manchester and with organisations across the UK.
STUDENT REPRESENTATION AND FEEDBACK
Each programme will choose a number of student representatives at the start of each academic year. You will be able to apply for this role, and will be informed of who is chosen so that you can feed back any issues or areas for improvement you may have identified within your programme.
The representatives are invited to the Staff Student Liaison Committee, where they can feedback anything which they have heard from their fellow students. The Programme Team then respond to these, and these responses and any action taken are fed back to staff and students via a newsletter.
Role of a Student Representative
The role of student representatives is to represent the views of students on a particular course to the academic staff at various meetings of the Division. This ensures that students have a voice and are participating in developing learning and teaching within the Division. Responsibilities include:
- Identifying student issues and needs. When necessary referring them on to the relevant people who can assist them.
- Providing another layer of support for new and existing students.
- Attending and participating in various meetings held at the University.
- Consulting, involving and reporting to students.
- When arranged, attending Student Representative training sessions.
- Providing a link between the staff and students at the Division.
- Keeping informed of developments within their programme of study.
- Promoting equal opportunities.
- Contributing to the growth and development of the Staff Student Liaison Committee by providing ideas and suggestions.
Benefits of Being a Student Representative
By committing time and effort student representatives reap many benefits and develop transferable skills. These include:
- Increased involvement in their educational experience at the Division. Knowing that students can make a positive impact on the lives of present and future students.
- Involvement in an extra-curricular activity.
- The opportunity to meet other students across the Division and University.
- Representation and advocacy skills.
- Listening and communication skills.
- Organisation and time management skills.
- Negotiation skills.
- A certificate from the Division to evidence the activity in professional profiles.
The Division also benefits through:
- Consultation with students.
- The opportunity to improve the quality of its courses and student satisfaction.
- Enabling students to understand the Division’s policies and processes.
- Promoting an increased sense of belonging to the Division amongst students. Having an active staff-student dialogue outside of the realms of teaching.
Meetings to Attend
All representatives will be required to regularly attend the previously mentioned Staff Student Liaison Committee which discusses cross-programme issues and is held five times per academic year (the first meeting is a student representative training session).
In addition, representatives attend their own Programme Committee. Programme Committees are responsible for the review procedures of their respective programmes. The Programme Committee manages programme development, assessment of individual units, student related matters and any other matter relating to the Programme. Each Programme Committee has student representatives from each year group.
Representatives may also be invited to participate in other committees, working groups, workshops and reviews related to academic programmes. Cohorts and years should have representation at all meetings. However, as there will be several representatives for each year /cohort you are encouraged to work as a team to facilitate this.
Although student representatives will receive an authorised letter of exemption (from lectures and clinical areas) to attend them, it is understood that as students it is not possible to attend all meetings. Therefore, apologies can be emailed a week in advance of the meeting, including any issues, ideas/suggestions that can be read to the meeting. Email is the main mode of communication between student representatives and University staff.
National Student Survey
In the final year of any undergraduate programme, you will be invited to complete the National Student Survey (NSS). This independently administered survey asks for your feedback on your whole degree, as well as your broader University experience. The results are published to help prospective students make informed decisions about where and what to study. The NSS also provides us with useful data for benchmarking ourselves against other universities.
PEER ASSISTED STUDY SESSIONS (PASS) AND PEER MENTORING
All first year students are placed in a PASS group which is led by two leaders who are current year 3 students. PASS utilises the experience and expertise of the higher year, volunteer students (PASS Leaders) who have been trained as facilitators, not teachers or tutors, to support their group of students in finding solutions to their problems themselves, through discussion and guided questioning.
PASS leaders will introduce themselves to their group through activities in Welcome Week and continue to support their group throughout the academic year in a series of compulsory timetabled sessions. The agenda for the sessions is led by the group who indicate to the PASS leaders the topics and /or skills that there would like to be addressed. The leaders then plan interactive tasks and activities. The PASS leaders are supported by the Student Support Manager and the Year 1 lead. Information on PASS can be found in the Student Support pages on Blackboard or by contacting sso.intern@manchester.ac.uk.
