BACHELOR OF MIDWIFERY (HONS) / INTEGRATED MASTERS
Faculty of Biology, Medicine & Health
School of Health Sciences
Division of Nursing, Midwifery and Social Work
STUDENT HANDBOOK
SEPTEMBER 2024
Version: August 2024
Purpose of this Handbook
The Student Handbook has been developed as a resource for undergraduate healthcare students, providing a comprehensive introduction to the Division of Nursing, Midwifery and Social Work and information on all aspects of your programme of study, and should be used as the first point of reference for questions concerning your program, support and advice, or academic policies and procedures. The University of Manchester is a large and complex organisation and we want to ensure that you know how to access the information and support and guidance you need to succeed in your studies. It is therefore designed to guide you through many aspects of your time as a student and provides useful links to information available through the University’s website, as well as summarising the facilities and support services that are available across the University and how you can access them. It also outlines what you should expect of the Division and what they can expect from you, and clarifies the policies and procedures relevant to your area of study. It is your responsibility to familiarise yourself with the Student Handbook and with the contents of the student pages on Blackboard (http://online.manchester.ac.uk) and to use them as a reference when required since they govern important aspects of your programme and therefore may have a significant impact on your studies and the successful completion of your degree.
This handbook is to be read in conjunction with the SHS Student Handbook.
Note: The material in this handbook can be provided in alternative formats. Please discuss your requirements with your Academic Adviser in the first instance.
Disclaimer
Although the information in this Handbook is accurate at the time of publication, aspects of the programme and of Divisional practice may be subject to modification and revision. The Division reserves the right to modify the programme in unforeseen circumstances, or where the process of academic development and feedback from students, quality assurance processes or external sources, such as professional or regulatory bodies, requires a change to be made. In such circumstances, revised information will be issued. Information provided by the Division in the course of the year should therefore be regarded, where appropriate, as superseding the information contained in the Handbook.
Please keep this Handbook in a safe place, as you will need to refer to it throughout your programme.
1. GENERAL INTRODUCTION
PROGRAMME DIRECTOR’S WELCOME
Dear Student Midwife,
May I congratulate you on behalf of the Midwifery programme team for gaining a place at The University of Manchester, School of Health Sciences. We are truly pleased that you have chosen our programme and we are looking forward to providing you with the support you need to succeed in gaining both your Bachelor of Midwifery (Hons) or Master of Midwifery degree, and professional registration as a midwife.
The place you have secured here at Manchester was highly sought after and we are pleased to say that we have recruited you because we saw in you the potential to become an excellent midwife and you demonstrated your commitment to a career in Midwifery. Over the next three or four years we will make it our priority to help you to develop your potential to the maximum. Together with our partners in the NHS we will endeavour to ensure that you become a confident and competent member of the midwifery profession. You will also need to take responsibility for your part in this process.
This is an extremely demanding and challenging course that will stretch you academically, practically and emotionally. It is essential that you familiarise yourself with the contents of this handbook so that you can avail yourself of the information that you will need to help you progress through every stage of the course. It will be important to strike the balance between work and play and we can support you to find out what strategies and techniques will be helpful for your continuing success. Whilst we will provide the academic support you need to succeed it is essential that you make use of the wide range of sources of support that are available to you and that are outlined in this handbook. It is also important that you seek and take note of feedback that is designed to help you improve your performance, both with your academic work and as you develop your skills and attributes in practice.
Finally, I would personally like to welcome you to a challenging and wonderful profession. I would also like to invite you to continue the tradition of excellence that The University of Manchester has established by achieving your full potential. I offer you a sincere welcome and wish you well.
Helen White,
Programme Director – Bachelor / Master of Midwifery
CONTACT DETAILS
The Division of Nursing, Midwifery and Social
The University of Manchester
Jean McFarlane Building
Oxford Road
Manchester
M13 9PL
Division Website: Nursing | Biology, Medicine and Health | University of Manchester
|
Head of School Professor Andy Brass Tel: 0161 306 0600 |
Head of Division Professor Hilary Mairs Tel: 0161 306 7779 hilary.j.mairs@manchester.ac.uk |
|
Director of Education Sam Freeman |
Head of Teaching, Learning & Student Experience Chris Bamford Tel: 0161 306 7613 |
Programme Management Team
|
BMidwif (Hons) / MMidwif Programme Director Dr Helen White Tel: 0161 306 7844 |
Lead Midwife for Education Margaret Walsh |
|
|
Admissions Manager Suzanne Eden Tel: 0161 305 2334 |
Admissions Tutors Sue Thornber and Gill Singleton |
|
|
Year 1 Lead Kirsty Lowe
|
Year 2 Lead Catherine Anders Catherine.anders@manchester.ac.uk
|
|
|
Year 3 Lead Alice Ciolino Alice.ciolino@manchester.ac.uk
|
Senior Academic Adviser Gillian Singleton Gillian.singleton@manchester.ac.uk Tel: 0161 306 7736 |
|
|
Student Support Manager Saira Jackson saira.jackson@manchester.ac.uk Tel: 0161 275 2559 |
Teaching and Learning Delivery and Development Manager David Parry Tel: 0161 275 2583 |
|
|
Academic Lead for Midwifery Practice Learning Elizabeth Nocton Elizabeth.nocton@manchester.ac.uk Tel: 0161 306 7724 |
Placements Officer Lindsay Blanks Lindsay.H.Blanks@manchester.ac.uk
|
|
|
Academic Lead for Practice Governance Dr Nigel Henderson Nigel.henderson@manchester.ac.uk Tel: 0161 306 78647775 |
||
WHERE TO GO FOR HELP AND ADVICE
Academic Adviser
Each student is assigned an Academic Advisor at the beginning of their degree.
Further information can be found in the SHS handbook here.
Your Academic Adviser will provide you with support throughout your programme. Our aim is that by engaging with your Academic Adviser, you:
- will know that your adviser cares about your progression, academic success and future plans
- will feel that you belong and are valued regardless of your background, personal strengths and weaknesses
- will know who to contact if you experience difficulties either personally, academically or in placement
- will work to enhance your academic and personal self-efficacy as a result of setting & reviewing goals and reflecting on your experiences
- will gain and grow in confidence and skills in developing professional relationships
- will gain professional support in managing your placement learning and assessment.
Your Midwifery programme will examine topics that can illicit strong emotional responses from students. If you are affected in any way by the material covered please seek support from your Academic Adviser who may then refer you to other support services.
You will also have an Academic Assessor who will work with your Academic Advisor to support your progress through the practice and academic elements of the programme.
Year Lead
The year lead will be responsible for having an overview of each year of the programme. This involves liaising regularly with the unit leads for that year and supporting them in managing their unit teams. The year lead will ensure consistency of the delivery of unit learning outcomes and ensure that amendments do not lead to curriculum drift, which means when your learning experience does not match with the unit or programme aims. The year lead will also meet regularly with Academic Advisers to ensure there is a strong link between practice and placement.
CONTACTING LECTURERS
- Lecturers will let you know how best to contact them at the beginning of each unit or, as Academic Advisers, at the beginning of the programme.
- Any meetings are best made at the beginning or end of the day so that lecturers and students are able to have a break at lunchtime.
- If you want to make an appointment you should do so via email, using your university email address
- In an urgent situation any available lecturer can be accessed for advice and support. It may then be necessary to share this information with the academic adviser / unit leader / examinations officer or programme director as appropriate.
- Five days is recognised as a reasonable time for lecturers to respond to students. Please remember that some staff are part time or have research days, holidays etc. If you require an urgent appointment, please check the location details at the main reception on the ground floor at Jean McFarlane Building.
Contact details of lecturers teaching on your programme are available in Blackboard.
PROGRAMME SCHEDULE & KEY DATES
Term Dates
| Semester 1 | Commences | 16th September 2024 |
| Ends | 24th January 2025 | |
| Semester 2 (part 1) | Commences | 27th January 2025 |
| Ends | 6th June 2025 | |
| Semester 2 (part 2) | Commences | 16th June 2025 |
| Ends | 12th September 2025 | |
| Resit period (resits may also take place at other times) | Commences | TBC |
| Ends | TBC |
Please note that the chart below provides an overview of Year One of the Programme illustrating holidays, study leave and allocation of days to each unit. Unit leaders will provide detailed timetables and assessment guidelines. An overview (A-Z) for your second and third year will be made available on Blackboard nearer the time.
Programme Holidays for Year 1 students
| Christmas | 23rd December 2024 – 5th January 2025 |
| Easter break | 7th April 2025 – 20th April 2025 |
| Early summer break | 9th – 15th June 2025 |
| Flexible Summer breaks | Flexible fortnight from a choice, which will be communicated to you at the start of the programme |
Clinical experience will be gained on weekdays, weekends and as night shifts throughout the programme. The clinical hours expected in each week are made clear below.
PLEASE NOTE THAT HOLIDAYS WILL NOT CHANGE BUT OTHER ASPECTS OF THE TIMETABLE ARE LIABLE TO ALTERATION TO FACILITATE LEARNING.
PLEAE DO NOT BOOK HOLIDAYS DURING STUDY OR PRACTICE WEEKS.
Please note that the dates of annual leave for BMidwif/MMidwif students will differ from year to year so you should check the A-Z on Blackboard before confirming any holiday arrangements. In each year there are some opportunities to select from a number of set holidays. Once agreed these programme holidays are non-negotiable. Any breaks taken outside of the programme annual leave dates will be recorded as an absence. Absence may adversely affect your progression and achievement on the programme and may be reported in employment references. If there are clear and compelling reasons why you need to take annual leave at a different time to the published weeks of leave, please discuss this in the first instance with your academic adviser. See also: Programme Attendance Requirements.
It is also important that you make your family and friends aware that your holidays are prearranged and fixed. Please emphasise that they are not to arrange any holidays on your behalf other than at programme holiday times.
Timetable & Course Programme (A-Z) overview
Your Course Programme (A-Z), which shows the teaching pattern for your units across the academic year is available on the Midwifery Gateway on Blackboard. Your detailed timetable is available via MyManchester, by selecting ‘MyCourse’ and ‘Timetable’.
You will be given guidance on accessing your timetable as part of your welcome and induction. If you are concerned that your timetable is incomplete or that you have not been allocated to a seminar group for a unit, you should contact the Programme Support Office for advice.
HEALTH & SAFETY
The Division and its associated Trusts all have NO SMOKING policies which you must strictly adhere to. The University of Manchester has implemented a total no smoking policy throughout the University campus.
Aspects of the course content may cause distress to some students. If you are affected by any of the issues raised, you can access support from your Academic Adviser who may then refer you to other support services such as the counselling service.
ADDITIONAL EXPENSES
It is your personal responsibility to ensure that you have appropriate supplements to your uniform, i.e. black, supportive, soft-soled shoes, scissors, pens, etc.
Whilst the library holds a wide range of texts and journals you will find that your studies are best supported by buying some key texts. Recommendations were sent as pre-course reading.
The cost of travel to the University, to sites and between sites is your responsibility, however, students eligible for The Learning Support Fund can claim back some travel expenses online using the Travel and Dual Expenses (TDAE) link. TDAE is part of the broader Learning Support Fund provided by the NHS Travel and Dual Accommodation Expenses (TDAE).
Please note that the TDAE guidance states that students are expected to travel by the cheapest form of transport available where it is reasonably practical to do so. If you are unable to travel via bus, train or tram please discuss this with your Academic Advisor before travelling by other means.
2. TEACHING, LEARNING & ASSESSMENT
You have elected to study on our programme leading to the academic award of Bachelor of Midwifery (Hons) or Integrated Masters Degree. Successful completion of this programme also leads to eligibility for professional registration with the Nursing and Midwifery Council as a midwife.
BMIDWIF OVERALL PROGRAMME AIMS AND INTENDED LEARNING OUTCOMES
The BMidwif programme aims to:
- Develop midwives who demonstrate professional behaviour and attitudes and are skilled; therefore competent, confident, evidence-based, resilient and compassionate practitioners, ready to safely practise within local and national maternity services, with the potential to become professional leaders of the future, and prepared to contribute to global maternity services.
- Enable registration with the Nursing and Midwifery Council (NMC) in accordance with their standards framework for nursing and midwifery education (NMC, 2018), standards for student supervision and assessment (NMC, 2018a), standards for pre-registration midwifery programmes (NMC, 2019), standards of proficiency for midwives (NMC, 2019a) and the International Confederation of Midwives’ definition of the midwife (ICM, 2017).
- Develop midwives who are eligible for the award of a Bachelor’s honours degree from the University of Manchester, in accordance with the purposes of a Manchester Undergraduate Education (UoM, 2021).
The Lead Midwife for Education and the programme team, within the School, Faculty and University, will employ a range of teaching and learning strategies including role modelling good practice that aim to:
- Foster an environment where intellectual curiosity and judgement is valued, by encouraging and developing skills in critical thinking, evaluation, analysis, and synthesis, problem solving, and individual or group research-based learning. Students will be equipped with a strong grounding in academic skills and research theory, enabling them to search for and critically appraise research evidence, analyse findings, identify best-practice, and consider the limits of knowledge and appropriate application in midwifery care.
- Engender a philosophy of respectful, inclusive and compassionate care for all pregnant or birthing women and people, their babies and families; respecting, enabling and advocating for their human rights, needs, safeguarding needs, views, preferences, decisions and strengthening their capabilities. This philosophy acknowledges social and health inequalities and aims to mitigate them through high-quality midwifery care that actively rejects prejudice and discrimination.
- Promote the midwife’s role to practise safely and competently in optimising physiological processes, supporting physical, psychological, social, cultural and spiritual safety to maximise positive outcomes, and anticipate, recognise, mitigate and prepare for complications.
- Cultivate and role model professional values and behaviours, a strong commitment to collaborative working with pregnant and birthing women and people and their families, members of the multidisciplinary team, student peers from other professions, health researchers, maternity service leaders and commissioners. This commitment will nurture students’ leadership capabilities and healthy team-working skills.
- Prepare students upon qualification to be accountable for the evidence-based care of pregnant and birthing women and people, their babies and families throughout the childbearing continuum. This includes being the lead professional where the pregnancy and birth is straightforward, the coordinator of care within the multidisciplinary team when complexities exist, and promoting public health through health education, promotion and protection for all.
- Equip students with the skills to evaluate the quality of maternity care, emphasising the roles of service-user voices, understanding local needs, clinical governance, audit and feedback, and probity and root cause analysis when adverse incidents occur.
- Enable students to acquire, develop and be responsible for maintaining secure knowledge and skills (including communication, clinical, leadership, technical and digital literacy), emotional intelligence and self-care, and a commitment to lifelong learning throughout the programme and their careers. Students will be encouraged to value reflection, self- and peer-evaluation, and peer support as tools to enable this.
- Immerse students in an environment that embraces and values cultural inclusivity, and that is committed to equality of opportunity regardless of race, disability, gender identity, religious or other beliefs, sexual orientation or age; thus, enabling students to qualify as midwives who also embody these values.
- In accordance with the University’s commitment to widening participation in higher education, and in conjunction with service users and providers, recruit to the programme, applicants from diverse backgrounds who demonstrate the academic potential to thrive within the learning environment of the University of Manchester, a strong commitment to providing person-centred maternity services and the potential to become the professional leaders of the future.
- Continually evaluate the effectiveness of the programme in meeting these aims in collaboration with students, service users, health professionals and practice partners.
In order to meet the aims for the BMidwif (Hons), learning outcomes have been mapped across the programme within and across units of learning, and within and across each year of the programme. These learning outcomes are derived from and fully mapped to proficiencies set out in the NMC ‘Standards of proficiency for midwives’ (NMC, 2019), key international midwifery documents and the Manchester Matrix – the purposes of a Manchester Undergraduate Education.
BMIDWIF INTENDED LEARNING OUTCOMES
Knowledge and understanding
On successful completion of the programme graduates from the BMidwif will be able to demonstrate:
A1. Critical contextual understanding of political, ethical, legal, social, cultural, philosophical and evidence-based influences on maternity care, and how this impacts on outcomes for pregnant and birthing women and people and their babies, midwives and the wider workforce, and maternity services.
A2. Applied and effective understanding of the impact of communication and leadership skills, styles and theories on team- and partnership-working with a range of individuals to enable safe and effective care; including coherent knowledge of the roles of other health and social-care professionals and critical evaluation of the contribution of interprofessional collaboration to the provision of high-quality and safe maternity care.