Optional peer mentoring groups for year 2 students may be offered by 3rd year students in Semester 1 to support the 2nd year students as they settle into year 2 and adjust to their new NHS Trust sites.
7. LEARNING RESOURCES
LIBRARY FACILITIES
The University of Manchester Library consists of the Main Library, Alan Gilbert Learning Commons (AGLC), and several site libraries, and provides you with the resources and support you need throughout your BMidwif/MMidwif programme. The two most relevant locations for you are the Main Library and the AGLC. The Main Library houses all of the essential text books whilst the AGLC provides a 24/7 learning environment.
As the third largest academic library in the country, and one of only five national research libraries, the Library has an extensive collection of resources, including eBooks, databases and journals available online.
The ‘My Home’ tab in MyManchester contains your library summary, including current loans, reservations and charges and links to the resource bank. Other Library services can be access via ‘My Learning’ within MyManchester.
Getting Started
You will need your student card to access all library sites around campus. Many of our services and resources also require you to confirm that you are a registered student. This authentication can be your student card, the ID number on the card, your Library PIN, the central username and password you use to log on, or a combination of these.
There is a subject guide for Nursing and Midwifery students giving all of the latest information on resources and services available to you. This is a good starting point if you are looking for any library resources or information related to your course.
My Learning Essentials is the name of the Library’s study skills programme. As part of this programme we provide face-to-face workshops and online tutorials covering a wide range of subjects from presentations skills to referencing.
Each course module in Blackboard includes an online reading list, so you can quickly check availability and directly access e-books, digitised chapters and e-journals or articles.
The Main Library
The Main Library holds the principal collection of Midwifery books and journals. Midwifery textbooks are located on Floor 2 of the Blue Area, together with books in other related subjects. Midwifery journals held in print are on Floor 1 of the Green Area in the Clinical Sciences sequence; further relevant periodicals are shelved in other areas of the Main Library. Library Search is the name of the Library’s catalogue. You can use Library Search to find out what items are available and where to find them, including eBooks and online journals. One of the great features of Library Search is that you can search down to the article level in journals (and databases) without having to go to the journal homepage.
The Main Library offers group study rooms, individual study space options and computer clusters. Wi-Fi is available throughout the building and a cafe lounge can be found on the ground floor. The Library has long opening hours and extends these during exam periods. Please check Locations and Opening Hours for full details on opening hours and facilities.
The Alan Gilbert Learning Commons
The AGLC is a state-of-the-art learning environment with 24/7 opening hours throughout term-time. The Learning Commons has flexible open learning spaces with multimedia facilities, computer clusters and 30 bookable group study rooms with whiteboards and media screens.
IT FACILITIES
IT Services and E-Learning
Details of what IT support is available and how to access it can be found on the FBMH eLearning Support page.
Login to the Support Centre online to log a request, book an appointment for an IT visit, or search the Knowledge Base.
Telephone: +44 (0)161 306 5544 (or extension 65544). Telephone support is available 24 hours a day, seven days a week.
In person: Walk-up help and support is available at the Joule Library, Main Library or Alan Gilbert Learning Commons
Use Support Centre online for support with eLearning, from where you may make a request or search the Knowledge Base.
For IT and eLearning support visit: https://elearning.bmh.manchester.ac.uk/student/technical-support/
University Computer Facilities
Students at the University have access to a wealth of resources including research support services, PC clusters, email and Internet access, wireless access, Microsoft applications, printing facilities, network document storage, student portal, eLearning environment and the extensive electronic resources managed by The University Library.
As a new student you will be introduced to the University’s IT facilities at your induction. In addition to your Faculty and Division IT provision, you will find IT facilities in areas of high student use, such as Jean McFarlane Building (George Kenyon cluster), John Rylands Library and the Joule Library. The two libraries also house the IT Service Desks where you can get help and information.
You will find the most up-to-date information about IT services on the IT Services website. Packed full of information, the website provides details of the services available to users including useful information about day-to-day help and support and information about protection from the latest viruses etc. We recommend you visit the ‘Getting Started’ section of the site first.
University PC Clusters
The University’s Public PC Clusters are available for any staff or student to use. Operated on behalf of the University by the IT Services division, they are present at various locations on campus and also in some Halls of Residence. Opening times for each cluster will vary but at least one cluster operates 24/7 and two clusters operate extended opening times including weekends.
Some clusters will be booked for teaching and learning purposes at various times, therefore you are advised to visit the website:
http://www.itservices.manchester.ac.uk/pcclusters/pcclusterlocations/ or the Central IT Service Desk for the latest opening times and PC Cluster information.
Online Skills Training Resource
The Faculty has developed a skills training resource to support you through your postgraduate taught programme. This online material should supplement the assessed learning material and activities undertaken in your taught programme.
Accessing the online skills resource
You can access Blackboard through the My Manchester portal (http://my.manchester.ac.uk). The skills training resource is available in an academic community space available to all registered PGT students in the Faculty through Blackboard.
If you cannot see these units in your Blackboard, please contact your Programme Administrator.
Content
Full details of all these resources can be found in the introduction to each unit. These resources have been designed to give you formative feedback on your progress through them. If you experience any problems and would like to talk to someone, please contact your Programme Director. If you have questions about referencing and how it applies to your own work, please contact your Programme Director or dissertation supervisor/module lead.
| Research Methods* | This course is spilt into 2 units that cover introductions to study design and dissertation skills. It has a number of online quizzes where you can test your knowledge. |
| Introduction to Statistics* | The course provides a valuable foundation for understanding and interpreting biostatistics. It aims to provide you with the fundamentals of quantitative analysis. |
| Presentation Skills | This short interactive unit is designed to help you enhance your presentation skills. Regardless of whether you are presenting in public, preparing for conferences, an oral examination or more informal settings this unit will give you the tops tips to improve your delivery. The course also includes a unit on influencing effectively, alongside the presentation and poster information. |
| Qualitative Research Methods* | This unit has been designed to give you an introduction to Qualitative Research. |
* NOTE: the material in this online resource is for reference and formative learning purposes only. In some of your taught programme you may be required to undertake assessed course units for Research Methods, Qualitative Research or Statistics. If your programme involves taught units then you should refer to the Blackboard material relating to that course unit. Please contact your Programme Administrator if you are unsure which material relates to your assessed work. You will still be able to refer to the online skills resource in later years.
Student IT Support Helpdesk
Tel 0161 306 5544
E-Mail: it-servicedesk@manchester.ac.uk
Divisional Computer Facilities
Computing facilities for the Division are available on the 2nd floor of the Jean McFarlane Building.
The facilities provided have healthcare specific applications and there are 40 computers. Students can access the full range of online resources available including Blackboard and the University Library electronic resources.
Printing has to be paid for, via print credits purchased from the Manchester Computing Shop or print robots situated around the University’s campus.
Access to the computers is via a standard University username which is obtained from any of the main campus computers displaying the standard log in screen or from the registration computers at Jean McFarlane Building, by answering the questions when prompted students can gain access to and receive their username and password. This will enable them to use any of the computers to which any student has access.
STUDY SKILLS
Each student will start their programme with a mix of different skills. We have identified a number of Study Skills that are vital for you to master early in your study, in order to achieve your full potential on the programme. These include academic writing, Harvard Referencing, Using IT software, Numeric and Literature skills.
Each programme of study will provide an introduction to relevant study skills during enrolment. In the BMidwif, these are part of the Professional Midwifery Unit with relevant activities located on Blackboard. You are also strongly advised to access the ‘My Learning Essentials’ resources via the library website. These offer a wind range of resources and workshops to help you develop your skills. If you feel that you may have a learning disability further assistance may be available, please see your Academic Adviser or the Disability Support Officer.
SOCIAL & WORKING SPACES FOR STUDENTS
The Jean McFarlane Building has a central atrium which provides comfortable and flexible spaces for students to meet or work. Wi-Fi is available in the atrium.
Work spaces may also be booked via the Library and within the Alan Gilbert Learning Commons building. There are many computer clusters available for use across the campus.
The use of all these facilities may be restricted depending on government and university guidance regarding the COVID pandemic.