A3. Applied knowledge of relevant life sciences (including anatomy and physiology, genetics and genomics, microbiology, biochemistry, pharmacology, epidemiology, psychology, and sociocultural influences) to underpin midwifery care; systematic understanding and critical analysis of risk factors and complications that put pregnant and birthing women and people and their babies at risk, of strategies for identifying and assessing those risks, and of the appropriate actions to anticipate, mitigate and prepare for complications.
A4. Secure, in-depth knowledge and critical understanding of the role and skills of the midwife throughout the childbearing continuum, including concepts of health, public health, health education and promotion in relation to multicultural local and national contexts, and an awareness of the global context of maternity services.
A5. Systematic comprehension of research methods, and critical evaluation of research findings and evidence-based practice considering the limits of knowledge and appropriate application to midwifery practice.
A6. Applied, in-depth knowledge and critical understanding of the complex factors influencing and influenced by infant feeding practices and a range of strategies to support optimum feeding practices.
A7. Critical understanding and knowledge of strategies for benchmarking, evaluating and improving the safety and quality of maternity care through clinical governance, innovation and research, evaluation of service-user experience, clinical audit, appraising the evidence-base, and professional leadership.
A8. Acknowledgement and application of the variety of educational, teaching and coaching practices that support and underpin learning.
A9. Digital literacy and a coherent understanding of health informatics.
A10. Generation of a personal philosophy of professional and ethical midwifery practice, including the need for ongoing reflective practice and metacognition, self-evaluation and self-care, continual professional development, self-efficacy and autonomy.
Intellectual skills
On successful completion of the programme graduates from the BMidwif will be able to:
B1. Critically analyse, synthesise and evaluate information and evidence from a range of sources related to concepts of midwifery practice, including those outlined above (A1–10), in order to develop a coherent and applied understanding of safe and evidence-based midwifery practice, including strategies for development.
B2. Construct and support reasoned arguments, engage in debate and draw logical conclusions related to their knowledge and understanding as outlined above (A1–10).
B3. Be intellectually prepared to make sound judgements and decisions, both professional and clinical, and to provide a rationale for them.
B4. Plan and conduct a systematic search of the evidence-base, and critically analyse, appraise and synthesise the evidence related to maternity care to propose strategies or priorities for practice development, further education and/or research.
B5. Think critically to solve complex problems related to midwifery care and ethical practice in a range of midwifery care contexts.
B6. Systematically and honestly reflect on and evaluate their own professional practice, learning and experiential needs, and fitness to practice, in order to develop and realise a continuing professional development action plan.
Practical skills
On successful completion of the programme graduates from the BMidwif will be able to:
C1. Practise in accordance with professional, ethical and legal frameworks of midwifery practice ensuring the safety, wellbeing and needs of pregnant and birthing women and people and their families remain their central focus (ICM, 2019; NMC, 2015; WHO, 2019), demonstrating the ability to escalate concerns.
C2. Apply the knowledge and understanding outlined above (A1–10) and the intellectual skills outlined above (B1–6) to underpin autonomous midwifery practice.
C3. Practise midwifery skills safely, competently and effectively, including in emergencies, providing continuity of carer through the childbearing continuum.
C4. Develop respectful and collaborative relationships with pregnant and birthing women and people, empowering, enabling and advocating for them to make informed decisions about their care.
C5. Effectively apply principles and strategies related to public health to promote the health of individuals, families and communities.
C6. Undertake and document systematic, accurate and holistic assessments of the physical, psychological and sociocultural health and wellbeing, safeguarding needs, changing needs and informed decisions of pregnant and birthing women and people, babies, groups and communities in order to formulate, document and realise collaborative and dynamic plans of care.
C7. Demonstrate safe and effective practice in relation to the administration and optimisation of prescription and non-prescription medicines, applying principles of antimicrobial stewardship; and infection prevention and control, including the use of personal protective equipment.
C8. Create and maintain safe environments of care through the effective use of quality assurance and risk management strategies.
C9. Effectively communicate with a range of individuals sensitively taking account of their cognitive, mental, physical, and behavioural health challenges.
C10. Facilitate effective learning with pregnant and birthing women and people, peers and colleagues, including demonstration of skills in supporting, supervising and coaching junior colleagues and peers.
Transferable skills & personal qualities
On successful completion of the programme graduates from the BMidwif will be able to:
D1. Communicate and practise sensitively, safely and with a positive attitude towards meeting the needs of people from diverse backgrounds and cultures, demonstrating the characteristics that pregnant and birthing women and people value, such as kindness and trustworthiness, respecting individuals’ beliefs and cultural practices, being able to challenge discrimination, and escalate concerns, including safeguarding.
D2. Demonstrate excellent professional inter-personal and communication skills (including verbal, non-verbal, written and digital) in a variety of clinical and educational setting with people from all backgrounds.
D3. Work collaboratively with others as part of a team, including those from other professions, recognising and optimising leadership skills in self and others.
D4. Optimise use of study skills, critical thinking, research and enquiry, problem solving and numeracy skills to address academic and clinical questions and facilitate personal and others’ learning.
D5. Demonstrate digital capability, agility and innovation using relevant, contemporary digital and information technologies to optimise practice.
D6. Develop and apply lifelong learning skills based on a drive to enhance and develop their professional performance in the work environment, including reflection, self-evaluation, and recognising and taking appropriate actions if stress or other circumstances are affecting them.
D7. Effectively and appropriately respond to and participate in change management in maternity services.
D8. Develop a sense of their own potential to make a difference to the wellbeing of pregnant and birthing women and people and their families and to the future development
MMIDWIF OVERALL PROGRAMME AIMS AND INTENDED LEARNING OUTCOMES
The MMidwif Programme aims to:
- Develop midwives who demonstrate professional behaviour and attitudes and are skilled; therefore, competent, confident, evidence-based, resilient and compassionate practitioners ready to safely practise within local and national maternity services, as professional leaders of the future, and prepared to contribute to global maternity services.
- Enable registration with the Nursing and Midwifery Council (NMC) in accordance with their standards framework for nursing and midwifery education (NMC, 2018), standards for student supervision and assessment (NMC, 2018a), standards for preregistration midwifery programmes (NMC, 2019), standards of proficiency for midwives (NMC, 2019a) and the International Confederation of Midwives’ definition of the midwife.
- Develop midwives who are eligible for the award of a Master’s honours degree from the University of Manchester, in accordance with the purposes of a Manchester Undergraduate Education (UoM, 2021).
The Lead Midwife for Education and the programme team, within the School, Faculty and University, will employ a range of teaching and learning strategies including role modelling good practice that aim to:
- Foster an environment where intellectual curiosity and judgement is valued, by encouraging and developing skills in critical and original thinking, evaluation, analysis, and synthesis, systematic and creative problem solving, and individual or group researchbased learning. Students will develop a comprehensive understanding of different systematic approaches to evidence synthesis, including searching for and critically appraising research evidence, analysing findings to inform current practice and future research, debate the nature of knowledge and demonstrate originality in the application of knowledge.
- Engender a philosophy of respectful, inclusive and compassionate care for all pregnant or birthing women and people, their babies and families; respecting, enabling and advocating for their human rights, needs, safeguarding needs, views, preferences, decisions and strengthening their capabilities. This philosophy acknowledges social and health inequalities and aims to mitigate them through high-quality midwifery care that actively rejects prejudice and discrimination.
- Promote the midwife’s role to practise safely and competently in optimising physiological processes, supporting physical, psychological, social, cultural and spiritual safety to maximise positive outcomes, and anticipate, recognise, mitigate and prepare for complications.
- Cultivate and role model professional values and behaviours, a strong commitment to collaborative working with pregnant and birthing women and people and their families, members of the multidisciplinary team, student peers from other professions, health researchers, maternity service leaders and commissioners. This commitment will nurture students’ healthy team-working skills, leadership capabilities and potential, personal responsibility, and enable personal and professional development and the development of others.
- Prepare students upon qualification to be accountable for the evidence-based care of pregnant and birthing women and people, their babies and families throughout the childbearing continuum. This includes being the lead professional where the pregnancy and birth is straightforward, acting autonomously in planning and implementing care, and the coordinator of care within the multidisciplinary team when complexities exist, promoting public health through health education, promotion and protection for all.
- Equip students with the skills to critically evaluate the quality of maternity care, emphasising the roles of service-user voices, understanding local needs, clinical governance, audit and feedback, probity and root cause analysis when adverse incidents occur, and to utilise effective leadership skills and theory to contribute to the evidence-based development or co-creation of maternity services.
- Enable students to acquire, develop and be responsible for maintaining secure knowledge and skills (including communication, clinical, leadership, technical and digital literacy), emotional intelligence and self-care, and a commitment to lifelong learning throughout the programme and their careers. Students will be encouraged to value reflection, self- and peer-evaluation, and peer support as tools to enable this.
- Immerse students in an environment that embraces and values cultural inclusivity, and that is committed to equality of opportunity regardless of race, disability, gender identity, religious or other beliefs, sexual orientation or age; thus, enabling students to qualify as midwives who also embody these values.
- In accordance with the University’s commitment to widening participation in higher education, and in conjunction with service users and providers, recruit applicants to the programme from diverse backgrounds who demonstrate the academic potential to thrive within the learning environment of the University of Manchester, a strong commitment to providing person-centred maternity services as the professional leaders of the future.
- Continually evaluate the effectiveness of the programme in meeting these aims in collaboration with students, service users, health professionals and practice partners.
In order to meet the aims for the MMidwif (Hons), learning outcomes have been mapped across the programme within and across units of learning, and within and across each year of the programme. These learning outcomes are derived from and fully mapped to proficiencies set out in the NMC ‘Standards of Proficiency for Midwives’ (NMC, 2019), key international midwifery documents, Health Education England’s ‘Maximising Leadership in the Preregistration healthcare curricula’ (NHS England 2018) and the Manchester Matrix – the purposes of a Manchester Undergraduate Education.
MMIDWIF INTENDED LEARNING OUTCOMES
Knowledge and understanding
On successful completion of the programme graduates from the MMidwif will be able to demonstrate:
A1. Contextual, comprehensive and critical understanding of political, ethical, legal, social, cultural, philosophical and evidence-based influences on maternity care, and how this impacts on outcomes for pregnant and birthing women and people and their babies, midwives and the wider workforce, and maternity services.
A2. Applied, effective and critical understanding of the impact of communication and leadership skills, styles and theories on team- and partnership-working with a range of individuals considering their own leadership skills and using reflection to develop. Including comprehensive knowledge of the roles of other health and social-care professionals and critical evaluation of the contribution of interprofessional collaboration to the provision of high-quality, safe and effective maternity care.
A3. Applied knowledge of relevant life sciences (including anatomy and physiology, genetics and genomics, microbiology, biochemistry, pharmacology, epidemiology, psychology, and sociocultural influences) to underpin midwifery care; systematic understanding and critical analysis of risk factors and complications that put pregnant and birthing women and people and their babies at risk, of strategies for identifying and assessing those risks, and of the appropriate actions to anticipate, mitigate and prepare for complications.
A4. Critical and comprehensive understanding and critical awareness of the psychological and emotional impact of pregnancy, birth, bonding and attachment on maternal, parent and infant mental health, and of strategies that have been developed for identifying, assessing and supporting mental health and parent/infant relationships.
A5. Secure, in-depth knowledge and critical understanding of the role and skills of the midwife throughout the childbearing continuum, including a comprehensive understanding of concepts of health, public health, health education and promotion in relation to multicultural local, national and international contexts.
A6. Systematic comprehension and practical understanding of research methods, in-depth knowledge and skills in identifying and retrieving appropriate evidence, critical interpretation and synthesis of quantitative and qualitative evidence, critical assessment of the quality of evidence using appropriate quality assessment tools and originality in the application of knowledge.
A7. Critical evaluation of the principles and application of health economics and their relevance to resource allocation, considering the impact of maternity policy on the coordination and delivery of maternity services and service development.
A8. Applied, in-depth knowledge and critical understanding of the complex factors influencing and influenced by infant feeding practices and a range of strategies to support optimum feeding practices.
A9. Comprehensive understanding and knowledge of critically appraised strategies for benchmarking, evaluating and improving the safety and quality of maternity care through clinical governance, innovation and translation of research into midwifery practice, evaluation of service-user experience, clinical audit, appraising the evidence-base, and professional leadership and link this to the effective and efficient management of resources.
A10. Acknowledgement and original application of the variety of educational, teaching and coaching practices that support and underpin learning.
A11. Digital literacy and a coherent understanding of health informatics.
A12. Generation of a personal philosophy of professional and ethical midwifery practice, including the need for ongoing reflective practice and metacognition, self-evaluation and self-care, continual professional development and independent learning, self-efficacy and autonomy.
Intellectual skills
On successful completion of the programme graduates from the MMidwif will be able to:
B1. Critically analyse, synthesise and evaluate information and evidence from a range of sources related to concepts of midwifery practice, including those outlined above (A1–12), in order to develop a coherent, applied and original understanding of safe and evidence-based midwifery practice, including current challenges and insights, to generate and strategies for development.
B2. Construct, support and critique reasoned arguments, engage in debate and draw logical conclusions related to their knowledge and understanding as outlined above (A1– 12).
B3. Be intellectually prepared to make sound judgements and decisions, even in the absence of complete data, both professional and clinical, to provide a rationale for them, and communicate them to specialist and non-specialist audiences.
B4. Plan, conduct and critique methods of identifying and retrieving the appropriate evidence, critically appraise research using different study designs to propose original strategies or priorities for practice development, further education and/or research.
B5. Debate critically the nature of evidence and the goal of evidence-based practice.
B6. Think critically, systematically and creatively to solve complex problems related to midwifery care and ethical practice in a range of midwifery care contexts.
B7. Critically understand of the mechanisms that can be used to influence organisational change and public policy, demonstrating development of political awareness and skills.
B8. Systematically and honestly reflect on and evaluate their own professional practice, learning and experiential needs, leadership potential and fitness to practice, in order to develop and realise a professional action plan.
Practical skills
On successful completion of the programme graduates from the MMidwif will be able to:
C1. Practise in accordance with professional, ethical and legal frameworks of midwifery practice ensuring the safety, wellbeing and needs of pregnant and birthing women and people and their families remain their central focus (ICM, 2019; NMC, 2015; WHO, 2019), demonstrating the ability to escalate concerns.
C2. Apply the knowledge and understanding outlined above (A1–12) and the intellectual skills outlined above (B1–8) to underpin autonomous midwifery practice.
C3. Practise midwifery skills safely, competently and effectively, including in emergencies, providing continuity of carer through the childbearing continuum.
C4. Develop respectful and collaborative relationships with pregnant and birthing women and people, empowering, enabling and advocating for them to make informed decisions about their care.
C5. Effectively appraise and apply principles, strategies, and local, national and international guidelines related to public health to promote the health of individuals, families and communities.
C6. Undertake and document systematic, accurate and holistic assessments of the physical, psychological and sociocultural health and wellbeing, safeguarding needs, changing needs and informed decisions of pregnant and birthing women and people, babies, groups and communities in order to formulate, document and realise collaborative and dynamic plans of care.
C7. Demonstrate safe and effective practice in relation to the administration and optimisation of prescription and non-prescription medicines, applying principles of antimicrobial stewardship; and infection prevention and control, including the use of personal protective equipment.
C8. Create and maintain safe environments of care through the effective use of quality assurance and risk management strategies. Identify and analyse developments necessary within maternity services to meet national and local policy directives for maternity service development and change.
C9. Effectively communicate with a range of individuals sensitively taking account of their cognitive, mental, physical, and behavioural health challenges.
C10. Facilitate effective learning using a range of educational practices in an original way with pregnant and birthing women and people, peers and colleagues, including demonstration of skills in supporting and supervising junior colleagues and peers.
C11. Demonstrate critical understanding of systematic review methods.
C12. Adapt and respond appropriately to changing situations of care, demonstrating sound judgement, personal responsibility and initiative in complex and unpredictable professional environments. Show commitment to interprofessional learning and working whilst working autonomously where appropriate.