8. APPENDICES
APPENDIX 1: DIVISION OF NURSING, MIDWIFERY & SOCIAL WORK
STUDENT CHARTER AND CONDITIONS OF PRACTICE EXPERIENCE
  |
Conditions of Practice Experience
The University of Manchester Student Charter has been developed jointly by the University and the Students’ Union; the Division of Nursing Midwifery and Social Work endorses this charter. It establishes clear and mutual expectations for the experience of all students: undergraduate, postgraduate taught and postgraduate research. It sets out what you can expect from the University and what the University expects of you as partners in a learning community under the following headings:
- Our learning environments
- Personal and academic development
- Communicating and interacting with each other
- Respecting and valuing each other
- Being part of our community
As a health/social care student you will have additional responsibilities under the heading of Developing Professional Practice. These responsibilities to service providers and users are detailed in the Conditions of Practice Experience below.
Conditions of Practice Experience:
You should apply the guidance given by your professional body at the links below in both your academic and practice work and behaviour:
- NMC Code of Conduct – The Code (nmc.org.uk)
- Standards of conduct, performance and ethics – nmc-old-code-2008.pdf
- Standards of Proficiency – Social Work (Standards of proficiency for registered nurses – The Nursing and Midwifery Council (nmc.org.uk) )
Developing Professional Practice
Together we will:
- be guided by the University’s and Providers’ policies and procedures
- perform all activities with guidance from and reference to the standards of professional bodies and current and relevant legislation in order for you to become a professional who is fit for award, employment and purpose
- ensure a safe environment where there is respect and dignity, and within which it is possible to raise and escalate concerns encountered during the practice experience in a timely way
- provide opportunities for you to develop your evidence base for practice where this is required
As a student I will:
- Maintain my health and good character by ensuring that I:
- attend all required Occupational Health Service appointments
- notify the Division of any situation which might result in the receipt of a police reprimand, caution or conviction
- complete the annual declaration of Good Health and Good Character
- ensure I access all learning environment information in a timely way and contact my practice experience provider before the placement begins
- engage with the activities of the learning environment under the supervision and guidance of an appropriate member of the provider’s staff
- maintain confidentiality with all forms of information I may have access to, see or hear
- ensure I present myself professionally at all times taking note of any regulations relating to uniform and personal appearance
- ensure I complete all patient/service user documentation in a timely, accurate and understandable way and obtain a staff signature where it is required to do so
- understand that my practice documentation is my responsibility and ensure it is available to practice area staff when I am there
- liaise with my Practice Assessor / Supervisor(s) to ensure that any practice experience documentation is completed in an honest, timely and appropriate way
- submit all practice documentation following University guidelines and deadlines
- engage in the assessment/feedback processes designed to support my practice development
- take part in evaluative processes which facilitate the development of practice experiences for all students take responsibility for my personal money or property whilst on Providers’ premises
- communicate appropriately with my academic assessor and academic adviser regarding any issues I am experiencing in practice and respond to requests to attend meetings regarding my progress
As a University, and in negotiation with Providers, we will ensure your practice experience:
- is prepared and audited in line with professional and University guidance
- has sufficient appropriately trained staff to support your development of practice-based skills
- is appropriate to your stage in the programme
- is communicated to you within the timeframe set out by the University
- is supported by allocations procedures to ensure your practice experiences facilitate development of your professional practice
- provides you with a supportive framework to resolve any challenges you may encounter I acknowledge that I have read the Student Charter and the Conditions of Practice Experience and agree to fulfil my role as laid out in these documents.
| Student | Academic Adviser |
| Name | Name |
| Signature | Signature |
| Date | Date |
APPENDIX 2: GUIDANCE ON MANAGING ATTENDANCE AND ABSENCE REPORTING
Our NMC validated curriculum (NMC 2018) requires student to complete 100% of their clinical hours and academic learning hours in order to meet the requirements for registration as a midwife and to develop skilled and knowledgeable midwives. Students who engage well with the learning materials and opportunities provided tend to do well in their studies and their professional development.