Transferrable skills & personal qualities
On successful completion of the programme graduates from the MMidwif will be able to:
D1. Communicate and practise sensitively, safely and effectively with a positive attitude towards meeting the needs of people from diverse backgrounds and cultures, demonstrating the characteristics that pregnant and birthing women and people value, such as kindness and trustworthiness, respecting individuals’ beliefs and cultural practices, being able to challenge discrimination, and escalate concerns, including safeguarding.
D2. Demonstrate excellent professional inter-personal and communication skills (including verbal, non-verbal, written and digital) in a variety of clinical and educational setting with people from all backgrounds.
D3. Critically explore and evaluate concepts, processes and skills related to collaborative, collegiate and effective interprofessional team working, recognising and optimising leadership skills in self and others.
D4. Optimise use of independent learning ability, critical thinking, research and enquiry, creative and systematic problem solving and numeracy skills to address academic and clinical questions, facilitate personal learning and that of others.
D5. Utilise systematic and creative approaches to problem solving and decision-making in relation to complex issues demonstrating resilience, empathetic leadership and emotional intelligence when faced with difficult and complex leadership problems and practice issues.
D6. Demonstrate digital capability, agility and innovation using relevant, contemporary digital and information technologies to optimise practice.
D7. Develop and apply lifelong learning skills based on a drive to enhance and develop their professional performance in the work environment, including reflection, self-evaluation, and recognising and taking appropriate actions if stress or other circumstances are affecting them.
D8. Critically reflect on their own academic and practical performance identifying abilities, limitations and opportunities to improve academically and as a practitioner and educator, utilising a range of improvement strategies.
D9. Respond to, initiate and manage change in maternity services effectively and appropriately, based on critical evaluation of current services and the evidence-base.
D10. Develop self-direction and a sense of their own potential to make a difference to the wellbeing of pregnant and birthing women and people and their families and to the future development of midwifery.
PROGRAMME STRUCTURE
This contemporary and innovative full-time midwifery programme offers the opportunity to study for either a Bachelor of Midwifery (Hons) (BMidwif) or an integrated Masters in Midwifery (MMidwif). The length of the BMidwif is 4,600 hours studied over 3 years, in accordance with the Nursing and Midwifery Council (NMC) (2019) regulations. The length of the MMidwif is 5,468 hours studied over 4 years. Based on consultation with prior students, the BMidwif (which incorporates the first 2 years of the MMidwif) will run over 45 weeks; years 3 and 4 of the MMidwif will each run over 35 weeks. Each week in any year will comprise around 35 hours of learning in either theory or practice, or a mixture of both. Successful completion of either award will result in eligibility to register with the NMC as a midwife. In each year of each programme, 50% of learning is theoretical and 50% of learning is based in midwifery and related learning environments (NMC, 2019).
The theory component will be a blend of face-to-face teaching, including teaching of clinical skills in our skills laboratories, online teaching, guided independent and self-directed study. Learning in clinical practice will take place under the supervision of qualified midwives and other health professionals across two placement sites at local NHS Trust maternity clinical learning environment provider sites. Knowledge, attitude, and skills will be assessed using a variety of methods, including written academic assignments, written examinations, viva voce examinations, clinical skills examinations in the skills laboratories and assessment of performance in clinical practice using the national and NMC-validated Midwifery Ongoing Record of Achievement (MORA).
In year 1, the programme commences with a block of approximately 8 weeks of theory learning, prior to starting in midwifery and related clinical learning environments. From this point onwards you will continue to work directly with women/birthing people, newborn infants and their families under the supervision of qualified midwives and other health professionals. The 50:50 integration of theory and practice learning evolves throughout the programme as your experience and confidence develop. In semesters 1 and 2 of year one, theory and practice are integrated within most weeks, in order to provide you with the support you need as you start to gain experience in practice learning environments. Towards the end of year 1 and in years 2 and 3 you will undertake blocks of weeks in practice learning environments, and blocks of theory learning. This hybrid approach to integrating practice and theory learning aims to provide nurturing support at the start of the programme, then transitioning to longer blocks of time to enable you to focus on the programme requirements in each learning setting.
BMidwif (Hons) route:
Semester 1 and semester 2 in each year of study follow normal University semester dates, however each year also has an ‘extended semester 2’ period because of Nursing & Midwifery Council (2019) regulations regarding the length of midwifery programmes (4,600 hours).
MMidwif route:
In years 3 and 4 of the MMidwif route, the length of study in each year is shorter and there is not an extended semester 2. Each year is 35 weeks long (1,200 hours of study each).
Units of study
All units of study must be completed for success in the BMidwif (Hons) and MMidwif degrees. There are no optional units although in the last 2 weeks of year 2, students may opt to undertake an unassessed area of study and elective placement related to their future career aspirations. These options include: midwifery professional consolidation, developing a research or education career, and international midwifery practice.
Assessments in semester 1 will be completed by end of the semester in line with the university’s examination cycle. Some units in semester 2 will have assessments completed at the end of semester 2 in line with the university’s examination cycle. Alternative assessment periods will be utilised for units where learning continues into the extended semester period (NMC, 2019), including the practice learning assessment evidenced within the MORA.
There are 15 units of study within the BMidwif programme, and 19 in the MMidwif. All units in the first three years have credit rating in multiples of 10 credits, with the 4th year units in the MMidwif being in multiples of 15 credits. The Midwifery Practice units in each year of the programme combine practice learning assessment (via the MORA) with theory learning assessments. At the University of Manchester, your clinical assessment grade will count towards your final degree classification. The clinical practice assessment accounts for 30 credits in years 1 and 2; and 40 credits in year 3 (both BMidwif and MMidwif) and year 4. It should be noted that all units are compulsory and must be successfully completed in order to obtain both the registered midwife qualification and the academic award.
Framework for Higher Education Qualifications for England, Wales and Northern Ireland (FHEQ) Levels 4 to 6 are studied over the three years of the BMidwif, and Levels 4 to 7 are studied across the 4 years of the MMidwif. Full details of units/credits/learning outcomes are presented later in this handbook. The focus of level 4, first year study is on the foundations of midwifery knowledge and application of this to universal midwifery care. At subsequent levels this knowledge is built upon to allow you to understand and detect more complex scenarios and competently care for those with additional care needs. Throughout the programme you will develop the skills to practice as a professional midwife including in continuity of midwifery carer models; to retrieve, critically appraise and apply research-based evidence; to work collaboratively with others and become leaders of the future. Ultimately the Programme will prepare you for employment as midwives at the point of registration.
Teaching and learning strategies have been developed to enable you to have a commitment to life-long learning and equip you with the necessary enquiry, thinking and problem-solving skills to support you in this process. It will also help facilitate the development of midwifery practitioners who are able to reflect on their clinical activities and evaluate their own performance against available evidence.
The programme units are constantly updated to meet the changing needs of women/birthing people and their families, in response to student evaluations and external drivers such as Department of Health directives and NMC requirements.
This programme has been developed through co-creation with a range of stakeholders including current and past students, service users and our practice learning environment partners. The programme is underpinned in structure and philosophy by the most recent NMC Standards for midwifery practice, has been mapped to key national and international midwifery documents and developed following a wide and comprehensive review of current information about the future of the maternity services.
The particular strengths in this programme related to curricular developments are:
- Fully embedding continuity of midwifery carer into practice and theory
- Hybrid approach to integrating theory and practice
- Qualification as a Newborn and Infant Physical Examination practitioner
- Gaining a teaching accreditation with Advance HE as an associate fellow
- The midwife’s important role in public health
- Standards related to the Baby Friendly Initiative
- Research teaching that aligns with our strong Divisional strategy
- Theory learning starting with the foundations of midwifery knowledge incorporating life sciences
- Leadership development, mapped to Health Education England’s model (HEE, 2018)
- Opportunity to explore future career opportunities such as international experience and social enterprise
Content notes: There are occasions in this programme when some sensitive issues and subjects will be covered or discussed that you may find emotionally challenging or feel uncomfortable with. It is important that such issues are addressed within this programme, so that you are prepared to provide high-quality care to individuals who may be affected and to protect yourselves in these situations should they arise in the clinical learning environment. Hence it remains essential that you engage in teaching and learning related to these sensitive issues.
You are encouraged to look at the content of individual units in advance if you think that you might struggle with some of the topics in the course. Topics may include domestic violence, child abuse, termination of pregnancy, mental illness, and racism (this list is not exhaustive as any topic may be distressing depending on individuals’ circumstances). If you feel that you may struggle with the content, you may want to seek support in advance and useful contacts may be your AA or the unit lead.
This programme aims to provide an open space for a critical yet civil exchange of ideas. We ask all learners to help create an atmosphere of mutual sensitivity and respect, just as you will in the clinical learning environment. Please ensure that you are respectful of others and do not use words or share ideas that are offensive or inflammatory. If you disagree with another learner’s ideas, ensure that you discuss their ideas rather than criticising them personally.
If you are concerned about any discussions, please contact the unit lead or the programme director.
INTEGRATED MASTERS IN MIDWIFERY
Students who wish to take the opportunity to qualify with a Masters in Midwifery have the opportunity to study at level 7 in the 4-year integrated Masters programme. To be eligible for the programme you must have achieved an average of a 2:1 (60% and over) throughout your study in years 1 and 2 of the programme. To remain eligible you also need to maintain this level of achievement in year 3.
While years 1 and 2 are exactly the same, irrespective of you electing to study to BMidwif or MMidwif level, year 3 differs. You will undertake fewer theory and practice hours in year 3 of the MMidwif, and the programme runs over 35 weeks. The programme structure, teaching, learning and assessment expectations will also differ on the MMidwif. If you are successful in maintaining the 2:1 average in year 3, you will continue onto study at level 7 in year 4.
If you are unsuccessful in maintaining the 2:1 average in year 3, you will still have the option to qualify with a BMidwif with eligibility to register with the NMC at the end of year 3. This will necessitate making up additional practice and theory hours to meet the NMC Standards (NMC, 2019).
Year 1:
Year 1 lays the foundations for you to develop the knowledge, understanding and skills for competent midwifery practice. ‘Professional Midwifery’ is the basis of a clear thread that runs through the programme enabling you to develop study and research skills, and introduce the concepts of professionalism and ethical practice. You will experience interprofessional education by joining together with learners on the BNurs/MNurs programme for the research thread of this unit. The ‘Foundations’ units support your knowledge of anatomy and physiology, microbiology and pharmacology with which to underpin your understanding of the physiology, and later pathophysiologies, related to childbearing. The ‘Universal Midwifery Care’ units directly reflect Domain 3 of the Standards of Proficiency for Midwives (NMC, 2019), related to the care and support provided to all women/birthing people, their newborn infants and their families. ‘Midwifery Practice 1’ supports you through your first experiences of caring directly for women/birthing people, their newborn infants and their families throughout the childbearing continuum.
| Year 1 – 120 credits at FHEQ Level 4 | ||||
| Semester 1 | Semester 2 | Semester 2 (+) | Credits | Assessment |
| Professional Midwifery | 20 | 1) Information leaflet for learner midwives (1500 words) (50%) (Sem 1) 2) Open book exam (1.5 hours) (50%) (Sem 2) | ||
| Foundations of Midwifery Practice: Anatomy and Physiology | 20 | Online unseen exam, multiple choice (1 hour) and open-book short answer questions (complete within 24 hours) (100%) | ||
| Universal Midwifery Care: Pregnancy and Health Promotion | 10 | Written essay (1500 words) (100%) | ||
| Foundations of Midwifery Practice: Microbiology | 10 | 1) Poster presentation (1000 words) (100%) 2) SafeMedicate drug calculations exam (0%) | ||
| and Pharmacology | ||||
| Universal Midwifery Care: Birth, Following Birth and Infant Feeding | 20 | Written essay: evidence-based care plan (2,500 words) (100%) | ||
| Midwifery Practice 1 | 40 | 1) Clinical proficiencies and MORA assessment (75%)* 2) Structured reflection (1500 words) (25%) | ||
* Practice assessment
Year 2:
Year 2 supports you to build on and develop your knowledge, understanding and skills to apply these in more complex scenarios and competently care for those with additional needs. ‘Professional Midwifery: Being Evidence-based’ continues the thread of developing your research skills with direct application to your clinical roles. The ‘Additional Midwifery Care’ units reflect Domain 4 of the Standards of Proficiency for Midwives (NMC, 2019), and build on the ‘Universal Midwifery Care’ units. The ‘Healthy Teams in Maternity Care’ unit reflects the midwife’s role as part of the multidisciplinary team and in providing an immediate emergency response and first-line management when complications arise. ‘Midwifery Practice 2’ supports you to apply your knowledge of universal and additional care and support, through contribution to the care of all women/birthing people, their newborn infants and families. The Midwifery Practice 2 unit will also enable you to experience clinical practice in another setting through an elective placement, which could be in another Trust in the UK or overseas; and to develop your knowledge, understanding and skills in performing the Newborn and Infant Physical Examination (NIPE).
| Year 2 – 120 credits at FHEQ level 5 | ||||
| Semester 1 | Semester 2 | Semester 2 (+) | Credits | Assessment |
| Professional Midwifery: Being Evidence-based | 20 | Written essay (2500 words): critical appraisal (100%) | ||
| Additional Midwifery Care: Part 1 | 20 | Written essay (2500 words): to include evidence-based care plan (1500 words) with personal development plan (1000 words) (100%) | ||
| Additional Midwifery Care: Part 2 | 20 | Written essay (2500 words): Case study (100%) | ||
| Healthy Teams in Maternity Care | 20 | Clinical competency assessment (50 minutes) (100%) | ||
| Midwifery Practice 2 | 40 | 1) Clinical proficiencies and MORA assessment (75%)* 2) Viva voce assessment (20 minutes) (25%) 3) Safe Medicate Drugs calculations (0%) |
||
* Practice assessment
Year 3:
Year 3 enables you to consolidate your knowledge, understanding and skills, encouraging you to think strategically about the role of the midwife, as an accountable and autonomous clinician, scholar, leader and educator. ‘Promoting Health for Life’ is the capstone unit for the public health thread, when you utilise your knowledge and understanding to think strategically about the midwife’s role in promoting a healthy life course for families. ‘Professional Midwifery: Scholarly Leadership’ encourages you to apply your research and critical thinking skills to practice-related topics and quality improvement of services. The remaining units in year 3 differ depending on which route you are taking. Those on the BMidwif will take the 30 credit ‘Promoting Excellence in Midwifery’ unit. This unit considers the many different roles of the midwife, including leader, communicator, professional, change-maker and educator. Embedded into this unit is guided preparation for you to apply for the Associate Fellowship of Advance Higher Education (HE) (AFAHE). Passing the AFAHE application is not essential to passing the unit, the midwifery degree and registering with the NMC, although the compilation and submission of an application is a mandatory component of the patchwork assessment. ‘Midwifery Practice 3 (BMidwif)’ supports you to apply your consolidated knowledge and understanding, demonstrating proficiency in all areas and your leadership and educator skills. You will also be supported to complete your NIPE qualification. Those on the MMidwif route will take the 10 credit ‘Promoting Excellence in Midwifery Unit’. This unit also considers the many roles of the midwife, in particular as leaders, communicators, professionals and change-makers. Leadership and education form a major aspect of your 4th year studies. ‘Midwifery Practice 3 (MMidwif)’ also supports you to apply your knowledge and understanding by demonstrating proficiency, and to complete the NIPE qualification. You will step-up to the 4th year through a self-directed reflection on your role within a clinical team.
| Year 3 – 120 credits at FHEQ Level 6 | ||||
| Semester 1 | Semester 2 | Semester 2 (+) | Credits | Assessment |
| Promoting Health for Life | 20 | 1) Portfolio (2000 words): Public health strategy (80%) 2) OSCE – Breastfeeding challenges (20%) |
||
| Professional Midwifery: Scholarly Leadership | 30 | Written essay & vlog/blog: Structured literature review (4000 words) and 10 minute vlog (or 1000 word blog) to disseminate information (100%) | ||
| BMidwif: Promoting Excellence in Midwifery | 30 | Patchwork text (4500 words) | ||
| MMidwif: Promoting Excellence in Midwifery | 10 | Patchwork text (1500 words) | ||
| BMidwif: Midwifery Practice 3 | 40 | 1) Clinical proficiencies and MORA assessment (100%)* 2) NIPE: 20 summative NIPE assessments (0%) 3) Safe Medicate Drugs calculations (0%) |
||
| MMidwif: Midwifery Practice 3 | 60 | 1) Clinical proficiencies and MORA assessment (67%)* 2) NIPE: 20 summative NIPE assessments (0%) 3) Written essay: reflective account of continuity of carer experience (2000 words) (33%) 4) Safe Medicate Drugs calculations (0%) |
||
* Practice Assessment
Year 4:
The principle focus in year 4 is leadership, reflecting the national and local goals to deliver improvements in maternity care through strong, effective midwifery leadership (RCM, 2019). All three theory units in year 4 will share learning with multi-professional learners, which may include post-registration health professionals. ‘Critical Appraisal and Evidence Synthesis’ forms part of the Division’s established Masters in Research and enables you to develop a comprehensive understanding of and skills in critical appraisal and evidence synthesis. These skills are essential to midwifery leadership roles in clinical practice, education, management and research. Leadership and Management for Innovation and Educator spans 2 semesters and reflects the enhanced skills learners are expected to apply in clinical practice at level 7. Within this unit you will be supported and guided to apply for the AFAHE accreditation. Passing the AFAHE application is not essential to passing the unit, the midwifery degree and registering with the NMC, although the compilation and submission of an application is a mandatory component of the patchwork assessment. In ‘Perinatal Parent and Infant Mental Health’ you will critically explore perinatal mental health and the impact on parents, families and infants and strategies and interventions to identify, assess and support. All theory units will enable you to develop the intellectual skills to deal with complex issues in a systematic and creative way, to assist you in making sound judgements which you can communicate clearly to a range of audiences. ‘Midwifery Practice 4’ supports you to apply these skills in clinical encounters, demonstrating self-direction and originality in solving problems. You will further develop your knowledge, understanding and skills in clinical practice to act autonomously in planning and implementing midwifery care, and demonstrate leadership skills to enhance team working and develop others.
| Year 4 – 120 credits at FHEQ level 7 | ||||
| Semester 1 | Semester 2 | Semester 2 (+) | Credits | Assessment |
| Critical Appraisal and Evidence Synthesis | 15 | Online assessment comprising of short answer questions (equivalent 3,500 words) | ||
| Perinatal Parent and Infant Mental Health | 15 | Written essay or poster presentation (3500 words) (100%) | ||
| Leader, Educator, Manager, Co-ordinator | 30 | Patchwork text (4,500 words) (100%) | ||
| Midwifery Practice 4 | 60 | 1) Clinical proficiencies and MORA assessment (67%)* 2) Critical incident accounts (2,000 words) (33%) 3) 10 summative NIPE assessments (0%) 4) Safe Medicate Drugs calculations (0%) |
||
* Practice Assessment
Further information on all BMidwif/MMidwif units is available via Blackboard and online on the University of Manchester webpages.
PROGRAMME REGULATIONS AND PROFESSIONAL REQUIREMENTS
Introduction
These regulations supplement the degree regulations of The University of Manchester valid at the time of the student’s admission to the University.
The Nursing & Midwifery Council (NMC) dictate that the minimum award for a preregistration midwifery education programme is a Bachelor’s degree in Midwifery (NMC 2019a). There is no option to register for practice with the NMC if the Honours degree level outcomes cannot be achieved.
Programme Specific Regulations
For MMidwif programme, the following weighting will be used to determine the degree classification:
Y1 to Y4 (L4 to L7 FHEQ) using weights of 0.0 (L4), 0.2 (L5), 0.4 (L6) and 0.4 (L7),
For BMidwif (Hons) programme, the following weighting will be used to determine the degree classification:
Y1 to Y3 (L4 to 6 FHEQ) using weights of 0.0 (L4), 0.33 (L5), and 0.67 (L6),
No accreditation of prior learning (APL) is permissible for entry to midwifery degree programmes. The midwifery programme is exempt from the degree regulations pertaining to APL: “Schools can stipulate when APL is not allowed due to Professional Body requirements.” NMC Standards for pre-registration midwifery programmes (2019) section 1.3 states that “recognition of prior learning is not permitted for pre-registration midwifery programmes”.
The NMC Midwifery standards refer to ‘parts’ of the programme, whereby students should complete all elements of one ‘part’ before progressing to another. NMC Standards for Supervision and Assessment of students (2019b) 9.1, 9.4 and NMC Standards Framework for Nursing and Midwifery Education (2019c) 3.8 refer to “9.1 academic assessors collate and confirm student achievement of proficiencies and programme outcomes in the academic environment for each part of the programme” and “progression for each part of the programme”.
Each ‘part’ is an academic year hence students cannot have more than 150 hours of practice learning or any theory or practice learning outcomes outstanding at the end of one part/ academic year of the programme, as this would prevent them progressing to the next part of the programme. Students having less than 150 hours outstanding will be noted at the September Exam Board and be given retrieval opportunities to complete their hours and/or practice / theory learning outcomes prior to a final board in late November/early December. Students who have amassed more than 150 hours of practice learning and / or practice / theory learning outcomes outstanding will be reviewed and may be required to interrupt the programme and recommence at a later date subject to eligibility to resit. The requirement to interrupt is to enable students time to address the issues that are impacting on their ability to keep up with practice hours, and to avoid accrual of any further hours deficit. Following interruption, the agreed return date would take account of the hours deficit to ensure that the student has enough opportunity to complete the required hours within the programme, which may mean a return date in advance of the start of the next year.
A maximum of 40 credits can be carried over into the next year at the discretion of the Examination Board, who will refer to regulation G36 in these considerations.
No compensation is permissible NMC Standards Framework for Nursing and Midwifery Education (2019c) section 5.16 “there is no compensation in assessments across theory and practice learning.”
Reassessment is essential in the final year of the BMidwif (Hons) and the MMidwif in order to satisfy the requirements of the NMC but referred marks will be capped at the pass mark. NMC Standards for pre-registration midwifery programmes (2019a) section 4.3 “ensure throughout the programme that students meet the NMC Standards of proficiency for midwives and programme outcomes”. Referral marks must be capped at 40 for UG and 50 for the master’s year as no compensation is permissible (above).
Reassessment is required in the final year as all components need to be passed.
Exit awards
BMidwif (Hons) with eligibility for Professional Registration with the NMC (for those originally intending the MMidwif but do not continue to L7)
Learners must achieve a minimum of 360 credits, which includes 120 credits at each QAA FHEQ levels 4–6. Professional registration as a midwife is only possible when all theory and practice hours are complete (minimum 4600 hours, 50% theory and 50% practice) and all clinical proficiencies are achieved at the end of the third year, level 6. This will necessitate an additional 166 hours each theory and practice to make up the difference between the MMidwif route and the BMidwif route in year 3. Practice hours and achievement of all clinical proficiencies must be demonstrated and theory hours can be achieved through completion of the extra theory delivered on the BMidwif route, including successful application for Associate Fellowship of Advance Higher Education (AFAHE).
Bachelor of Science Healthcare Studies (maternal and fetal)
This exit award is available to students who do not complete the BMidwif programme and have achieved at least 300 credits, which must include 60 credits at QAA FHEQ level 6. No option for professional registration.
ASSESSMENT
Introduction to Assessment
This section reflects the assessment regulations of the University of Manchester. The standard of the University’s awards and the students’ confidence in the equity and parity of the assessment of their work depends crucially on the scrupulous conduct of all matters relating to the assessment process.
The Bachelor of Midwifery programme and the Master of Midwifery are bound by the degree regulations of the University of Manchester valid at the time of the student’s admission to the University. In addition to these regulations, there is a requirement for additional rules and regulations in relation to midwifery education, as prescribed by the Nursing & Midwifery Council (NMC).
All units of study need to be assessed and in this programme you will be assessed in both theory and practice elements.
The purpose of assessment is to form a judgement on the quality of your work, to ascertain and certify levels of achievement, and to enable examiners’ to report on the standard of performance reached by students.
You will have formative opportunities to undertake that will help you meet the requirements of assessments. Assessments must be passed in order for an award to be conferred. Failure to pass all assessments will affect your progression through the course and may result in discontinuation of your studies.
The pass mark for all assessed work is 40% for years 1-3 and 50% for the integrated master’s year, unless stated otherwise.
The dynamic nature of midwifery education, the variety of assessment strategies, and the changes in University regulations will lead to periodic review of the assessment information within this handbook.
You will be notified of updates through the Blackboard Community Areas – Midwifery Gateway and Practice Learning Gateway. It is important to check this information on a regular basis.
It is essential that you familiarise yourself with these regulations so that you are aware of the correct procedures to follow for all assessment matters.
Systems are in place to support your progression throughout the programme. Please take time to read the rest of this section as it will guide you through relevant processes. If you have a problem or concern at any stage of the assessment process it is beneficial to the student to deal with issues as they arise by contacting their academic adviser in the first instance.
Range of Assessments
A range of assessments are utilised within the programme in order to assess your knowledge, understanding, and developing intellectual, practical and key transferable skills.
There is also a significant amount of practice assessment. In each year you will complete a Midwifery Practice unit that involves clinical placements requiring achievement of practice-based outcomes and competencies, these will be assessed by a Practice Assessor confirming achievement of proficiencies. Your progress will be evidenced in the Midwifery Ongoing Record of Achievement (or MORA) which will be accessed via an online system called PARE (Practice Assessment Record and Evaluation). This is essential to assess your abilities to demonstrate achievement of the knowledge and skills necessary to meet the proficiencies required by the NMC for entry to the professional register. You must demonstrate that you are at the required level in all the unit learning outcomes and the NMC proficiencies in order to pass the practice unit in each part (academic year). You must also pass all theoretical assessments. Both theory and practice assessments contribute to the grade awarded for the unit. Your Academic Assessor will collate and confirm achievement of proficiencies and other programme outcomes at the end of each part (academic year). The Academic Assessor will work in partnership with our Practice Assessor to recommend progression to the next part (academic year) of the programme.
For each assessment, you will be provided with written guidelines to help you formulate your work. For those units incorporating both practical and theoretical assessment elements, both elements of the assessment must be passed in order for you to be awarded credit for the unit.
Preparing for Assessments
Thorough preparation for any form of assessment should enable you to reach your maximum potential.
For each unit of study there is a unit lead and a deputy unit lead who provide much of the teaching for the unit and who work together to provide guidance and feedback opportunities in relation to the unit assessments.
Opportunities for academic support is normally timetabled where you can meet with the unit lead and/or deputy unit lead to discuss issues relating to your assessment work.
Opportunities to gain formative feedback on your work prior to assessment will be provided. This will take a variety of formats. For example the unit leads may provide an opportunity for you to submit up to 500 words of formative work. The purpose of this is to provide feedback on style and level of writing and ability to integrate evidence into your lines of discussion Other formative feedback opportunities may include a seminar where you can present your work to a small group to allow discussion about a case study and your plans for your assignment.
Where the unit assessment is an examination you will have an opportunity to undertake practice questions and discuss answer plans.
There will be plenty opportunities to gain developmental feedback throughout the programme, so you are strongly advised to actively participate in seminars, academic support sessions and/or by completing practice examination questions as appropriate.
Details of appropriate and specific academic support within units are contained within your unit handbooks and on the timetable. Unit leads may provide formative feedback from draft work normally no later than two weeks prior to submission. Should a unit lead be unavailable for any reason you are advised to contact the Deputy Unit Lead in the first instance for guidance.
Should you feel there are any adverse circumstances that may be affecting your ability to engage with your studies you are strongly advised to discuss these with your unit lead, academic adviser, practice supervisor, or practice assessor as appropriate.
MANAGEMENT OF THE ASSESSMENT PROCESS
University and Professional Requirements for Progression
Both the University and the NMC set requirements for progression from one part of the course to the next. NMC progression points exist before the end of each academic year of the programme, and at the end of year 3 (Year 4 for MMidwif) for progression to the register.
Progression
- Progression to the final year (level 7) of the Integrated Masters is dependent upon you achieving an average of at least an upper second classification by the end of the second year in order to register for the Masters (level 7) element of the course.
- If you undertake the MMidwif component and subsequently withdraw, you must complete all outstanding necessary theory and practice learning elements in order to be eligible to register with the NMC with a Bachelors (Hons) degree in order to practice as a midwife.
- You are required to declare, at the beginning of each new year of study and upon return from interruptions, any changes to or that there are no changes to your health and your Disclosure & Barring Service record via a self-declaration.
Guidelines for Assessment Course Work Requirements
Further information can be found within the SHS handbook here.
Presentation of Assignments
- Presentation is an important aspect of assignment writing. Poor presentation of assignments can result in poor marks. You are strongly advised to take heed of the following guidelines. Further aspects of assignment presentation can be obtained from Academic Advisers, Unit leaders, and the study skills workbook.
- All work handed in must be accompanied by the relevant submission details completed by you, including your correct ID number and course unit code (beginning “NURS”). This should be inserted into the header.
- Each page must be numbered, preferably at the bottom centre position.
- Each assignment must possess a reference list using the Harvard referencing style. For any student who has cited throughout their work but fails to provide a reference list, the assessment will be marked, and a 10% reduction will be applied by the marker. The rubric will be used to reflect this mark reduction. A comment will be provided by the marker, in the feedback, noting the lack of a reference list. This change does not replace or impact on the policy pertaining to academic malpractice.
- Assignments should not be decorated. This is unacceptable in academic work.
- The specific requirements for assessments can be found in the individual unit guide.
Referencing – The Harvard System
Accurate referencing of all written work is essential as it enables readers to (i) assess the accuracy of the writer’s interpretation of source material; (ii) check the writer’s integrity; and (iii) easily seek out material that may be of interest to their own studies. All assignments completed for this programme of study are required to have a reference list.
Though there are many referencing/bibliographical systems around, the Harvard system is the system adopted by many of the prestigious social work and social science journals. More importantly, it is the system, which the Division of Nursing, Midwifery & Social Work has adopted.
This means that it is the only system, which is acceptable for any work submitted by students within the Division. Please see the Library’s Referencing Guide.
ASSESSMENT PROCESS
Location of Examinations Office
The Examinations Secretary is located in the Division of Nursing, Midwifery & Social Work exams office, Jean McFarlane Building, University Place. In recognizing ‘normal office hours’ (Mon-Fri 9.00am-4.00pm) you should take account of the normal breaks which occur during the working day in the morning and afternoon and at lunchtime. You should contact examination office staff by email in the first instance: shs.assessments@manchester.ac.uk.
Mitigating Circumstances
Further information can be found within the SHS handbook here.
As you are on a clinical programme and your reason for an extension or mitigating circumstances may impact on your placement, your academic team will be made aware so that they can review your fitness to practice.
MARKING CRITERIA – GUIDELINES FOR ACADEMIC ACHIEVEMENT
General Statements
Specific guidelines for each assignment will be issued by the unit leader. However, a set of general marking criteria is in use across the Division and these apply to all academic work at undergraduate level. These are as follows:
General Statements which apply across all Levels:
- At every level you should apply presentation guidelines as set out in the programme handbook/guidelines for the assessment.
- At every level you should adhere to the recommended method of referencing as set out in the programme handbook.
- At every level you should demonstrate (as a minimum) knowledge/awareness of acceptable standards of practice.
- At every level you are required to address the aims of the assessments as set out in the assessment guidelines.
You are advised to stay within the recommended word limit for assignments +/- 10%. The penalty which are levied for words in excess of this limit will be a ratio of 1% per 100 words.
The Division uses one set of generic marking criteria to mark all assessments. The marking criteria are structured on 9 themes:
- Transferable skills
- Learning outcomes and assessment criteria: adherence to the criteria for assessment in the question.
- Structure, planning and organization.
- Evidence of reading that is appropriate, relevant, broad, and accurately recorded.
- Use of research to support the discussion
- Knowledge and understanding of the topic, the main issues and the concepts
- Application of theory to practice
- Reflection on practice which identifies professional development and responsibility
- Arguments: the understanding of the topic and associated issues/debates
The level descriptors increase incrementally each year of the programme according to the academic level. All marking will reflect the descriptors and marks will be allocated from 0-100%.
The full marking criteria are available in the Assessments area of Midwifery Gateway on Blackboard. You are encouraged to familiarise yourself with the descriptors to gain a better understanding of the academic level required of your assessments for each year of the programme, as well as understand how marks are awarded according to the descriptors.