In accordance with the ‘University of Manchester Policy on recording and monitoring Attendance’ (UoM 2014), the programme has a policy of recording, monitoring and responding to attendance and engagement issues, with the aim of assisting students to access appropriate support with issues affecting welfare and attendance so they are able to meet the attendance requirements of the programme or to recognise when this is not achievable.
In line with the University policy, if a student does not manage to comply with the required steps to improve their attendance, the Examination Board may refuse them permission to proceed on their programme. The student would have the right to appeal any such decision and would be notified of the timeframe for this process.
As completion of the whole programme is required (NMC 2009), students who have outstanding theory or practice attendance requirements at the end of the final year will need to continue on the programme until all hours (theory & practice) have been completed. The student will need to arrange funding to support them during this extra time. Students will be encouraged to make up missed time within each academic year to avoid building up a large amount of ‘making up time’ using the ‘making up time in practice policy’ and ‘making up theory time policy’.
Recording attendance and engagement
Instructions for students
- For synchronous (live face-to-face or online) sessions, which you must attend at the stated time. Unless instructed otherwise by your lecturer, it is your responsibility to register yourself as present at all activities
- It is your professional responsibility to complete all asynchronous (or not live) theory sessions, such as online activities, pre-recorded lectures, and guided reading. These are timetabled to assist you in pacing your studies and to help you prepare for future live theory sessions, simulation, or assessments, hence it is strongly recommended that you complete them on the day they are set.
- Engagement with asynchronous activities and the unit overall may be periodically monitored via quizzes or online tasks.
- Students who fail to confirm their attendance at a synchronous session MUST complete a Missed Teaching Form (MTF) to evidence their learning and send this to their unit Unit Lead (UL).
- Links to all forms, including MTFs are available in Blackboard (BMidwif Student Gateway; Forms and Uniforms folder).
- The UL may wish to discuss MTFs with students before signing off the learning and they will let students know if this is the case; once signed off the deficit in hours will be removed from the student’s non-attendance record.
- Students who are struggling to meet the attendance requirements are strongly advised to discuss this with their Academic Advisor.
- Students should not approach the programme administrator to request additions to the register.
Missed Teaching Forms
Missed teaching can be ‘made up’ using the missed teaching form. The student must provide evidence of how they have engaged with the material. Where possible, podcasts and recordings are available in Blackboard to facilitate this process.
IMPORTANT: Missed teaching forms should be submitted by e-mail to the Unit Lead along with any appropriate evidence; the Unit Lead update the record.
Sessions that cannot normally be made up through private study may include:
- Skills lab or practical sessions.
- Tutorials/seminars involving discussion and interaction
- Inter-professional learning activities involving discussion & interaction
- Special events.
Missed Teaching Forms should clearly indicate the session being made up, the date and nature of the session, the number of attendance hours missed and being made up and the work that has been done to catch up the missed material.
Examples of acceptable evidence include:
- Annotated PowerPoint handouts indicating that the student has listened to the podcast and engaged with the material
- Own notes relating to the topics covered in the session.
- Annotated additional reading relating to the topics covered in the session
- Completed quizzes or activities given out in the session.
The amount of evidence required should be in proportion to the length of the session. Lectures may decline to sign the missed teaching form if the work submitted does not indicate that the student has engaged with the material, eg if the student has simply cut & pasted the lecturer’s PPT slides into a word document.
Forms should be presented in the same year/semester that the unit is being taught. Lecturers may decline to sign missed teaching forms presented outside this period. Students should aim to have all missed sessions from the academic year caught up by the end of the academic year.
Students are expected to make up missed theory time through theory-related activity. Attendance at some optional sessions or conferences can be accepted as an alternative way of making up missed theory learning – see Attendance at Conferences Policy on Nursing Gateway.
Attendance at compulsory NHS Core skills practical sessions
Some practical sessions may be identified as compulsory (ie required in order to be allowed in practice or to continue in practice). These will include sessions linked to on-line NHS Core Skills which are also compulsory. One repeat session can be arranged for those who did not attend. Failure to meet the requirements for attending placement will result in being withdrawn from placement until this can be achieved.
Students will need to seek an alternative opportunity to complete the skills session eg accessing a session in the Trust or joining a different year group or a BNurs group.