EXTERNAL EXAMINERS
The External Examiners for this programme are:
Year 1
Zoi Vardavaki, Senior Midwifery Lecturer, London South Bank University.
Year 2
Helen Recchia, Senior Midwifery Lecturer, University of York.
Year 3
TBC
Year 4
TBC
OCCUPATIONAL HEALTH CLEARANCE
Continuation on the programme is conditional on continued health clearance. The BMidwif (Hons) / MMidwif programme is predicated on an integrated model of learning combining both theory and practice. If at any stage the Division is notified that you are not fit to attend, either by an advisory notification from Occupational Health or through a GP fit note you would normally be placed on sick leave (attending neither theory or practice). A continued period of sick-leave may lead to a period of interruption from the programme. See also: Attendance and Interruptions.
In order to maintain safety for the public, your colleagues and yourself, the Division will defer to the advice and recommendations of Occupational Health in matters of health and fitness for the programme.
During the course of your programme you may engage in Exposure-Prone Procedures and you should follow the guidelines in the Division’s Exposure-Prone Procedures Policy (https://documents.manchester.ac.uk/display.aspx?DocID=46917). If you have any concerns about your own health in this regard please refer to the advice available on Blackboard.
The Occupational Health Department operate an ‘open door’ policy where you can make an appointment at any stage of your course. Where you self-refer to Occupational Health no report or contact with the Division is made without your consent. If it is mutually agreed that a report would be helpful then this will be undertaken with your consent.
If you have health concerns (physical or psychological) or a disability that affects your ability to study you may be referred formally to the Occupational Health Service by anyone with a concern e.g. Division, accommodation pastoral team etc. You may also be referred if study is affecting your health. The referring party should advise you of the reason for referral. When referred, the Occupational Health department will email you to arrange an appointment time.
In making decisions with regards to medical fitness for the programme, Occupational Health will ensure that they comply with relevant legislation, e.g. Equality Act 2010 and National Fitness Standards.
The Occupational Health Physicians and Occupational Health Nurses are all bound by the Code of Professional Conduct as set out by the GMC and NMC and the information you provide to the Occupational Health Service is subject to the General Data Protection Regulation (GDPR) and the Data Protection Act 2018 and will only be divulged with your informed consent.
You must inform your Academic Adviser or self-refer to Occupational Health if you are pregnant: see Policy for Pregnant Students.
You must inform the Occupational Health Services of any needlestick or sharps injury which occurs whilst on placement in addition to meeting the accident reporting requirements of the NHS placement provider. You must also notify your academic adviser.
RESPONSIBILITIES OF STAFF AND STUDENTS
Blackboard Student Communities
The various Blackboard community pages such as Midwifery Gateway and the Practice Learning Gateway have been devised to provide information that is generic to all course units within the programme. Please explore these sites to find lots of important information to help you get going with your studies.
3. PRACTICE LEARNING
THE ARRANGEMENT OF PRACTICE LEARNING EXPERIENCES
The placement of any midwifery or nursing students within the maternity services of the NHS Trusts affiliated with The University of Manchester should be negotiated through the Allocations Officer for this programme.
Different Trusts organise the provision of midwifery care in different ways so learning environments will vary from Trust to Trust, although the Allocations Officer in conjunction with the Academic Lead for Midwifery Practice will ensure that you experience the range of learning environments needed to meet the practice learning requirements of the programme.
The Allocations Officer will normally inform you of your allocation at the beginning of the programme and thereafter, prior to the commencement of each year of the programme. Notification will be provided via your university e-mail.
The BMidwif/MMidwif programme will expose you to learning environments in two different hospital sites across the Greater Manchester region to facilitate a variety of experiences. In year 1, we endeavour to provide learning experiences in one hospital, and then another hospital for years 2 and 3 (and 4 if applicable). However this arrangement is subject to availability and the provision of maternity services in the area.
You will be allocated a Practice Assessor in each year / part of the programme, who will assess your learning and development across several learning environments.
HUB & SPOKE
During some allocations you may want to arrange to visit a related department or gain relevant experience. An example might be that during your allocation to the antenatal clinic you would like to spend an afternoon in the ultrasound scan department when there is no official clinic running. Your Practice Supervisor(s) / Practice Assessor should facilitate the organisation of this and any requests should be raised during the initial interview.
As you move through the programme you should document evidence of having cared for maternity service users with concurrent medical or gynaecological conditions. You should also arrange spoke visits (where available) to relevant medical and gynaecological learning environments to develop your understanding further. This experience should also be documented in the MORA, within the ‘Complementary placement records’, to evidence that you have met the EU requirements in this field. The PEFs will provide details of how to organise spoke visits.
CONTINUITY OF MIDWIFERY CARER
Evidence supports midwifery continuity of carer as a safe and effective model of care, which optimises outcomes and enhances individual experiences for childbearing women/people, their babies and families (Perriman et al., 2018; Sandall et al., 2016; Forster et al., 2016; Rayment-Jones, 2015; Mclachlan et al., 2012). Continuity of carer (CoC) is a central aspect of maternity policy and has become a focal part of the National Maternity Transformation Programme (NHS England, 2016; NHS England, 2017). In recognition of the importance of CoC, and the future midwife’s role working within this model of care, the new NMC standards of proficiency for midwives (NMC, 2019a) have devoted a whole domain to continuity: ‘Domain 2: Safe and effective care: promoting and providing continuity of care and carer’. This domain stipulates the CoC requirements for undergraduate midwifery students to “demonstrate the ability to provide continuity of midwifery carer across the whole continuum of care and in diverse settings for women and newborn infants with and without complications and additional needs” (NMC, 2019a., pp. 17)
The provision of midwifery students CoC has been identified to be beneficial for professional learning, development and skills acquisition (Moncrieff et al., 2020; Sidebotham and Fenwick, 2019; Rawnson, 2011). Similarly to CoC provision by qualified midwives, continuity by student midwives has been shown to have a positive impact for the individuals receiving the care and associated with improved clinical outcomes (Tickle et al., 2021).
CoC is a key thread that runs throughout the programme, in both university-based theory and practice-based learning. By embedding CoC in this way as a student midwife you will be exposed to optimal learning opportunities, which will continuously enable you to link your acquired theoretical knowledge and practice-based experience of CoC. The hybrid programme structure has been developed to enhance learning, enabling you as a student midwife flexibility and the opportunity to maximise your experience of midwifery continuity. As a student midwife within the practice learning environment, you will be involved in the provision of maternity care through the pregnancy continuum, including holding a small caseload. The level of your participation in this care will develop throughout the course and in accordance with your stage of learning. This practice-based learning will complement your theoretical learning; starting in year one with a focus on universal care and midwifery-led care pathways, and then developing from year two to include continuity of care for those with additional needs. This structure of your CoC experience within the practice learning environment is outlined as follows:
- Year 1: As a student midwife you will observe and participate in the provision of care through the pregnancy continuum for a small number of women/people on a midwifery-led pathway
- Year 2: As a student midwife you will contribute to the provision of continuity of carer for a small caseload of women/people, including those with additional care needs
- Year 3: As a student midwife you will demonstrate proficiency in providing continuity of carer for a small caseload of women/people. You should aim to recruit some women/people with additional needs or complexities that enable further self-development of specific skills
- Year 4: As a student midwife you will gain further experience related to working within a continuity of carer team/model
Your experiences of providing CoC within the programme will be used as evidence of your developing proficiency in providing midwifery care across the childbearing continuum. Your experiences should be recorded and reflected upon in the MORA. The NMC standards for supervision and assessment (NMC, 2018a) will be adhered to for all practice-based learning and therefore for all CoC experiences as a student midwife you will be working under the supervision of a qualified midwife. In partnership with the practice learning providers the University will provide clear guidance and support for you regarding student midwives’ provision of CoC. This will optimise the CoC learning experience (Moncrieff et al., 2020) alongside promoting safety for yourself as a student midwife and for the individuals you are caring for.
ATTENDING HOME BIRTHS
We would like to facilitate your attendance at home births where feasible. If you have a home birth imminent in your community area, you should discuss this with your Community Practice Supervisor and with your unit leader(s) so that they can highlight sessions that must be attended and those that could be made up later should you need to attend the birth during a theory day. A maximum of 3 days per year of theory time may be used in this way. Missed theory sessions must be made up. Additional practice hours can be documented in PARE.
MIDWIFERY ONGOING RECORD OF ACHIEVEMENT (MORA)
Assessment within the Midwifery Ongoing Record of Achievement (MORA) evidences your development towards the required proficiency of all midwives and forms an important part of the assessment strategy over the programme. The MORA is hosted by an online platform called Practice Assessment Record & Evaluation (PARE) https://onlinepare.net. PARE also allows you to provide feedback and evaluation of your learning experience in an easy and timely manner. The feedback that you provide is essential to ensure that practice learning experiences are enhanced and supported for all learners in practice.
The Midwifery Ongoing Record of Achievement (MORA) comprises:
- NMC proficiencies that relate to the NMC Standards of proficiency for midwives (NMC, 2019); a proportion of which must be achieved to a specified level in each year of the programme.
- Space for you to generate evidence of achievement of proficiencies, including:
- Practice Episode Records
- Breastfeeding assessment records
- Feedback from Supervisors
- Feedback from service users
- Your own reflections
- Records of clinical experiences of providing care for a certain number of women/birthing people and babies, to achieve Directive 2005/36/EC
- This includes records within the Complementary placement records
- Practice Assessor reviews, including 2 formative assessments and 1 summative holistic assessment each year
- Records of meetings
- Records of your completed practice hours
Further guidance on use and completion of the MORA is available on PARE in the ‘MORA Context Document’ and in the ‘Student Guidance’ section.
PRACTICE LEARNING REGULATIONS & GUIDELINES
All learners are allocated to practice learning environments that meet the requirements of the curriculum. All learning environments undergo an education audit and have assurances that there are enough Practice Supervisors and Practice Assessors to support teaching and assessment of students in practice. You will be allocated to a variety of learning environments to ensure you experience practice across a range of settings. The provision of learning experiences throughout the curriculum has been developed and expanded in partnership between service and University colleagues. You will be required to travel to your allocated learning environment.
Learners are normally informed of their allocation to a learning environment 4 weeks prior to commencement. Notification of allocations is via your student e-mail account. Students MUST contact the learning environment 2 weeks prior to commencing to discuss arrangements for arrival. Learning environments allocated to learners will not normally be changed. In exceptional circumstances learners may request a change to their allocation by completing the Trust Change Request form available on Blackboard within the Practice Learning Gateway.
Your Academic Adviser / Academic Assessor is available for you to discuss your MORA development and practice learning progress. Should you have any areas of concern relating to your learning environment you can discuss these with your Academic Adviser / Academic Assessor. There are also formal procedures available to report your concerns / evaluations of your practice experiences: guidance on providing feedback and raising concerns is available in the Practice Learning gateway in Blackboard.
If you sustain a sharps injury or needlestick injury in the learning environment, you must report this immediately to your Practice Supervisor / Practice Assessor and Academic Advisor. You must also attend the University Occupational Health Department for review, even if the learning environment ask for you be reviewed at your trust Occupational Health Department.
See also: Attendance requirements
WHO WILL BE AVAILABLE TO SUPPORT ME DURING MY PRACTICE LEARNING EXPERIENCE?
Practice Supervisors (PS)
Registered Midwives or other registered health or social care professionals are able to be Practice Supervisors. They have current knowledge and experience and are appropriately prepared for the role in which they;
- Ensure safe and effective learning experiences
- Facilitate independent learning
- Provide co-ordination and continuity of support and supervision
- Ensure observation on your conduct, proficiency, and achievement of programme outcomes are shared with key staff, for example, other Supervisors
- Contribute to assessment and record regular feedback
They have responsibilities for overseeing your progress during your learning experience and may undertake your initial interview supporting you to identify your learning needs, discussing the learning opportunities and completion of your learning plan.
Supervisors have an important role in contributing to your assessment and giving you regular feedback, collaborating with other Supervisors and your nominated Practice Assessor. You may, depending on your allocated learning environment, have several Practice Supervisors supporting your development.
Practice Assessors (PA)
Practice Assessors for midwifery students must be Registered Midwives with current knowledge and expertise and are appropriately prepared for the role in which they;
- Conduct assessments, informed by feedback from Practice Supervisors
- Make and record objective decisions, drawing on records, observations, student reflection and other resources
- Periodically observe you in practice (by objective evidence-based assessment)
- Gather and coordinate feedback from Practice Supervisors and other relevant people
- Schedule communication with Academic Assessors at relevant points
- Review assessment documentation in your MORA that has been completed by your Supervisor(s) and a range of other health or social care professionals who have contributed to your development
- Assess your conduct, proficiency and achievement of proficiencies and will complete the 2 formative reviews and final summative holistic assessment and review of proficiency achievement at the end of the year.
As well as undertaking the required supervision and assessments, the role of the Practice Supervisor and Practice Assessor also includes identifying relevant learning opportunities and creating learning and development plans with the student. In situations where a concern is raised about progress, knowledge-base or conduct, a progression plan will be developed by your Practice Assessor in collaboration with you and your Academic Assessor.
Academic Assessors (AcAs)
Academic Assessors must be Registered Midwives who are nominated for each Part of the programme and are appropriately prepared for the role which includes;
- Working in partnership with your Academic Adviser
- Working in partnership with the Practice Assessor to evaluate and recommend you for progression for each part of the programme. In this context a part refers to the end of each year
- Understanding your learning and achievement in practice
- Undertaking scheduled communication and collaboration with your Practice Assessor
- Collating and confirming your achievement of the proficiencies required within each part of the programme, based on assessment and information that is objective and fair
You will be allocated an Academic Assessor for each Part of the programme (i.e. each year) and within each year there are different levels of performance that you need to demonstrate.
Academic Assessors will collate and confirm your achievement of the proficiencies required within each part of the programme. They will review your progress throughout the year and complete the final assessment in collaboration with the Practice Assessor, having considered your progress and all the evidence. Your Academic Assessor will review your MORA progress following each Practice Assessor review (formative and summative reviews), as indicated on your timetable. If there are any development needs in relation to your performance, they will work with the Practice Assessor in agreeing a progression plan. The progression plan will be reviewed by your Practice Assessor and Academic Assessor together to ensure that the progression plan outcomes have been achieved, or consider further actions. Following the summative holistic assessment (and a retrieval opportunity, where needed) at the end of each part, the Academic Assessor will confirm achievement of the outcomes required in that part or indicate non-achievement.
Your Academic Assessor in the final allocation in your final year will review and confirm overall achievement of the programme practice requirements in collaboration with your Practice Assessor to recommend progression to registration.
Practice Education Facilitators (PEF)
Practice Education Facilitators (PEF) are Trust employees whose role is to facilitate learning in practice for all undergraduate healthcare students, with a particular focus on quality assurance and inter-professional learning. The PEF has an overview of your learning environment and is a point if contact if needed. Please refer to the Practice Gateway within Blackboard for further information. In some trusts, there are Practice Education Practitioners (PEPs) who support the PEFs.
University Link Lecturers (ULL)
An ULL acts as the primary link between the University and the learning environment.
The Midwifery ULL role includes:
- Working effectively as a team with PEFs, taking a risk assessment approach, to ensure the provision of appropriate learning environments
- Provide student, Practice Supervisor and Practice Assessor support
- Working collaboratively with all stakeholders and ensuring good channels of communication are in place
A list of ULLs is located via the Practice Learning Gateway within Blackboard.
Student Illness during Practice Learning Experiences
If you are ill or absent for any reason during practice learning experiences, on the first day of absence you should inform your Practice Supervisor / Practice Assessor (or a designated deputy) of the reason, by telephoning the clinical area (it is also good practice to contact the Practice Education Facilitators). Please also email your Academic Advisor. If your absence is notified in the required manner you should note this as an ‘authorised absence’ in your PARE timesheet; if you do not correctly notify your absence this will be noted as an ‘unauthorised absence’ in your PARE timesheet (please see the absence reporting flow chart in Appendix).