Making up missed practice hours
Please see the BMidwif making up practice hours policy on the Practice Learning Gateway
Reporting the reason for absence If no reason for absence has been given, the absence will be recorded as ‘unauthorised’. Students should therefore indicate the reason for an absence of up to 7 days (theory or practice) in the following ways:
- On all occasions, email attendance@manchester.ac.uk or bmidwifery@manchester.ac.uk
- Contact the lecturer/unit leader as a courtesy to let them know you will be absent and provide a brief reason for the missed the session.
- Email their Academic Adviser to keep them informed and to discuss any difficulties they are experiencing which are affecting their ability to attend.
- If missing a practice day, the student should contact the placement area to notify their mentor/ward manager/team leader that they will not be attending and also contact their academic adviser to let them know they are not attending.
Absences due to sickness more than 7 days should be certified by a sicknote, fitnote, Dr’s letter or an Occupational Health letter. A copy should be emailed to the Academic Adviser and copied to the programme administrator.
Authorised absences can be agreed by the Academic Adviser. These can be agreed in response to significant personal difficulties, for a period up to 3 weeks. Please note, this time will need to be made up in order to meet the NMC completion requirements.
Students must not arrange holidays during term time. These are always classed as unauthorised absence. Taking unauthorised leave may result in a referral to the Fitness to Practice / Health & Conduct Committee.
Monitoring sickness and absence in relation to university days
Your Academic Adviser will have access to your attendance record throughout the academic year and this will be discussed at each progression point meeting.
The Programme Team will review attendance weekly and highlight to AAs:
- Any student who has hit a trigger for hours of absence
- Any student with certified non-attendance who may need support and an attendance review with their Academic Adviser (eg repeated short term sick leave).
Triggers for action in relation to attendance are set out below.
First trigger – 10 hours of absence
Response: the student will be emailed (AA copied in) indicating :
- That their attendance is being monitored.
- Reminding them of the full attendance requirements.
- Reminding them of the need to complete unit registers or the relevant online form if they are unable to complete their learning activities if ill or absent.
- Reminding them of how to make up missed sessions.
- They will also be directed to seek support from their Academic Adviser.
Second trigger – 15 hours of absence or on-going problems with attendance relating to health or personal difficulties
Response: The Academic Adviser will be notified that the student has hit this second trigger in relation to absence. The student will be asked to attend a meeting with their AA to discuss their attendance. At the meeting:
- They should be given an opportunity to discuss any factors making it hard for them to attend and helped to develop an action plan to improve attendance.
- Their practice attendance will also be reviewed.
- Students should be referred to any relevant support services to assist them eg ‘My learning essentials’, student support, occupational health, DASS or the counselling service.
- Students should be reminded of their professional responsibility to attend and the need to meet the programme attendance requirements.
- Students should be reminded of the appropriate ways to make up missed clinical hours and missed theory sessions.
- An informal warning may be issued with a requirement to improve attendance.
Third Trigger – 20 hours of absence or on-going problems with attendance relating to health or personal difficulties
Response: The Academic Adviser will be notified that the student has hit this third trigger in relation to absence. The student will be asked to attend a meeting with their AA to discuss their attendance. At the meeting:
- As above and
- A formal warning may be issued with a requirement to improve attendance.
Forth Trigger – 25 hours of absence or on-going problems with attendance relating to health or personal difficulties
Response: The Academic Adviser will be notified that the student has hit this forth trigger in relation to absence. The student will be asked to attend a meeting with their AA to discuss their attendance. At the meeting:
- As above and
- The student may be referred to the Fitness to Practice / Health & Conduct Committee.
The Academic Adviser will discuss with the Programme Director situations where students are struggling to attend due to acknowledged reasons. It may be appropriate to suggest that a student consider interruption if they cannot meet the attendance requirements or their difficulties combined with their poor attendance is affecting their ability to progress on the course.
If a student has not attended either theory or practice for 4 weeks with no communication to explain their absence, they will be written to by recorded delivery, asked to clarify whether they are still on the programme and be invited to attend a meeting with their Academic Adviser and the Programme Director. If no reply is received or the student does not attend to attend a meeting with the Programme Director or their Academic Adviser, they will be referred to the Fitness to Practice / Health & Conduct Committee who may decide to discontinue them from the programme.