If you are unable to attend your learning environment for any reason it is important that:
- All relevant people are informed in the interest of professionalism and safety
- Your absence is noted on your PARE timesheet
Please note that nursing / midwifery students are not automatically entitled to Wednesday afternoons off. If you are a member of a university club which meets on a Wednesday afternoon you can try to negotiate this time off with the Practice area, but you will need to make this time up on another weekday or at the weekend.
Due to NMC regulations, all absences including authorised absences must be made up to complete the programme. You can find guidance on making up missed practice hours on the Practice Learning Gateway in Blackboard.
ATTENDANCE IN PRACTICE
All students are required to work the normal shift times of their learning environment starting and finishing at the same time as other staff (with similar breaks). Commitment to attendance and punctuality is important and will be closely monitored.
During the programme you are considered as supernumerary, this means you are not calculated as part of the workforce, it does not mean you are unable to undertake any duties. You will be expected to observe and participate in clinical activities and duties with supervision as appropriate to your level and abilities.
You will be expected to work early and late shifts, standard and long day shifts and some night duty. You are also expected to work some weekends with your Practice Supervisor(s). Requests for a bank holiday as a day off should be considered sympathetically. In some learning environments and for your continuity of carer experiences you will be expected to work ‘on-call’ duties alongside your Practice Supervisor. If you have difficulty meeting the ‘on-call’ requirements of the learning environment, you should discuss this with your Academic Adviser. Bank holidays are included in your annual leave allocation, therefore you should work a normal week, without an extra day off during a bank holiday week.
It is not acceptable to swap days off unless in an emergency as this will affect planned practice supervision and therefore your assessment. If you are having any difficulties in practice you should speak to your Academic Advisor.
It is not acceptable for you to use the days allocated for practice for other purposes such as completing assignments or attending academic tutorials – unless confirmed in writing by the Academic Adviser. Time is allocated for these activities during the study days.
Further guidance and support about working shifts can be found on Blackboard within the Practice Learning Gateway.
You are expected to attend all practice days. Any time missed will need to be made up due to statutes concerning midwifery education which dictate the length of education and training that each student must undertake in order to be eligible to register as a midwife.
Further guidance about the attendance regulations for this programme can be found later in this handbook. Non-attendance due to paid employment commitments is considered to be un-authorised absence and will be responded to in accordance with the programme policy.
Any changes to allocated off duty can only be authorised by the student’s Practice Supervisor / Practice Assessor who may ask for an explanation. Swapping of shifts/practice weeks to make up for sickness or absence or to change holiday weeks is not permitted. Amendments to allocations can only be made by the Allocations Officer. Additional shifts may be planned with your Practice Supervisor to help you make up missed practice time – see the making up time policy available on Blackboard within the Practice Learning Gateway.
Online Timesheets in PARE are used for recording attendance in practice. These are completed by the student and signed by the Practice Supervisor(s) on a daily basis. These completed timesheets are required as evidence of meeting the 100% attendance requirements of the programme. If these are not complete at the end of each semester it may prevent progression to the following semester. Students are strongly advised to get their timesheet signed each shift as it is difficult for Practice Supervisors to remember what shifts you worked once the learning experience has been completed. Practice Supervisor(s) may refuse to sign old timesheets so you may need to work those hours again.
Any sickness or absence during your learning experience must be reported to the placement and noted in your online timesheet in PARE. You should also notify your academic adviser of any sickness or absence affecting your attendance.
When you are on a practice learning experience, you remain a registered student of The University of Manchester and will continue to be governed by The University of Manchester’s Rules and Regulations. You should also abide by any relevant learning environment area rules and regulations.
CAR INSURANCE
Please note that when undertaking learning experiences, students may invalidate their car insurance if they make journeys after their arrival on duty as this may be considered to be using your vehicle for work purposes. Many insurance companies will allow policy holders to travel between different places of work without it being classed as business use. Any car use during the working date other than to travel to or from your work base could be considered as business use, so any such use should be checked with insurers.
4. STUDENT PROGRESSION
ATTENDANCE REQUIREMENTS
In keeping with Regulation XX – Monitoring Attendance and Wellbeing of Students, the University records and monitors your attendance to:
- Support academic attainment and progression;
- Ensure student wellbeing; and
- Satisfy external reporting/accreditation requirements.
As a student on the BMidwif/MMidwif programme you are required to complete both theoretical and practice-based learning. In accordance with the NMC standards governing our current programme, you will need to complete the whole programme which totals 4600 hours of learning over the course of the BMidwif programme or 5468 hours learning over the course of the MMidwif programme, 50% of which takes place in practice (NMC, 2019).
You are expected to engage fully with all theory and practice components of the programme. This includes attending/completing 100% of University timetabled teaching activities (synchronous and asynchronous lectures, seminars, skills teaching, Academic Adviser meetings, etc.), practice hours for each clinical placement, and completing independent study as indicated on the timetable.
Students cannot have more than 150 hours of practice learning outstanding at the end of one part / academic year of the programme. Students having less than 150 hours outstanding will be noted at the September Exam Board and be given retrieval opportunities to complete their hours and/or practice learning outcomes prior to a final board in late November/early December. Students who have amassed more than 150 hours of practice learning outstanding will be reviewed and may be required to interrupt the programme and recommence at a later date subject to eligibility to resit.
A full version of the BMidwif/MMidwif attendance policy as approved by the programme committee is available in Midwifery Gateway on Blackboard.
Reporting Absence
It is important that you are aware of attendance expectations and keep the Division appropriately informed of any issues affecting your ability to attend either theory or practice. If you are unable to attend you must notify the Division at the start of your period of absence. This should be done by emailing your academic adviser in all circumstances, explaining the reason for the absence (for example, sickness or caring responsibilities for dependents). If you are absent from theory learning, you must also inform the session lead(s) by email, so that you can also enquire how you can make up the missed learning. If you are absent from practice learning you must also let your Practice Supervisor / Assessor or the clinical learning environment know, by telephone (and contact the Practice Education Facilitation team as well). Please see the Absence flow chart in Appendix 2.
The Division differentiates between authorised and unauthorised absence from the programme. Absence from the programme can be authorised in advance due to documented sickness, or by an Academic Adviser or Year Lead for other reasons. Please note that due to NMC regulations, all absences including authorised absences must be made up in order to complete the programme.
Absences due to sickness of between 1 and 7 days can be self-certified. Sickness absences of more than 7 days require a doctor’s note. Please supply this information to your Academic Advisor. Absences due to other reasons such as carers leave, compassionate leave or attendance at an interview or conference can be authorised by an Academic Adviser who will complete an authorised absence form which is submitted to the Programme Director.
Attendance Monitoring
Due to the professional nature of the course there is a 100% attendance expectation. Any learning missed must be made up in order to meet the requirements of the NMC. Students who engage well with the learning materials and opportunities provided tend to do well in their studies and their professional development.
In accordance with the ‘Monitoring Attendance, Engagement and Wellbeing of Students’ (UoM 2021), the programme has a policy of recording, monitoring and responding to attendance and engagement issues, with the aim of assisting students to access appropriate support with issues affecting welfare and attendance so they are able to meet the attendance requirements of the programme or to recognise when this is not achievable.
In line with the University policy, if a student does not manage to comply with the required steps to improve their attendance, the Examination Board may refuse them permission to proceed on their programme. The student would have the right to appeal any such decision and would be notified of the timeframe for this process.
Attendance at all synchronous (or live) theory sessions will be monitored, including face-to face and online teaching. It is your responsibility to ensure that you accurately and honestly register your attendance.
Do not sign anyone else in on the register or share any attendance monitoring codes and do not request a friend to sign you in or record attendance when not present. All of these actions contravene the NMC Code for Professional standards of practice and behaviour for nurses, midwives and nursing associates (NMC 2018). See standards 10.1, 10.3, 10.4, 20.2. The programme team will take action in these circumstances. This may be considered evidence of fraudulent documentation and dishonesty and can result in a Fitness to Practice Committee Referral and even discontinuation from the programme.
If you are sometimes struggling to attend the taught sessions, please seek support and discuss this with your academic advisor.
It is your professional responsibility to complete all asynchronous (or not live) theory sessions, such as online activities, pre-recorded lectures, and guided reading. These are timetabled to assist you in pacing your studies and to help you prepare for future live theory sessions, simulation, or assessments, hence it is strongly recommended that you complete them on the day they are set.
Engagement with asynchronous activities and the unit overall may be periodically monitored via quizzes or online tasks.
Any theory session that is missed needs to be completed through private study. Some sessions cannot be made up via the missed teaching process. You will be advised about other options for catching up this missed learning opportunity.
On practice days, you must report your absences to the Trust and your Academic Advisor, irrespective of plans for the time to be made up.
Logging and evidencing made-up missed teaching
For the occasional times that you miss theory or teaching sessions, this needs to be made up to adhere to the NMC requirement. For most sessions you can do this by locating and watching the podcast video that was recorded live. Take careful notes from the recording to enhance your learning and as evidence that you have made the session up. Please keep these notes somewhere safe and easy to find, so that you can provide it to your AA when asked to update your theory ‘attendance’ record. We recommend using the ‘Logging missed teaching and attendance’ template to record your missed teaching and support you to find evidence of making it up.
There will be some teaching sessions that are not recorded, such as seminars, skills sessions or conference days. For these sessions, please ask the unit lead if and how you can make these up. If the unit lead tells you these cannot be made up, this will be because the important element of the learning came from being present and engaging live – such as discussion or group work. In these cases, you will have the opportunity to off-set these missed sessions with other relevant learning.
Please keep evidence of these experiences such as these to share with your AA – evidence can include notes or certificates of attendance:
- e-Learning (additional to those set in the Programme)
- Webinars
- Conferences
- PASS leader training & leading PASS sessions
- Representation at meetings as a student midwife
- Peer teaching opportunities
Please note: this is for occasional missed teaching due to illness or other unavoidable absence. Non-engagement in teaching will be monitored and reviewed, and may result in sanctions such as not having the opportunity to attempt the assessment. If you are struggling with attendance or engagement with any aspect of the programme please contact your AA, Programme Director and/or Student Support and Wellbeing.
Making up time missed due to sickness and absence
As completion of the whole programme is required, students who have outstanding theory or practice attendance requirements at the end of the final year will need to continue on the programme until all hours (theory & practice) have been completed. The student will need to arrange funding to support them during this extra time, with support. Students will be encouraged to make up missed time within each academic year to avoid building up a large amount.
Any absences from the course must be made up prior to registration as a midwife. There are two ways this time may be made up. These are:
- Making up a missed university day through private study to demonstrate achievement
of the learning outcomes is at the discretion of the unit lead. Some theoretical sessions
missed can only be made up by attendance at a later session on the same topic. - You may make up missed clinical practice hours using the guidance in the Making up
Time in Practice policy that can be found on the Practice Learning Gateway within
Blackboard.
If you have sickness / absence time to make up, you should bear this in mind when planning holidays at the end of the course. It is the normal policy that you must make up your time before you take your final weeks of holiday. However, if you have a lot of time to make up you may be allowed to take your holidays before you make up your missed time.
Consequences and sanctions
Further information can be found within the SHS handbook here.
PROGRAMME INTERRUPTIONS AND WITHDRAWALS
It is the expectation that you will pursue your studies on the BMidwif (Hons) or MMidwif programme on a continuous basis for the duration of your programme, and complete within 3 or 4 years of commencement, respectively.
If you are experiencing uncertainty about your position on the programme should contact your Academic Adviser for advice and support in the first instance. The Programme Director or Senior Academic Adviser are also able to offer you support.
Further information can be found within the SHS handbook for Interruptions and Withdrawals.
Policy for Pregnant Students
If you become aware that you are pregnant you should initially inform your Academic Advisor. You should arrange to meet with your Academic Advisor to secure a referral to Occupational Health and to discuss your plans for maternity leave. You should also examine with them the implications for your studies in relation to sharing information with clinical colleagues if on placement and also the need to secure a formally agreed authorised absence from your studies via the interruptions policy as extant within undergraduate programmes.
In all instances you are required to inform the School of your pregnancy and to secure an appointment with Occupational Health to ensure that all necessary support mechanisms and reasonable adjustments are in place to protect yourself, especially in relation to risk associated with COVID infection.
Prior to any period of interruption you will need to meet your Programme Director and Academic Advisor to formalise and agree the interruption. At this interview you should complete a Request for Interruption Form and agree the date of interruption and a provisional return date. It is your responsibility to contact the school 15 weeks prior to your return to confirm your intentions.
You are required to provide the University with some form of confirmation of the pregnancy before commencing maternity leave, for example, a MATB1 form, which is available from a GP or midwife. This form is usually provided once a pregnancy has been established for 20 weeks.
If you are in receipt of the Learning Support Fund (LSF) – Training Grant, Parental Support and Exceptional Support Fund – you may be considered for continued payment up to the last date of the payment term in which you began your authorised period of leave. There are 3 terms in the LSF payment year; November, March and May. No further LSF payments will be made until you return to the programme.
Please self-refer to Occupational Health in the first instance if you experience any problems with your pregnancy that you feel impacts on your programme of study.
Pregnant Students and Practice Placements
For students engaging in clinical practice a Risk Assessment will be required:
Students must inform the placement manager of their pregnancy on each placement so that a risk assessment specific to the area can be undertaken and recorded. Likely areas to be considered may include:
- Participation in manual handling procedures
- Exposure to radiotherapeutic investigations
- Sequencing and length of shift patterns
- Exposure to infectious disease
- Working in Theatres
- Preparation and administration of cytotoxic chemotherapeutic agents
- Exposure to hazardous waste
- Provision of Uniforms
- Access to rest areas
- Students who are non-responders to Hepatitis B vaccination, may require restrictions to practice based on risk assessment.
Students Returning to Study
You will be informed that you must take at least two weeks compulsory leave following birth by law: Pregnancy and Maternity Rights.
It is your responsibility to contact the school 15 weeks prior to your return to confirm your intentions.
You will be required to have a review with Occupational Health prior to your return to secure clearances to recommence your programme of study.
BMidwif policy regarding interruptions.
The University policy is that students can normally interrupt their degree studies for 1 year. In line with this, the BMidwif programme normally agrees an interruption for up to one year when requested by the student or required for progression reasons. However due to the demanding nature of the programme involving placement attendance as well as theoretical study, we are willing to allow students to apply to extend their interruption for a 2nd period (so interrupting for a further 12months), to help them overcome their personal difficulties and hopefully be able to return to study and practice at the appropriate point in the programme. An individualised plan for return from interruption will be developed with the student at the point of interruption and will then be reviewed several weeks before the student actually returns, to confirm the appropriateness of the plan in the light of their circumstances and learning & assessment needs at that time.
This limit of 2 years of interruption is to ensure that the student’s learning remains current so that they can provide safe and effective care for service users by drawing on their up-to-date knowledge and skills for midwifery practice. For this reason, a request for a 2nd year of interruption in the later stages of the programme may not be agreed, as the programme team need to be confident that the student is ready for clinical practice as a qualified midwife at the point of completion.
A limit of 2 years interruption will normally be applied to all interruption requests. In unusual circumstances, exceptions to this rule may be considered at the discretion of the Programme Director & Lead Midwife for Education. These circumstances will usually relate to the delivery of the programme such as major changes to the curriculum or the availability of placements.
Interruption by Student Request
If you feel that you would benefit from a leave of absence from the programme for any reason, you should initially discuss this with your Academic Adviser. You are encouraged to be proactive in accessing support, advice and guidance from your Academic Adviser, Year/Field Lead, Occupational Health, the Disability Support Office and Student Support Office as may be beneficial.
Formal requests for interruption are made by meeting with your Programme Director or Cohort/ Year Lead (or their acting deputy) to complete an Interruption Request Form (Appendix 1). If you are requesting interruption you should provide third-party evidence of your circumstances to enable the programme to fully consider whether an interruption is the best course of action for the you. Documentation submitted in support of an interruption may be shared with the Examinations Office in order to apply the mitigation circumstances policy to assessments affected by the circumstances leading to your interruption. Once used, evidence will be treated confidentially and kept on your file.
As the interruption meeting will include advice and guidance on the practicalities of interrupting and a personalised return plan it is anticipated that the request form would be completed during the meeting. In exceptional circumstances only this may be completed remotely. Final approval will be confirmed in the interruption letter which you should receive within 5 working days of the meeting.
As stated above support and guidance on the interruptions process is available via a number of means including Programme Directors, Academic Adviser, Student Support and Cohort/Year Leads. It is important to ensure that all cases for interruptions are dealt with in an efficient and proactive manner as future tuition fee and bursary funding may be affected.
Interruption by Divisional Committee
In rare cases, the Division may require a student to interrupt your programme. You would normally interrupt the programme as soon as it became apparent that either:
- You are in breach of the professional progression requirements of your programme
- You are not fit for study on the recommendation of Occupational Health or the Fitness to Study Committee
- You have failed to meet the attendance requirement of your programme as detailed in the relevant programme handbook
- The Programme Director judges that you will be unlikely to be able to meet the professional progression requirements and it in your best interest to commence a period of interruption immediately
This regulation is designed to protect you by minimising the amount of time that students repeat, which will impact you future funding.
Financial Support
Such a change in circumstances may have implications for your student finance and accommodation so we strongly recommend that you contact your Student Finance company and the University’s Student Services Centre – further information can be found here.
If you are in receipt of a student loan it is your responsibility to contact Student Finance UK to suspend your student loan.
Tuition Fees
If you receive a tuition fee loan from Student Finance, the amount you borrow depends on the date you interrupted, please see further details here.
You will not be charged fees during your interruption. If you are self-funding, and have overpaid fees i.e. for a period longer than your interruption date, you can request a refund or have the portion saved for next year – further information can be found here.
Student Finance Maintenance Loans:
We will inform Student Finance that you have interrupted your studies. They will recalculate your entitlement of maintenance loan and grant based on the date you last attended. This could mean that you have received more than entitled to, and they will ask you to pay back any overpayment of maintenance grant. Student Finance may pay up to 60 days sick pay in any one academic year where students interrupt for health reasons but payment post-interruption is at their discretion. If you have interrupted for health reasons, with your permission, we can inform Student Finance and they may pay an additional discretionary 60 days allowance of funding. More information can be found on the Money Advice Team Fact Sheets: https://www.studentsupport.manchester.ac.uk/finances/a-z/
The Learning Support Fund (LSF)
If you are entitled to funding from the LSF, the programme administration will them that you have interrupted your studies. They will recalculate your entitlement of Training Grant and Parental Allowance based on the date you last attended. This could mean that you have received more than entitled to, and they will ask you to pay back any overpayment of maintenance grant. You may submit any outstanding claims for travel and Dual Accommodation Expenses that were accrued prior to interruption within 6 months of the date they were incurred.
Access:
As you are not a registered student, your access to University premises will be the same as a member of the public; you will lose onsite IT and library access. However, you will retain access to My Manchester, your student email account and the Careers Service. You will lose access to some resources in Blackboard so download any materials that you will need. You can access:
Lecture podcasts via https://video.manchester.ac.uk/lectures
Blackboard archives via http://online.manchester.ac.uk/
Visa: UKVI will be notified of your interruption and your visa will be cancelled; you will need to return home within 60 days. If you need advice about the implications your interruption will have on your immigration status, please contact the Student Immigration Team at the Student Services Centre (contact details below).
Student Finance: If your return date is in the next academic year, Student Finance will not automatically carry over your loans so ensure you re-apply.
If you interrupted for health reasons: Before you return, you must submit evidence from a medical professional that you are now well enough to resume your studies. We may refer you to the University Occupational Health department so this can be confirmed and we will arrange this before your return date. We will also arrange for you to meet with the Senior Adviser to discuss ongoing health needs. We may also refer you to the Disability Advisement and Support Service (if you are not already registered with them) if your condition is ongoing.
Under our regulations, long-term conditions will not normally be considered by the Faculty more than once. This means that you are unlikely to be able to apply for mitigation for the same reasons in the future unless there is a major change or exacerbation in your situation.
Literature Review/Project: We will try to maintain your supervisor; if this is not possible, we will assign a new supervisor or look for a similar subject area or project type if you have not yet commenced this unit.
Visa: Please email supportoffice.sbs@manchester.ac.uk 2-3 months before your return date to request a new CAS.
JURY SERVICE
There is a possibility that you may be approached to fulfil this service during your time as a student. Although we acknowledge this experience might well be beneficial to your understanding of the legal system, the possibility that the commitment may extend beyond two weeks is a very real one and as such would interfere markedly with the continuity of the theoretical and clinical experience.
Those who administer Jury Service sometimes allow students in full-time education, including students of nursing / midwifery, to defer of the service. If you are asked to do Jury Service we do have a standard letter which can be sent on your behalf, explaining your current position as a student. Please contact the programme team to ask for a letter requesting exemption from jury service.
THE UNIVERSITY AND SECONDING EMPLOYERS
Students who are seconded to the University from their employer for a programme of study should note the following:
The University will not routinely share information about student progress and attendance with seconding employers. However, circumstances may arise where it is appropriate for information held by the University or the employer, which may affect student progression and continuation on programmes of study or employer support, to be shared between these parties. The University will respond to reasonable requests by employers for such information and may on occasion seek information from employers. Agreement to the sharing of such information for seconded students is a pre-requisite for entry and continuation on programmes of study. Students who wish to be excluded from this agreement should formally notify the Programme Director in writing, who will relay this information to the seconding employer.
INDIVIDUAL PROGRESS AND DEVELOPMENT REVIEW
All students should be offered opportunities to meet with their Academic Adviser, three times during the first semester of their programme and twice in each subsequent semester. Where extended terms operate in the second semester, an additional Academic Adviser session should be arranged. During this meeting issues to be discussed may include:
- Student’s study progress and requirements
- Any supervision and guidance that the student may require
- Placements
- Expectations of the programme
- Attitudes
- Any other items that either the student or the tutor may wish to raise, or
- Particular issues that may be relevant to the continuing success of the student
A summary will be made of the meeting, to be signed yourself and your Academic Adviser, which will then be inserted into your file.
ACADEMIC AWARD & CLASSIFICATION
Following the successful completion of full time study on the programme and the required course units The University of Manchester will award: A Bachelor of Midwifery (Hons) degree, or A Master of Midwifery degree
Degree Classification
BMidwif:
Classification of the BMidwif (Hons) degree awarded will be determined from the marks achieved by the student in all the theoretical and practice-based assessments for level 5 and 6 units. Students must accrue 360 credits in total to be awarded an honours degree (120 credits at level 4, 120 credits at level 5 and 120 credits at level 6). The weighting given to the marks gained within each unit is in proportion to the credit weighting of the unit. The calculation of the classification shall be weighted as follows:
- Year 1 (L4) – 0, Year 2 (L5) – 0.33, Year 3 (L6) – 0.67.
The degree classification is then worked out according to the table below.
Honours Degree Classification:
| I | 70%+ | |
| II(i) | 60-69% | |
| II(ii) | 50-59% | |
| III | 40-49% | |
| Fail | <40% |
MMidwif:
Classification of the MMidwif degree awarded will be determined from the marks achieved by the student in all the theoretical and practice-based assessments for level 5, 6 and 7 units. Students must accrue 480 credits in total to be awarded an honours degree (120 credits at level 4, 120 credits at level 5, 120 credits at level 6, and 120 credits at level 7). The weighting given to the marks gained within each unit is in proportion to the credit weighting of the unit. The calculation of the classification shall be weighted as follows:
- Year 1 (L4) – 0.0, Year 2 (L5) – 0.2, Year 3 (L6) – 0.4 and Year 4 (L7) – 0.4.
Professional Registration as a midwife with the NMC
On successful completion of the programme you will be eligible to register as a midwife with the NMC. In this case successful completion of the programme includes the following:
- Successful completion of all theoretical and practical assessments
- Successful completion of all proficiencies
- Successful completion of all Statutory Clinical Experiences as determined by the NMC
- Completion of all attendance requirements
- Completion of MORA
In order to graduate, you must at least have met the requirements for the relevant academic award, BMidwif (Hons) Degree (360 credits) or MMidwif degree (480 credits).
A personal identifying number will be allocated to each student prior to completion of the course. This number does not permit you to work as a Midwife in any capacity and is purely for communication with the NMC. Details of this will be sent out to you by e-mail. It is the student’s responsibility to ensure that all personal details held on record are correct.
Following ratification of final results at the Awarding Examination Board details of students who have successfully completed the course will be forwarded to the Nursing and Midwifery Council. A Declaration of Good Health and Good Character is signed by the Lead Midwife for Education (or their nominee) and sent to the NMC. The School will receive confirmation that this information has been safely received.
Each student will normally receive a registration pack from the NMC within two weeks of completion information being sent from the School. To be entered on the register, the NMC must have received a completed registration pack from the student and the Declaration of Good Health and Good Character from the School.
It is important that you apply to register with the NMC within five years of your completion date or you will not be able to register with them (NMC, 2019). If you do not register your qualification within five years, you may have to complete a pre-registration programme again. You may apply for jobs before your registration is live but you must be aware that any employment offer will be subject to successful registration. It is the student’s responsibility to liaise with their prospective employer if there is any known delay to registration. Failure to do this may jeopardise your offer of employment.
Non-Completion of the MMidwif Programme
If you elect to undertake the MMidwif, but are unsuccessful at level 7, you will still have the opportunity to qualify for the BMidwif, with eligibility to register with the NMC.
BMidwif (Hons) with eligibility for Professional Registration with the NMC (for those originally intending the MMidwif but do not continue to L7)
Learners must achieve a minimum of 360 credits, which includes 120 credits at each QAA FHEQ levels 4–6. Professional registration as a midwife is only possible when all theory and practice hours are complete (minimum 4600 hours, 50% theory and 50% practice) and all clinical proficiencies are achieved at the end of the third year, level 6. This will necessitate an additional 166 hours each theory and practice to make up the difference between the MMidwif route and the BMidwif route in year 3. Practice hours and achievement of all clinical proficiencies must be demonstrated and theory hours can be achieved through completion of the extra theory delivered on the BMidwif route.
Learners completing the BMidwif programme of study with 300 credits (60 of which must be at level 6) and who do not complete a unit of study, the practice assessments or hours of study required for professional registration as a midwife will exit the programme with a non-practice award of “BSc Healthcare Studies (Maternal and Fetal)” and will not be able to register with the NMC to practise midwifery.
Students completing the programme of study with 240 credits and who do not complete any level 6 credits may be able to exit the programme with a Diploma in Healthcare Studies (Maternal and Fetal).
Students completing the programme of study with 120 credits and who do not complete any level 5 and 6 credits may be able to exit the programme with a Certificate in Healthcare Studies (Maternal and Fetal).
5. BEHAVIOUR & PROFESSIONAL CONDUCT
Information can be found in the SHS handbook here.
Fitness to Practice
A Fitness to Practice Committee may decide to prevent students from proceeding to the next year of study if:
- the student has not behaved in accordance with the principles of the NMC The Code: Professional standards of practice and behaviour for nurses and midwives1 or
- the student’s health would prevent them from fulfilling the NMC’s The Code: Professional standards of practice and behaviour for nurses and midwives6
- the student does not uphold the NMC’s The Code: Professional standards of practice and behaviour for nurses and midwives6
Further information can be found in the SHS handbook here.
Professional Conduct
If, during the programme you receive any police convictions, cautions or “bind-overs” you should discuss this immediately with your Academic Adviser for support and guidance. You will also be asked to complete the on-line good health and good character form each year.
Further information can be found within the SHS handbook here (including the Nursing & Midwifery Council guidance).
STUDENT UNIFORM POLICY
Introduction
Wearing a uniform is essential to project a smart, professional image in the workplace. Nursing and Midwifery students of the University of Manchester are required to be well presented at all times in the clinical area. They are not only representing their profession, but also the University. Patients and clients can be assured of your commitment to best practice in infection prevention and control if your uniform is clean and you dress according to appropriate standards.
Most Trusts that you are likely to work in will have their own uniform or dress code and you are required to strictly adhere to those policies, in addition to the Division’s policy.
The policy below (and available on Blackboard) applies to all Nursing and Midwifery students who undertake placements organised by the Division. This policy supplements the Communication and Dress Code for Students in the Faculty of Biology, Medicine and Health at The University of Manchester.
Failure to comply with the uniform policy will be regarded as unprofessional behaviour and steps will be taken to invoke the Division’s procedure regarding discipline if necessary.
University of Manchester Student Midwife Uniform
You will be provided with a maximum of three complete sets of uniform by the University at the beginning of your programme of study as follows:
- White dress with purple trim and University Logo
Or
- White tunic with purple trim and University Logo and navy blue trousers
Replacement Uniforms
‘Alexandra’ is the only University approved supplier for University of Manchester student Nurse/Midwife uniforms.
You can purchase additional sets of uniform from the University suppliers at the same cost as paid by the University at the time of ordering.
Additional uniforms can be ordered and purchased by students from the supplier at the time of initial ‘fitting’ and any replacement/additional uniforms subsequently required can be ordered via the supplier website using the unique code you can obtain from shs.placements@manchester.ac.uk . You are responsible for the costs of any additional and/or replacement uniforms, and any additional delivery costs. Instructions for setting up your account and ordering replacement uniforms are available in the BMidwif Gateway.
You must only use the University approved supplier for any additional or replacement sets/items of uniform as these are supplied to a strict specification in line with relevant local and national guidance.
You will be provided with a University name badge bearing your full name, designation (student nurse or student midwife) and the logo of the University of Manchester. These must be worn at all times as part of the uniform in addition to any badge provided by the placement provider.
Replacement University name badges can be ordered from the Programme Support Office, G.319 Jean McFarlane Building.
Where this Policy Applies:
When in placement in clinical / community environments you must wear your University of Manchester uniform at all times whilst at the placement.
Due to the nature of work and specific patient/client groups they serve, some Trust staff will in some clinical areas wear their own clothes. In these instances, you will be required to wear your own clothes but these must be appropriate to the work environment, look clean and smart and adhere to any local policies.
Plain, appropriate clothing must be worn and no advertisement logos or slogans should be visible.
University uniform must also be worn when undertaking any clinical skills training sessions in the University or in the Trust. This includes any training undertaken in the clinical skills laboratories at the University such as moving and handling and basic life support training and update sessions.
You must not, as far as possible, wear your uniforms outside of the placement area and must change into your own clothes upon completion of a shift. When working in community you should wear a coat that covers the uniform entirely. The Department of Health advises that the public do not like to see hospital staff in uniform away from the workplace because they may perceive this as a risk to hygiene and infection control in the workplace. COVID infection control measures may also prohibit staff travelling in their uniforms.
Uniform Appearance and Care
A clean uniform must be worn for every new shift. You are responsible for washing and ironing your own uniforms. The Department of Health recommends that uniforms be washed at a minimum of 60° Celsius for at least 10 minutes which is sufficient to remove most microorganisms. Uniforms must look clean and neat at all times. If an item gets stained or damaged then a replacement must be obtained as soon as possible (see above for how to obtain replacement or additional uniforms).
Adjustments to the uniform for cultural / ethnic or religious reasons will be considered where possible but must be in line with national and local policies. In relation to the University supplied items of uniform, adjustments to sleeve length are not offered. Any student wishing to wear long sleeves for religious reasons will be required to purchase their own under garments / disposable sleeves.
Black headscarf / turban / skull cap may be worn.
The correct size of uniform must be worn and students must not wear cardigans or other over garments in the clinical areas.
Appropriate shoes must be worn. These must be black, flat, full shoes not boots, which cover the entire foot, have a non-slip rubber sole, and be plain (not suede or canvas). It is not acceptable to wear any other type of shoe.
Tights that are black or skin coloured only may be worn, with no embellishments. Only plain black socks may be worn.
Whilst on placements the following will also apply:
- Hair must be tidy and long hair must be tied/clipped back off the face and collar. Protruding hair decorations must not be worn. If required, neutral colour decoration should be used to secure hair.
- Long hair should be firmly tied back in such a way as not to interfere with duties or patient care.
- Beards and moustaches should be neatly trimmed.
- Fingernails should be clean, short and free of all nail polish. Acrylic nails must not be worn at any time due to the risk of infection (McNeil 2001)
- If make-up is worn, this should be discrete and false eyelashes are not acceptable. Perfumes and after-shave should be used sparingly.
- In the interest of infection control and minimising risks to the student and the patient/client NO jewellery other than small, plain stud earrings (one per ear) and one plain band ring is permitted at any time whilst wearing uniform. Wristwatches and bangles must not be worn when attending to patients.