Recording Attendance in Practice
You are responsible for documenting their attendance in practice via the PARE timesheets and for asking your practice supervisor/assessor to sign to confirm the hours you have worked on a daily basis. You should ask for the whole sheet to be signed by your Practice Assessor at the end of the placement. Leaving timesheets unsigned for a long time may result in the clinical midwife no-longer being available to sign them or to remember what shifts you worked, so these hours may be lost. Therefore, it is important to get these signed as soon after completion as possible.
If you are off sick on a placement day, you must inform your placement area that you are not going to attend. You must also email your Academic Adviser and the Allocations Team to indicate that you will be absent from practice. You should also indicate that you were off sick on the PARE timesheet.
Practice supervisors and practice assessors have a responsibility to monitor student attendance in placement so they can confidently sign the PARE timesheets and report absent students to the university via bmidwifery@manchester.ac.uk or by emailing the student’s Academic Adviser/Academic Assessor (contact details available via the PARE system).
Recording attendance in relation to case-holding experience
The unit lead will give specific guidance about how you are to record their practice hours for your case-holding work.
Monitoring attendance in practice
You should self-monitor your attendance, using the yearly overview provided each year. If you are not being given enough clinical shifts to meet these requirements, it is your responsibility to raise this with the placement team and seek support from your AA to ensure your have enough shifts. If you are falling behind in meeting your clinical hours requirements, you should discuss this with your Academic Adviser and where feasible, use the making-up practice hours policy to begin to catch up these hours so you are on track by the end of the year. Each year you should complete the required hours of practice learning, which should be documented in PARE.
| Year (part) of study | Practice hours required |
| 1 | 767 |
| 2 | 767 |
| 3 (BMidwif) | 766 |
| 3 (MMidwif) | 600 |
| 4 (MMidwif) | 600 |
Your Academic Adviser will review practice attendance at least twice a year at each progression point (Academic Assessor review). Students who are falling behind (eg 40 hours deficit) in meeting their placement hours requirements will be:
- Given an opportunity to discuss any factors making it hard for them to attend and be helped to develop an action plan to improve attendance.
- Referred to any relevant support services to assist then eg student support, occupational health, DASS or the counselling service.
- Helped to develop a Support in Practice Plan in relation to agreed reasonable adjustments if appropriate.
- Reminded of the appropriate ways to make up missed clinical hours and missed theory sessions and helped to develop an action plan to address the deficit.
- Monitored by their Academic Adviser.
Students reaching 100 hours of missed practice time without reasonable explanations about the reason for absence and no evidence of improving attendance may receive an informal warning.
Students reaching 150 hours of missed practice time (4 weeks of full-time work) without reasonable explanations about the reason for absence and no evidence of improving attendance may receive a formal warning.
Further on-going absences from practice may result in a referral to the Concerns Review Panel / Fitness to Practice / Health & Conduct Committee. Students cannot have more than 150 hours of practice learning outstanding at the end of one part / academic year of the programme. Students having less than 150 hours outstanding will be noted at the September Exam Board and be given retrieval opportunities to complete their hours and/or practice learning outcomes prior to a final board in late November/early December. Students who have amassed more than150 hours of practice learning outstanding will be reviewed and may be required to interrupt the programme and recommence at a later date subject to eligibility to resit. The requirement to interrupt is to enable students time to address the issues that are impacting on their ability to keep up with practice hours, and to avoid accrual of any further hours deficit. Following interruption, the agreed return date would take account of the hours deficit to ensure that the student has enough opportunity to complete the required hours within the programme, which may mean a return date in advance of the start of the next year.
If there are recognised factors affecting your ability to meet the attendance requirements for practice, you will be supported to maximise your attendance but may be advised to interrupt your studies and return to the programme when you are better able to meet the practice learning requirements.
You will not be able to be presented to the NMC for registration until all theory and all practice hours have been completed and documented. You may need to self-fund any making up time at the end of the programme.
Student Attendance Monitoring Process