- Any visible piercings must be removed whilst in the clinical area and / or treating patients or clients.
- Tattoos that may cause offence should be covered accordingly and should adhere to the required dress code described above.
References:
McNeil S.A, Foster C.L, Hedderwick S.A (2001) Clin Infect Dis 32:367-372 Department of Health (2007) Uniforms and Workwear. An evidence base for developing local policy. © Crown Copyright 2007 [online: (Local Uniform Policy)
CLINICAL SKILLS LABORATORY: STUDENT CONDUCT
You must follow the regulations below when using the laboratories:
- Aspx (manchester.ac.uk) (Social Networking)
- http://documents.manchester.ac.uk/display.aspx?DocID=29038 (Communication and Dress Code)
- Faculty of Medical and Human Sciences (manchester.ac.uk) (Drugs & Alcohol)
HEALTH CLEARANCE
Continuation on the programme is conditional on continued health clearance: see Occupational Health clearance.
You are expected to be proactive in managing both physical and psychological health issues and seek support from your Academic Adviser or self-refer to Occupational Health if you have any concerns about the impact of health issues on your ability to study.
It is your responsibility to attend agreed health screening, referral and immunisation appointments and specifically to securely retain the vaccination history information provided by Occupational Health at the end of the course of vaccines. Occupational Health recommends that no student commences on clinical placement until they have had an initial health screening appointment. You are encouraged to advise Occupational Health if you have any significant health related concerns that could affect your fitness to for the programme.
The programme team will be keen to support you manage any health issues. You have a professional responsibility to engage with occupational health processes in order to “maintain the level of health you need to carry out your professional role” (NMC 2018). Failure to do could result in a referral to a Fitness to Study or Fitness to Practice Committee.
Crisis counselling is provided by the Universities Counselling service however Occupational Health can offer support and advice with regards fitness to return to the programme.
Occupational Health will advise the Division if you do not attend a formal appointment and this may impact your progression.
Please note that the Universities Counselling and Mental Health services offer confidential help with any personal issues affecting work, self-esteem, relationships, sexuality, mental health and general well-being. See also: https://www.counsellingservice.manchester.ac.uk/.
If you have a disability or an issue such as Dyslexia, Dyspraxia, Dyscalculia then the Disability Advisory & Support Service [DASS] would welcome you registering for advice and additional support. See also: https://www.dass.manchester.ac.uk/
GOOD HEALTH AND GOOD CHARACTER
You must declare any criminal convictions, cautions, reprimands or warnings received (either in this country or overseas) that may call into question your good character as soon as possible, as this may impact your continuation on the programme. For each year of your studies, you will be required to complete an annual self-declaration of Good Health & Good Character confirming your continued good character.
PART-TIME EMPLOYMENT
You are advised to think carefully about how you will balance work in theory and practice against the demands of part-time employment and to limit any hours they work accordingly. The Division is not able to provide character references for part-time employment undertaken during a programme of study, but will provide details of your programme of study.
If however you do have a part-time job in a particular clinical area, please inform the allocations department. We recommend that you do not have a clinical placement in the same area as your part-time job, due to the conflict of interests which may arise.
UNIT EVALUATIONS
Since we are encouraging you to develop your willingness and ability to ask searching questions about midwifery practice, we expect you to offer equally appropriate criticisms of our work in midwifery education. In this respect, we agree to accept your evaluation of our work. You, as new midwives, carry forward our aspirations, and you will help to assure the on-going development of midwifery education.
6. STUDENT SUPPORT
Support from the University
As a student at the University of Manchester, you have access to a huge range of support services and resources. This includes, but is not limited to, support relating to your studies, finances, health and wellbeing, settling in and making friends, personal safety and planning for your future beyond University.
You can access the SHS handbook here.
PEER ASSISTED STUDY SESSIONS (PASS) AND PEER MENTORING
All first year students are placed in a PASS group – Further information can be found within the SHS handbook here.
PASS leaders will introduce themselves to their group through activities in Welcome Week and continue to support their group throughout the academic year in a series of compulsory timetabled sessions. The PASS leaders are supported by the Student Support Manager and the Year 1 lead.
Optional peer mentoring groups for year 2 students may be offered by 3rd year students in Semester 1 to support the 2nd year students as they settle into year 2 and adjust to their new NHS Trust sites.
7. LEARNING RESOURCES
LIBRARY FACILITIES
Further information can be found within the SHS handbook here.
Getting Started
There is a subject guide for Nursing and Midwifery students giving all of the latest information on resources and services available to you. This is a good starting point if you are looking for any library resources or information related to your course.
IT FACILITIES
University Computer Facilities
Further information can be found within the SHS handbook here.
Divisional Computer Facilities
Computing facilities for the Division are available on the 2nd floor of the Jean McFarlane Building.
The facilities provided have healthcare specific applications and there are 40 computers. Students can access the full range of online resources available including Blackboard and the University Library electronic resources.
Printing has to be paid for, via print credits purchased from the Manchester Computing Shop or print robots situated around the University’s campus.
Access to the computers is via a standard University username which is obtained from any of the main campus computers displaying the standard log in screen or from the registration computers at Jean McFarlane Building, by answering the questions when prompted students can gain access to and receive their username and password. This will enable them to use any of the computers to which any student has access.
STUDY SKILLS
Each student will start their programme with a mix of different skills. We have identified a number of Study Skills that are vital for you to master early in your study, in order to achieve your full potential on the programme. These include academic writing, Harvard Referencing, Using IT software, Numeric and Literature skills.
Each programme of study will provide an introduction to relevant study skills during enrolment. In the BMidwif, these are part of the Professional Midwifery Unit with relevant activities located on Blackboard. You are also strongly advised to access the ‘My Learning Essentials’ resources via the library website. These offer a wind range of resources and workshops to help you develop your skills. If you feel that you may have a learning disability further assistance may be available, please see your Academic Adviser or the Disability Support Officer.
SOCIAL & WORKING SPACES FOR STUDENTS
The Jean McFarlane Building has a central atrium which provides comfortable and flexible spaces for students to meet or work. Wi-Fi is available in the atrium.
Work spaces may also be booked via the Library and within the Alan Gilbert Learning Commons building. There are many computer clusters available for use across the campus.
The use of all these facilities may be restricted depending on government and university guidance regarding the COVID pandemic.
8. APPENDICES
APPENDIX 1: DIVISION OF NURSING, MIDWIFERY & SOCIAL WORK
STUDENT CHARTER AND CONDITIONS OF PRACTICE EXPERIENCE
  |
Conditions of Practice Experience
As a health/social care student you will have additional responsibilities under the heading of Developing Professional Practice. These responsibilities to service providers and users are detailed in the Conditions of Practice Experience below.
You should apply the guidance given by your professional body at the links below in both your academic and practice work and behaviour:
- NMC Code of Conduct – The Code (nmc.org.uk)
- Standards of conduct, performance and ethics – nmc-old-code-2008.pdf
- Standards of Proficiency – Social Work (Standards of proficiency for registered nurses – The Nursing and Midwifery Council (nmc.org.uk) )
Developing Professional Practice
Together we will:
- be guided by the University’s and Providers’ policies and procedures
- perform all activities with guidance from and reference to the standards of professional bodies and current and relevant legislation in order for you to become a professional who is fit for award, employment and purpose
- ensure a safe environment where there is respect and dignity, and within which it is possible to raise and escalate concerns encountered during the practice experience in a timely way
- provide opportunities for you to develop your evidence base for practice where this is required
As a student I will:
- Maintain my health and good character by ensuring that I:
- attend all required Occupational Health Service appointments
- notify the Division of any situation which might result in the receipt of a police reprimand, caution or conviction
- complete the annual declaration of Good Health and Good Character
- ensure I access all learning environment information in a timely way and contact my practice experience provider before the placement begins
- engage with the activities of the learning environment under the supervision and guidance of an appropriate member of the provider’s staff
- maintain confidentiality with all forms of information I may have access to, see or hear
- ensure I present myself professionally at all times taking note of any regulations relating to uniform and personal appearance
- ensure I complete all patient/service user documentation in a timely, accurate and understandable way and obtain a staff signature where it is required to do so
- understand that my practice documentation is my responsibility and ensure it is available to practice area staff when I am there
- liaise with my Practice Assessor / Supervisor(s) to ensure that any practice experience documentation is completed in an honest, timely and appropriate way
- submit all practice documentation following University guidelines and deadlines
- engage in the assessment/feedback processes designed to support my practice development
- take part in evaluative processes which facilitate the development of practice experiences for all students take responsibility for my personal money or property whilst on Providers’ premises
- communicate appropriately with my academic assessor and academic adviser regarding any issues I am experiencing in practice and respond to requests to attend meetings regarding my progress
As a University, and in negotiation with Providers, we will ensure your practice experience:
- is prepared and audited in line with professional and University guidance
- has sufficient appropriately trained staff to support your development of practice-based skills
- is appropriate to your stage in the programme
- is communicated to you within the timeframe set out by the University
- is supported by allocations procedures to ensure your practice experiences facilitate development of your professional practice
- provides you with a supportive framework to resolve any challenges you may encounter I acknowledge that I have read the Student Charter and the Conditions of Practice Experience and agree to fulfil my role as laid out in these documents.
| Student | Academic Adviser |
| Name | Name |
| Signature | Signature |
| Date | Date |
APPENDIX 2: GUIDANCE ON MANAGING ATTENDANCE AND ABSENCE REPORTING
Making up Missed Teaching
The student must provide evidence of how they have engaged with the teaching material in order to be credited for making up what has been missed. Where possible, podcasts and recordings are available to facilitate this process.
IMPORTANT: Students must keep evidence of making up missed teaching safe and somewhere it can be easily found. Please use the ‘Logging missed teaching and attendance’ template to assist you with your responsibility here.
Sessions that cannot normally be made up through private study may include:
- Skills lab or practical sessions.
- Tutorials/seminars involving discussion and interaction
- Inter-professional learning activities involving discussion & interaction
- Special events.
Evidence should clearly indicate the session being made up, the date and nature of the session, the number of attendance hours missed and being made up and the work that has been done to catch up the missed material.
Examples of acceptable evidence include:
- Annotated PowerPoint handouts indicating that the student has listened to the podcast and engaged with the material
- Own notes relating to the topics covered in the session.
- Annotated additional reading relating to the topics covered in the session
- Completed quizzes or activities given out in the session.
The amount of evidence required should be in proportion to the length of the session. Evidence may not be accepted if the work submitted does not indicate that the student has engaged with the material, eg if the student has simply cut & pasted the lecturer’s PPT slides into a word document.
Students should aim to have all missed sessions from the academic year caught up by the end of the academic year.
Students are expected to make up missed theory time through theory-related activity. Attendance at some optional sessions or conferences can be accepted as an alternative way of making up missed theory learning – see Attendance at Conferences Policy on Nursing Gateway.
Attendance at compulsory NHS Core skills practical sessions
Some practical sessions may be identified as compulsory (ie required in order to be allowed in practice or to continue in practice). These will include sessions linked to on-line NHS Core Skills which are also compulsory. One repeat session can be arranged for those who did not attend. Failure to meet the requirements for attending placement will result in being withdrawn from placement until this can be achieved.
Students will need to seek an alternative opportunity to complete the skills session eg accessing a session in the Trust or joining a different year group or a BNurs group.
Reporting Absence
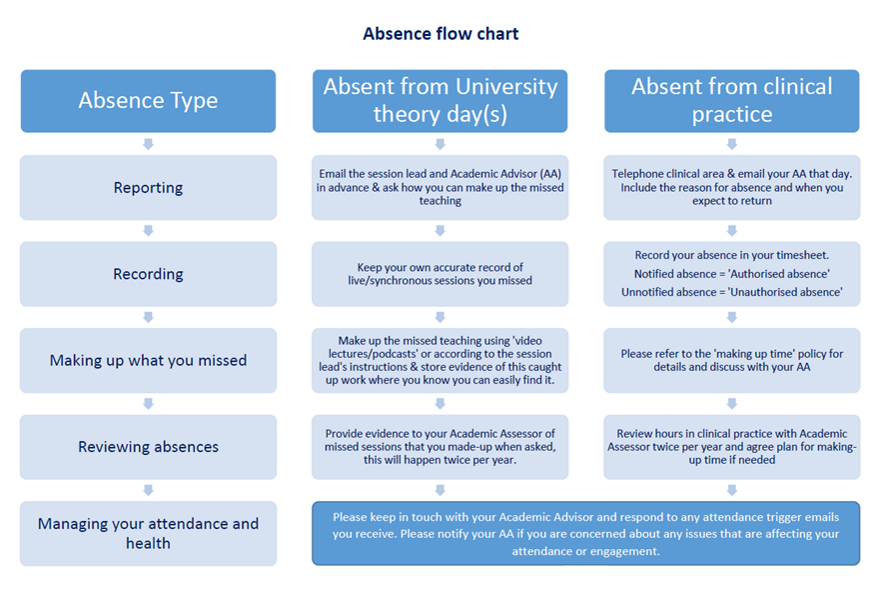
If a student has not attended either theory or practice for 4 weeks with no communication to explain their absence, they will be written to by recorded delivery, asked to clarify whether they are still on the programme and be invited to attend a meeting with their Academic Adviser and the Programme Director. If no reply is received or the student does not attend to attend a meeting with the Programme Director or their Academic Adviser, they will be referred to the Fitness to Practice / Health & Conduct Committee who may decide to discontinue them from the programme.
Monitoring attendance in practice
You should self-monitor your attendance, using the yearly overview provided each year. If you are not being given enough clinical shifts to meet these requirements, it is your responsibility to raise this with the placement team and seek support from your AA to ensure your have enough shifts. If you are falling behind in meeting your clinical hours requirements, you should discuss this with your Academic Adviser and where feasible, use the making-up practice hours policy to begin to catch up these hours so you are on track by the end of the year. Each year you should complete the required hours of practice learning, which should be documented in PARE.
| Year (part) of study | Practice hours required |
| 1 | 767 |
| 2 | 767 |
| 3 (BMidwif) | 766 |
| 3 (MMidwif) | 600 |
| 4 (MMidwif) | 600 |
Your Academic Adviser will review practice attendance at least twice a year at each progression point (Academic Assessor review). Students who are falling behind (eg 40 hours deficit) in meeting their placement hours requirements will be:
- Given an opportunity to discuss any factors making it hard for them to attend and be helped to develop an action plan to improve attendance.
- Referred to any relevant support services to assist then eg student support, occupational health, DASS or the counselling service.
- Helped to develop a Support in Practice Plan in relation to agreed reasonable adjustments if appropriate.
- Reminded of the appropriate ways to make up missed clinical hours and missed theory sessions and helped to develop an action plan to address the deficit.
- Monitored by their Academic Adviser.
Students reaching 100 hours of missed practice time without reasonable explanations about the reason for absence and no evidence of improving attendance may receive an informal warning.
Students reaching 150 hours of missed practice time (4 weeks of full-time work) without reasonable explanations about the reason for absence and no evidence of improving attendance may receive a formal warning.
Further on-going absences from practice may result in a referral to the Concerns Review Panel / Fitness to Practice / Health & Conduct Committee. Students cannot have more than 150 hours of practice learning outstanding at the end of one part / academic year of the programme. Students having less than 150 hours outstanding will be noted at the September Exam Board and be given retrieval opportunities to complete their hours and/or practice learning outcomes prior to a final board in late November/early December. Students who have amassed more than150 hours of practice learning outstanding will be reviewed and may be required to interrupt the programme and recommence at a later date subject to eligibility to resit. The requirement to interrupt is to enable students time to address the issues that are impacting on their ability to keep up with practice hours, and to avoid accrual of any further hours deficit. Following interruption, the agreed return date would take account of the hours deficit to ensure that the student has enough opportunity to complete the required hours within the programme, which may mean a return date in advance of the start of the next year.
If there are recognised factors affecting your ability to meet the attendance requirements for practice, you will be supported to maximise your attendance but may be advised to interrupt your studies and return to the programme when you are better able to meet the practice learning requirements.
You will not be able to be presented to the NMC for registration until all theory and all practice hours have been completed and documented. You may need to self-fund any making up time at the end of the programme.


